Abstract
The Wiskott-Aldrich syndrome (WAS) is a severe X-linked disorder characterized classically by thrombocytopenia, immunodeficiency, and eczema. The phenotype observed in this syndrome is caused by mutation in the WAS gene. Peripheral blood DNAs were isolated from an 18-month-old boy with WAS and his mother, maternal uncle, and maternal grandmother. Genetic analysis for the detection of a mutation of WAS gene was performed by polymerase chain reaction-single strand conformational polymorphism analysis (PCR-SSCP) and direct sequencing of the PCR product. In PCR-SSCP, the patient and his maternal uncle had an abnormal shift band, which was not found in normal controls, and his mother and maternal grandmother showed heterozygous bands. In direct sequencing analysis, the patient with WAS had CGC→CAC point mutation in exon 2 that resulted in an amino acid change in codon 86 (Arg86His). The present study identified a gene mutation responsible for WAS at a mutation hotspot of the WAS gene in a Korean family.
Wiskott-Aldrich syndrome (WAS) (Online Mendelian Inheritance in Man [OMIM] 301000) is an X-linked recessive disorder characterized by thrombocytopenia, eczema, and immunodeficiency. Clinical symptoms include petechiae, bloody diarrhea, inability to generate antibodies against polysaccharide antigens, and in some cases, autoimmune manifestations. Affected boys often die because of malignant tumors, particularly lymphoma (1, 2). Treatments for WAS include antimicrobial therapy for infections, intravenous immune globulin, splenectomy for thrombocytopenia, and allogeneic bone marrow transplantation (3-5).
The gene responsible for WAS was isolated, and designated the WAS gene (6). The gene is composed of 12 exons spanning approximately 9 kilobases. The encoded protein is a 502 amino-acid long intracellular protein, which is broadly expressed in hematopoietic cells (7). The WAS gene was found to be mutated, not only in classic WAS patients, but also in patients with X-linked thrombocytopenia (XLT), which is a clinically mild allelic variant (8, 9). Recent reports have expanded the WAS mutation phenotype to include intermittent XLT, X-linked neutropenia with or without myelodysplasia, or WAS/XLT in females with heterozygous mutations (10, 11).
Many WAS gene mutations have been reported in patients with WAS. However, little is known about Korean WAS patients in terms of their molecular genetic diagnosis. In this report, we describe a Korean family with WAS, which was diagnosed as having exon 2 mutation, based on the WAS gene mutation analysis. This is the first identified case of a hotspot mutation in exon 2 of WAS in Korea.
A one-day-old male neonate was admitted to the hospital because of jaundice and petechiae on the body. He was born after 37 weeks gestation, by Cesarean section due to breech presentation and had a birth weight of 2,800 g. Laboratory data showed a hemoglobin of 16.8 g/dL, a white blood cell count of 17,050/µL, a platelet count of 39,000/µL, and a high reticulocyte count (9.1%), but Coombs' tests were negative. The level of serum bilirubin (total/direct) was 7.3/0.4 mg/dL, and the result of the liver function test was unremarkable. Also, immunoglobulin (Ig) M titers to TORCH were negative. Serum Ig measurements at day 1 revealed an elevated Ig A level (28.8 mg/dL; normal range, 1.3-3.6) (Ig G: 1,216.8, Ig M<23.8, Ig D<1.5, and Ig E<18.0). The results of peripheral blood smear were unremarkable, except for a markedly decreased number of platelets. A bone marrow aspiration smear showed slight erythroid and megakaryocytic hypoplasia. Karyotyping analyses of both the patient and his mother were normal. A review of family history revealed his maternal uncle was clinically diagnosed as having WAS at five years of age. The patient was treated with platelet transfusion, and petechiae on the body disappeared immediately. However, the patient's thrombocytopenia persisted. When the patient was 18 months old, genetic counseling was provided at his mother's request.
Genomic DNA was isolated from peripheral blood leukocytes by using the Wizard Genomic DNA purification kit, according to the manufacturer's instructions (Promega, Madison, WI, U.S.A.). In order to examine mutations on the WAS gene, polymerase chain reaction-single strand conformational polymorphism (PCR-SSCP) was performed for all 12 coding regions of the WAS gene by using the primer sets as listed in Table 1. The PCR was performed with a thermal cycler (model 2400, Applied Biosystems, Foster City, CA, U.S.A.) as follows: 32 cycles of 1 min at 94℃ for denaturation, 1 min at 55-60℃ for annealing depending on the primers, and 1 min at 72℃ for extension. Final extension was performed at 72℃ for 10 min. The PCR products were electrophoresed on an agarose gel and stained with ethidium bromide to confirm the size of the bands. The PCR products were also denatured in formamide loading buffer and electrophoresed through 8% and 10% polyacrylamide gels. Silver stain was performed to develop bands (12). To determine the sequences of the DNA samples showing mutant bands, direct sequencing was performed on the ABI Prism 3100 Genetic Analyser (Applied Biosystems).
