Abstract
The aims of this study were to summarize results on the association of HLA-DRB1 with rheumatoid arthritis (RA) in Asians and to determine if the shared epitope (SE) hypothesis could explain the meta-analysis results. Among the papers published between January 1987 and July 2006 on RA susceptibility in Asian-Mongoloid populations (Korean, Japanese, Chinese, and Thai), 12 were selected for the meta-analysis. Mongoloid-Asian patients with RA had significantly higher frequencies of HLA-DRB1*0101, *0401, *0410, and *1001 than controls (OR 1.5-2.1, p<0.05 for association). When analyses were restricted to more ethnically homogeneous populations, HLA-DRB1*0405 showed a significant susceptibility to RA in Koreans (OR 5.65, 95% CI 4.32-7.39), whereas the HLA-DRB1*0301, *0403, *0406, *0701, *1301, and *1405 alleles showed protective association with RA (OR 0.32-0.70, p<0.05 for association). In conclusion, it was found that HLA-DRB1 *0101, *0401, *0405, *0410, and *1001 are susceptible, while HLA-DRB1*0301, *0403, *0406, *0701, *1301, and *1405 are protective in Asian-Mongoloids. All the RA-associated alleles except DRB1*0301 could be explained by the structural model supporting the SE hypothesis that RA susceptibility is determined by the combination of amino acid residues at HLA-DR β71 and β74, not by β71 alone.
Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by chronic inflammation of the joints, which may lead to joint destruction and disability. The prevalence of RA is about 1% of the population worldwide, and genetic factors have been estimated to account for 60% of the disease risk (1). Genetic variation is believed to be important in determining both the susceptibility to and severity of RA, with the strongest association being observed in the HLA region, in particular, with HLA-DRB1 alleles (1). The shared epitope (SE) hypothesis has been proposed to explain susceptibility to RA, based on the observation that HLA-DR specificities associated with the disease share a similar amino acid sequence in the third hypervariable region of the HLA-DRB1 molecule (2, 3). Many studies have attempted to clarify this relationship, but there has been no definite consensus to date (4). Differences in results may be related to the ethnic and clinical heterogeneity of the patients studied or to the relatively small numbers of patients in each study.
Meta-analysis is one way to overcome the problems of small sample size and inconsistent results. Combining the results from several studies can achieve greater statistical power. Well-designed meta-analyses of Caucasian and Native American populations have provided evidence showing a strong association between HLA-DRB1 and RA susceptibility and severity (4, 5). To date, however, there have been no meta-analyses on other ethnic groups, especially for Asian-Mongoloid populations. Individual studies have reported different results regarding the association of HLA alleles with RA. For example, some have reported that the frequency of the HLA-DRB1 *0101 and *0401 alleles are significantly increased in RA patients, whereas others have found no associations (6-9). Therefore, we performed a meta-analysis on the association between HLA and RA in Asian-Mongoloid population.
We searched Pubmed and EMBase using the keywords 'human leukocyte antigen' and 'rheumatoid arthritis' for all English language articles published between 1 January 1987 and 31 July 2006. The start time was based on the introduction of molecular DRB1 typing in 1987 (10). We also included studies referenced in any articles selected.
One reviewer evaluated the materials and methods section of all identified articles, and selected only those that met all the inclusion criteria as follows: 1) HLA-DRB1 alleles were molecularly typed (high resolution level), 2) controls and RA patients were Asian-Mongoloid populations, and 3) materials and methods were well-described and reliable. Although assessment of study quality is considered important for systematic reviews and meta-analyses, scoring methods have been considered problematic (11) and may not accurately assess the quality measures of interest (12). Therefore, we used reliability of patient selection, molecular typing method, and statistical analysis method as quality variables.
HLA-DRB1 alleles were considered only when they were typed in at least 2 independent studies. The frequency of HLA-DRB1 alleles varies according to ethnic and racial background, with some alleles being extremely rare. Therefore, articles were not required to identify all alleles for inclusion.
Comparisons of allele frequencies between patients and controls were made using the Z test (13) and summary odds ratios (ORs) with 95% confidence intervals (CIs). Summary ORs were computed using fixed effects models of the Mantel-Haenszel method (13), and the heterogeneity of the study results was evaluated with chi-square-based Q statistics. For the Mantel-Haenszel method, the test for heterogeneity is based on the weights from the inverse-variance method (13). Considering the low power of the Q statistic, the heterogeneity test was considered significant when the p value was less than 0.1 (14). Publication bias was assessed graphically by funnel plot (15) and was statistically evaluated by the regression asymmetry test (16), which has been shown to be a powerful test for assessment of publication bias (17). Finally, the trim and fill method was used to adjust for publication bias (18). All analyses were performed using MedCalc for Windows, version 9.0 (MedCalc Software, Mariakerke, Belgium) and Comprehensive Meta Analysis V2 (Biostat, Englewood, NJ, U.S.A.).
The radiography crystal structure of HLA-DRB1*0401 in complex with a peptide from human collagen II (PDB entry 2SEB) was used as a structural template. The molecular modeling with energy minimization was carried out on an OCTANE R1200 Silicon Graphics workstation with X-build module of QUANTA software and Affinity module of Insight II from Accerlys, Inc. Side chain conformations of the modified residues were assigned to the preferred conformer most similar to the conformation of the side chain in the crystal structure templates and backbone conformations were not changed under restraint. The qualities of the models were analyzed by PROCHECK (19).
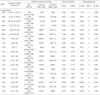
A total of 5,234 articles were identified using the keywords 'human leukocyte antigen' and 'rheumatoid arthritis'. After reviewing the abstracts, we selected 22 articles that studied the association of HLA-DRB1 alleles with RA patients in Asian populations. Ten of these articles were excluded from the analysis: 2 were duplicate publications, 5 had only serologic results, and 3 were studies in non-Mongoloid populations. Therefore, a total of 12 studies, which included 2,204 RA patients and 2,375 healthy controls, were used in our meta-analysis (6-9, 20-27). Characteristics of the studies included are presented in Table 1. All of 12 studies were reporting the association between HLA-DRB1 alleles and RA in Asian-Mongoloid patients, including Korean, Japanese, Chinese, and Thai individuals. The high-resolution typing for HLA-DRB1 alleles was performed with adequately described methods. All studies had a cross-sectional design.
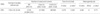
A total of 30 alleles were assayed in the 12 studies: HLA-DRB1* 0101 (DR1); DRB1*1501, *1502, and *1602 (DR2); HLA-DRB1*0301 (DR3); HLA-DRB1*0401, *0402, *0403, *0404, *0405, *0406, *0407, *0408, and *0410 (DR4); DRB1*1101 and DRB1*1201 (DR5); DRB1*1301, *1302 *1401, *1402, *1403, *1405, and *1406 (DR6); HLA-DRB1*0701 (DR7); HLA-DRB1*0802 and *0803 (DR8); HLA-DRB1*0901 (DR9); and HLA-DRB1*1001 (DR10). The results of meta-analysis are summarized in Table 2, 3. The summary ORs showed that Asian-Mongoloid patients with RA had significantly higher frequencies of HLA-DRB1* 0101, *0401, *0410, and *1001 than controls (OR 1.5-2.1, p<0.05 for association). In contrast, the HLA-DRB1 *0301, *0403, *0406, *0701, *1301, and *1405 alleles showed negative associations with RA (OR 0.32-0.70, p< 0.05 for association). Six of the 30 alleles (HLA-DRB1*0405, *0802, *1202, *1302, *1403, and *1501) showed significant heterogeneity (p<0.1 for heterogeneity). When the analysis was restricted to similar ethnic populations (i.e., the Korean, Japanese, and Chinese cohorts), 2 of the alleles (HLA-DRB1* 0405 and *1403) no longer showed significant heterogeneity. In the case of the HLA-DRB1*0405 allele, however, a subgroup analysis of the 4 studies in Korean patients showed a significant association with RA susceptibility (OR 5.65, 95% CI 4.32-7.39). Subanalysis of HLA-DRB1*1403 in Japanese patients also showed homogeneity, but the OR was not significant (p=0.402 for association).
The funnel plot to detect publication bias (15) showed relatively symmetric for most alleles, except for HLA-DRB1* 1405 (not shown). Moreover, the regression asymmetry test (16) did not reveal significant evidence for publication bias (p<0.1), while studies on the HLA-DRB1*1405 allele still showed significant publication bias (p=0.011).
In the SE hypothesis of RA, the amino acid residue at DR 71 is critical for binding to the P4 position of the bound antigenic peptide, thus profoundly influencing T cell recognition and immune response. For example, a positively charged residue (lysine or arginine) at position DR 71 can form a salt bridge with a negatively charged residue (aspartate or glutamate) at the P4 position. A modeling study of the MHC class II-peptide-TCR interaction has shown that the CDR3 loop of TCR is likely to be in contact with the DR residue 71 and the P4 residue of the antigenic peptide (28-30). RA susceptible alleles with a positively charged residue at 71 can accommodate only an antigenic peptide with a negatively charged P4 residue, and the microenvironment of the salt bridge between them can be optimally recognized by the CDR3 loop of TCR, causing signaling immunocyte activation.
Based on the amino acid sequences of alleles identified as susceptible or protective, however, it was suggested that RA susceptibility is determined by the combination of two residues, 71 and 74, not by 71 alone. Although a positively charged residue at 71 is of primary importance for RA susceptibility of an allele, a residue at 74 cannot be ignored because it can also be involved in the interaction with the P4 residue (Fig. 1A). In RA-susceptible alleles such as DRB1*0101, 0401, 0405, 0410, and 1001 (Fig. 1B, C), the residue 71 is positively charged and forms a salt bridge with the negatively charged residue P4, while the alanine residue at 74 does not affect this DR 71-P4 interaction due to its small size. In the DRB1*0403, 0406, and 1405 alleles (Fig. 1D), however, a negatively charged residue, glutamate, at position 74 repels the P4 residue by electrostatic repulsion, resulting in the ability to form the DR 71-P4 salt bridge. This would lead to misalignment of the antigenic peptide in the binding groove and impair antigen recognition by TCR, making these alleles protective against RA. In the DRB1*0701 allele (Fig. 1E), the position of glutamine at 74 would be determined by a hydrogen bond between the N atom of the side chain of Q74 and the backbone carbonyl oxygen of the 70 residue. Therefore, the partial negative charge on the O atom of the side chain of Q74 would face an acidic P4 residue, preventing the formation of the DR 71-P4 salt bridge by electrostatic repulsion. In the DRB1*1301 allele (Fig. 1F), 71 is negatively charged and therefore cannot form a salt bridge with an acidic residue at P4. Taken together, these findings indicate that a positively charged residue at 71 is a necessary but not sufficient condition for RA susceptibility, because the residue at 74 can affect the formation of the DR 71-P4 salt bridge.