PCR and subsequent SSCP analysis in exon 2 of the WAS gene identified an aberrantly migrating band in the patient's mother, and in his maternal grandmother, compared to two wild type bands in the controls. The patient and his maternal uncle showed two bands, one of which was a lower wild single strand band and the other, an abnormal shifted band (Fig. 1). In the direct sequencing analysis of the PCR products for SSCP, the missense mutation was observed in the patient and his maternal uncle. This showed G-to-A transition at complementary nucleotide 257 (c.257G>A) (Fig. 2C), resulting in substitution of His for Arg at codon 86 (Arg86-His) (CGC→CAC). The patient's mother and his maternal grandmother were heterozygous for the mutation at codon 86 (Fig. 2B).
Mutations of the WAS gene result in 3 distinct phenotypes: the classic WAS triad of thrombocytopenia with small platelets, recurrent infections as a result of immunodeficiency, and eczema (1); the milder XLT variant, characterized predominantly by thromobocytopenia with small platelets (8, 9); and finally, congenital neutropenia without the clinical findings characteristic for WAS/XLT (10, 11).
As shown in WASPbase (13), a database of mutations, a total of 441 cases consisted of missense mutations in 179 cases (40.6%), deletions in 92 cases (20.9%), nonsense mutations in 64 cases (14.5%), splicing defects in 64 cases (14.5%), and insertions in 42 cases (9.5%). The exon distribution of over 5% frequency of mutation was located in exon 2 (27.0%), exon 10 (16.1%), exon 1 (13.8%), exon 4 (9.8%), exon 3 (7.5%), and exon 7 (6.4%). Notably, the frequency at codon 86 in exon 2 was 33.6% (40/119 cases). It is well known that the codon 86 of the WAS gene is the most common missense mutation site responsible for WAS/XLT (10, 13). To our knowledge, this is the first report on the hotspot missense mutation in exon 2 of WAS gene in Korea.
There are several reports on WAS mutations in Korean families (Table 2). As shown in Table 2, the predominant mutations were nonsense mutations and missense mutations (14-18). Only one small deletion was reported in exon 10 (15). In this report, we found a missense mutation in exon 2. In Korean patients' reports, including our results, mutations in exon 1, 2, 3, 7, 8, and 10 have been involved in WAS. Therefore, although it is necessary to accumulate mutation data from a large number of patients with WAS, the distribution of mutations may be highly diverse in Korean patients, as had been observed in other reports (9, 10, 13).
A correlation between clinical phenotype and genotype was reported independently by several investigators (19-21), but was not observed by all (22, 23). Imai et al. demonstrated that all WAS patients with missense mutations showed WASP-positive expression; in contrast, patients with nonsense mutations, large deletions, small deletions, and small insertions were WASP-negative expression. Patients with splicing mutations were either WASP-negative or WASP-positive. Lack of WASP expression was associated with severe clinical symptoms and poor prognosis (24). Jin et al. reported 5 mutational hotspots in the WAS gene from 227 WAS/XLT families with a total of 262 affected members. They also noted that the missense mutation at codon 86 was observed most frequently and associated with mild symptoms (25). Two previous reports (24, 25) showed that there is a strong possibility of establishing an association between genotype and phenotype. In spite of advances in the clinical treatment of WAS patients, WAS remains a life-threatening condition, resulting in a poor quality of life and a bad long-term prognosis, especially for those who lack an HLA-matched sibling. The discovery of the WAS gene, and the identification of the molecular basis of WAS, have made it possible to provide genetic counseling for at-risk families. Therefore, this report on the hotspot missense mutation in exon 2 of WAS gene, will help this patient's parent and his maternal uncle to understand WAS and plan both genetic counseling and family regulation.
Figures and Tables
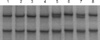 | Fig. 1Single-strand conformational polymorphism patterns for exon 2 of the WAS gene. Patient's mother and his maternal grandmother showed an extra band above upper normal single strand band in lane 5 and 7. In lane 6 and 8, patient and maternal uncle exhibited two bands, a normal lower single strand band and a mobility shift band. In lane 1-4, normal subjects showed two single strand bands. |
 | Fig. 2Sequencing identification of the missense mutation in exon 2 of the WAS gene. The asterisk (*) indicated a single base "G" to "A" substitution in the affected patient (C) compared with a normal control (A), causing replacement of arginine by histidine at the amino acid residue 86 (Arg86His). WAS exon 2 sequence in female heterozygotes (B). |
References
1. Sullivan KE, Mullen CA, Blaese RM, Winkelstein JA. A multiinstitutional survey of the Wiskott-Aldrich syndrome. J Pediat. 1994. 125:876–885.