HLA molecules with specific shared epitopes (SEs) are considered to explain about 30-40% of the genetic risk for RA (31). There are 5 major susceptibility alleles that share the epitopes QKRAA or QRRAA between residues 70 and 74 of HLA-DRB1: DRB1*0401, *0404, *0101, *0405, and *1402. Although these SE susceptibility sequences increase the risk for RA, there is some heterogeneity in the relative contribution of these 5 alleles to RA susceptibility. In populations in which DRB1*0401 and DRB1*0404 are common, these alleles are usually more associated with the disease than others. Conversely, in populations in which DRB1 *0401 and DRB1*0404 are rare, other alleles, such as DRB1 *0405 and DRB1*1402, account for the HLA-associated disease risk.
Our meta-analysis of Asian-Mongoloid populations showed that patients with RA had higher frequencies of HLA-DRB1*0101, *0401, *0405, *0410, and *1001 than controls. Unlike in Caucasian populations (5, 32), however, the HLA-DRB1*0404 and *1402 alleles did not increase the susceptibility to RA in Asian-Mongoloid populations. The lack of association between these alleles, which have the same epitope as HLA-DRB1*0405, and RA may be a reflection of the low frequency of these alleles in Asian populations (33). Our meta-analysis also showed that certain DRB1 alleles (HLA-DRB1*0301, *0403, *0406, *0701, *1101, *1301, and *1405) occur at lower frequencies in RA patients than in controls, suggesting that they have protective effects. The protective alleles identified in Asian patients also differed from those reported in Caucasians (HLA-DRB1*07, *1201, *1301, and *1501) (3).
Our structural model can explain the role of SE for most of the alleles showing significant RA susceptibility or protection, except for the protective role of DRB1*0301 allele. Since HLA-DRB1*0301 has been reported to be susceptible to other autoimmune diseases such as autoimmune hepatitis (34, 35) and our results on this allele were obtained from only 2 papers, we extended the meta-analysis using papers with low resolution results for DRB1*03. This was justified with the fact that a great majority of Asian-Mongoloid individuals with HLA-DRB1*03 are positive for *0301 (33). The result showed that HLA-DRB1*03 was significantly less frequent in RA patients than in controls, although none of the individual studies showed a statistically significunt difference (Table 4). HLA-DRB1*0301 allele has been reported to be marginally protective in Singaporean Chinese, although the statistical significance was lost after Bonferroni correction (7). The marginal association of DRB1*0301 with RA protection may arise from loose linkage disequilibrium with other genetic loci near to HLA. Genome scan analysis has revealed that genetic associations with RA are complex and that at least two additional genetic effects are present close to or within the major histocompatibility complex (36, 37). The A9 allele of the MICA gene, located between class I and class II HLA, has been found to be protective against RA in Koreans (38). Our unpublished data on MICA-DRB1 haplotype distribution showed strong linkage disequilibrium between the DRB1*0301 and MICA A9 alleles in Koreans (relative linkage disequilibrium=0.633), suggesting that susceptibility of HLA-DRB*0301 to RA may be due to other nearby genetic loci in linkage disequilibrium.
Our analysis showed that the DRB1*0405, *0410, and *0401 alleles are associated with RA susceptibility whereas the DRB1*0403 and DRB1*0406 alleles are associated with RA protection in Asian-Mongoloid individuals. Among the HLA-DR antigens, HLA-DR4 is the most heterogeneous in Asian populations and the DRB1*0403 and *0406 alleles are more frequently present in normal Koreans (33, 39) and Japanese (33, 40) than in Caucasians (less than 0.1%) (33, 41). This may be the reason why several studies have reported a lack of association between the DR4 antigen and RA in Asians.
In conclusion, our meta-analysis enabled us to identify the HLA-DRB1 alleles associated with susceptibility to RA in Asian populations. Our structural model supporting SE hypothesis indicated that RA susceptibility is determined by the combination of the residues at 71 and 74, not by 71 alone, for all associated alleles except DRB1*0301. The weak association between DRB1*0301 and RA may arise from linkage disequilibrium with nearby susceptible loci. This analysis will provide a basis for further studies concerning the effect of HLA-DRB1 and nearby loci on RA in Asian populations.
Figures and Tables
 | Fig. 1Structural analysis of the interactions between the P4 residue of the antigenic peptide and the residues at positions 71 and 74 of DRβ in RA susceptible and protective alleles. (A) Overall structure of the HLA-DR molecule containing a peptide with a negatively charged residue at P4. The positions of DRβ residues 71-74 are indicated by red labels. The region inside the blue rectangle is magnified in panels B-F. (B) Close-up of the interaction of the P4 residue with the HLA DRB1*0401 molecule. Lysine at position 71 makes a salt bridge with the negatively charged P4 residue, leading to the optimal binding of an antigenic peptide for TCR recognition. A small residue, alanine, at amino acid 74 does not inhibit the salt bridge of DRβ 71-P4. The residues at positions 72 and 73 are not involved in peptide binding. (C) Close-up of the interaction of the P4 residue with HLA DRB1*0101, 0404, 0405, 0410, and 1001. The microenvironment is similar to that of DRB1*0401 due to the similar properties of arginine and lysine. (D) Close-up of the interaction of the P4 residue with HLA DRB1* 0403, 0406, and 1405. A negatively charged residue, glutamate, at position 74 would repel the negatively charged P4 residue and inhibit formation of the DRβ 71-P4 salt bridge. (E) Close-up of the interaction of the P4 residue with HLA DRB1*0701. The hydrogen bond between the N atom of the side chain of Q74 and the backbone carbonyl oxygen of the β70 residue causes an electrostatic repulsion between the partial negative charge on the O atom of the side chain of Q74 and an acidic P4 residue. (F) Close-up of the interaction of the P4 residue with HLA DRB1*1301. |
Table 1
Characteristics of the studies included in the meta-analysis on the association of HLA-DRB1 with RA patients in Asian populations

Table 2
Summary of cumulative meta-analysis for the association between HLA-DRB1 alleles and RA susceptibility in Asian populations

References
2. Gregersen PK, Silver J, Winchester RJ. The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum. 1987. 30:1205–1213.

3. de Vries N, Tijssen H, van Riel PL, van de Putte LB. Reshaping the shared epitope hypothesis: HLA-associated risk for rheumatoid arthritis is encoded by amino acid substitutions at positions 67-74 of the HLA-DRB1 molecule. Arthritis Rheum. 2002. 46:921–928.

4. Gorman JD, Criswell LA. The shared epitope and severity of rheumatoid arthritis. Rheum Dis Clin North Am. 2002. 28:59–78.

5. Gorman JD, David-Vaudey E, Pai M, Lum RF, Criswell LA. Lack of association of the HLA-DRB1 shared epitope with rheumatoid nodules: an individual patient data meta-analysis of 3,272 Caucasian patients with rheumatoid arthritis. Arthritis Rheum. 2004. 50:753–762.

6. Lee HS, Lee KW, Song GG, Kim HA, Kim SY, Bae SC. Increased susceptibility to rheumatoid arthritis in Koreans heterozygous for HLA-DRB1*0405 and *0901. Arthritis Rheum. 2004. 50:3468–3475.

7. Chan SH, Lin YN, Wee GB, Koh WH, Boey ML. HLA class 2 genes in Singaporean Chinese rheumatoid arthritis. Br J Rheumatol. 1994. 33:713–717.