2. Filipovich AH, Mathur A, Kamat D, Kersey JH, Shapiro RS. Lymphoproliferative disorders and other tumors complicating immunodeficiencies. Immunodeficiency. 1994. 5:91–112.
3. Mullen CA, Anderson KD, Blaese RM. Splenectomy and/or bone marrow transplantation in the management of the Wiskott-Aldrich syndrome: long-term follow-up of 62 cases. Blood. 1993. 82:2961–2966.

4. Litzman J, Jones A, Hann I, Chapel H, Strobel S, Morgan G. Intravenous immunoglobulin, splenectomy, and antibiotic prophylaxis in Wiskott-Aldrich syndrome. Arch Dis Child. 1996. 75:436–439.

5. Filipovich AH, Stone JV, Tomany SC, Ireland M, Kollman C, Pelz CJ, Casper JT, Cowan MJ, Edwards JR, Fasth A, Gale RP, Junker A, Kamani NR, Loechelt BJ, Pietryga DW, Ringden O, Vowels M, Hegland J, Williams AV, Klein JP, Sobocinski KA, Rowlings PA, Horowitz MM. Impact of donor type on outcome of bone marrow transplantation for Wiskott-Aldrich syndrome: collaborative study of the International Bone Marrow Transplant Registry and the National Marrow Donor Program. Blood. 2001. 97:1598–1603.

6. Derry JM, Ochs HD, Francke U. Isolation of a novel gene mutated in Wiskott-Aldrich syndrome. Cell. 1994. 78:635–644.

7. Stewart DM, Treiber-Held S, Kurman CC, Facchetti F, Notarangelo LD, Nelson DL. Studies of the expression of the Wiskott-Aldrich syndrome protein. J Clin Invest. 1996. 97:2627–2634.

8. Villa A, Notarangelo L, Macchi P, Mantuano E, Cavagni G, Brugnoni D, Strina D, Patrosso MC, Ramenghi U, Sacco MG, Ugazio A, Vezzoni P. X-linked thrombocytopenia and Wiskott-Aldrich syndrome are allelic diseases with mutations in the WASP gene. Nat Genet. 1995. 9:414–417.

9. Schwarz K. WASPbase: a database of WAS- and XLT-causing mutations. Immunol Today. 1996. 17:496–502.

10. Imai K, Nonoyama S, Ochs HD. WASP (Wiskott-Aldrich syndrome protein) gene mutations and phenotype. Curr Opin Allergy Clin Immunol. 2003. 3:427–436.

11. Devriendt K, Kim AS, Mathijs G, Frints SG, Schwartz M, Van Den Oord JJ, Verhoef GE, Boogaerts MA, Fryns JP, You D, Rosen MK, Vandenberghe P. Constitutively activating mutation in WASP causes X-linked severe congenital neutropenia. Nat Genet. 2001. 27:313–317.

12. Ha TW, Han KH, Son DG, Kim SP, Kim DK. Analysis of loss of heterozygosity in Korean patients with keratoacanthoma. J Korean Med Sci. 2005. 20:340–343.

13. Imai K. WASPbase. Available from:
http://homepage.mac.com/kohsukeimai/wasp/WASPbase.html.
14. Jo EK, Futatani T, Kanegane H, Kubota T, Lee YH, Jung JA, Song CH, Park JK, Nonoyama S, Miyawaki T. Mutational analysis of the WASP gene in 2 Korean families with Wiskott-Aldrich syndrome. Int J Hematol. 2003. 78:40–44.
15. Kim MK, Kim ES, Kim DS, Choi IH, Moon T, Yoon CN, Shin JS. Two novel mutations of Wiskott-Aldrich syndrome: the molecular prediction of interaction between the mutated WASP L101P with WASP-interacting protein by molecular modeling. Biochim Biophys Acta. 2004. 1690:134–140.

16. Hwang DJ, Yang JW, Kim SY, Yi HK, Lee DY, Hwang PH. Diagnostic Approach of Wiskott-Aldrich Syndrome. Korean J Pediatr. 2004. 47:726–734.
17. Baek HJ, Choi SH, Sohn KR, Kook H, Kim SJ, Song ES, Han DK, Hwang TJ. Mutation Analysis in X-linked Recessive Congenital Immunodeficiency Syndromes. Chonnam Med J. 2005. 41:48–61.
18. Kim HJ, Yoo EH, Ki CS, Yoo GH, Koo HH, Kim JW, Kim SH. A novel mutation W252X in the WAS gene in a Korean patient with Wiskott-Aldrich syndrome. Int J Hematol. 2006. 83:426–428.

19. Wengler GS, Notarangelo LD, Berardelli S, Pollonni G, Mella P, Fasth A, Ugazio AG, Parolini O. High prevalence of nonsense, frame shift, and splice-site mutations in 16 patients with full-blown Wiskott-Aldrich syndrome. Blood. 1995. 86:3648–3654.

20. Zhu Q, Watanabe C, Liu T, Hollenbaugh D, Blaese RM, Kanner SB, Aruffo A, Ochs HD. Wiskott-Aldrich syndrome/X-linked thrombocytopenia: WASP gene mutations, protein expression, and phenotype. Blood. 1997. 90:2680–2689.

21. Lemahieu V, Gastier JM, Francke U. Novel mutations in the Wiskott-Aldrich syndrome protein gene and their effects on transcriptional, translational, and clinical phenotypes. Hum Mutat. 1999. 14:54–66.

22. Greer WL, Shehabeldin A, Schulman J, Junker A, Siminovitch KA. Identification of WASP mutations, mutation hotspots and genotype-phenotype disparities in 24 patients with the Wiskott-Aldrich syndrome. Hum Genet. 1996. 98:685–690.

23. Schindelhauer D, Weiss M, Hellebrand H, Golla A, Hergersberg M, Seger R, Belohradsky BH, Meindl A. Wiskott-Aldrich syndrome: no strict genotype-phenotype correlations but clustering of missense mutations in the amino-terminal part of the WASP gene product. Hum Genet. 1996. 98:68–76.

24. Imai K, Morio T, Zhu Y, Jin Y, Itoh S, Kajiwara M, Yata J, Mizutani S, Ochs HD, Nonoyama S. Clinical course of patients with WASP gene mutations. Blood. 2004. 103:456–464.

25. Jin Y, Mazza C, Christie JR, Giliani S, Fiorini M, Mella P, Gandellini F, Stewart DM, Zhu Q, Nelson DL, Notarangelo LD, Ochs HD. Mutations of the Wiskott-Aldrich Syndrome Protein (WASP): hotspots, effect on transcription, and translation and phenotype/genotype correlation. Blood. 2004. 104:4010–4019.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download