8. Tokunaga NK, Noda R, Kaneoka H, Ogahara S, Murata T, Hiratsuka T, Michinaga I, Naito S. Association between HLA-DRB1*15 and Japanese patients with rheumatoid arthritis complicated by renal involvement. Nephron. 1999. 81:165–171.

9. Yukioka M, Wakitani S, Murata N, Toda Y, Ogawa R, Kaneshige T, Ochi T. Elderly-onset rheumatoid arthritis and its association with HLA-DRB1 alleles in Japanese. Br J Rheumatol. 1998. 37:98–101.

10. Apple RJ, Erlich H. Browning MJ, McMichael AJ, editors. HLA class II genes: structure and diversity. HLA and MHC: genes, molecules and function. 1996. Oxford (UK): BIOS Scientific Publishers, Ltd;100.
11. Conn VS, Rantz MJ. Research methods: managing primary study quality in meta-analyses. Res Nurs Health. 2003. 26:322–333.

12. Huwiler-Muntener K, Juni P, Junker C, Egger M. Quality of reporting of randomized trials as a measure of methodologic quality. JAMA. 2002. 287:2801–2804.

13. Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959. 22:719–748.
14. Attia J, Thakkinstian A, D'Este C. Meta-analyses of molecular association studies: methodologic lessons for genetic epidemiology. J Clin Epidemiol. 2003. 56:297–303.

15. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001. 54:1046–1055.
16. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997. 315:629–634.

17. Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000. 53:1119–1129.
18. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000. 56:455–463.

19. Laskowski RA, MacArthur MW, Moss DS, Thornton JM. PROCHECK: a program to check the stereochemical quality for assessing the accuracy of protein structures. J Appl Cryst. 1993. 26:283–291.
20. Kim TG, Choi HB, Park SH, Kim HY, Han H. DQCAR 113 and DQCAR 115 in combination with HLA-DRB1 alleles are significant markers of susceptibility to rheumatoid arthritis in the Korean population. Tissue Antigens. 1999. 54:552–559.

21. Hong GH, Park MH, Takeuchi F, Oh MD, Song YW, Nabeta H, Nakano K, Ito K, Park KS. Association of specific amino acid sequence of HLA-DR with rheumatoid arthritis in Koreans and its diagnostic value. J Rheumatol. 1996. 23:1699–1703.
22. Kim HY, Kim TG, Park SH, Lee SH, Cho CS, Han H. Predominance of HLA-DRB1*0405 in Korean patients with rheumatoid arthritis. Ann Rheum Dis. 1995. 54:988–990.

23. Molkentin J, Gregersen PK, Lin X, Zhu N, Wang Y, Wang Y, Chen S, Chen S, Baxter-Lowe LA, Silver J. Molecular analysis of HLA-DR beta and DQ beta polymorphism in Chinese with rheumatoid arthritis. Ann Rheum Dis. 1993. 52:610–612.

24. Seglias J, Li EK, Cohen MG, Wong RW, Potter PK, So AK. Linkage between rheumatoid arthritis susceptibility and the presence of HLA-DR4 and DR beta allelic third hypervariable region sequences in southern Chinese persons. Arthritis Rheum. 1992. 35:163–167.
25. Takeuchi F, Nakano K, Matsuta K, Nabeta H, Bannai M, Tanimoto K, Ito K. Positive and negative association of HLA-DR genotypes with Japanese rheumatoid arthritis. Clin Exp Rheumatol. 1996. 14:17–22.
26. Higami K, Hakoda M, Matsuda Y, Ueda H, Kashiwazaki S. Lack of association of HLA-DRB1 genotype with radiologic progression in Japanese patients with early rheumatoid arthritis. Arthritis Rheum. 1997. 40:2241–2247.

27. Pimtanothai N, Kimkong I, Inwattana R, Deesomchok U, Charoenwongse P. DRB1*04 subtype in Thai patients with rheumatoid arthritis. J Med Assoc Thai. 2002. 85:Suppl 1. S366–S370.
28. Penzotti JE, Doherty D, Lybrand TP, Nepom GT. A structural model for TCR recognition of the HLA class II shared epitope sequence implicated in susceptibility to rheumatoid arthritis. J Autoimmun. 1996. 9:287–293.

29. Garboczi DN, Ghosh P, Utz U, Fan QR, Biddison WE, Wiley DC. Structure of the complex between human T-cell receptor, viral peptide and HLA-A2. Nature. 1996. 384:134–141.

30. Garcia KC, Degano M, Stanfield RL, Brunmark A, Jackson MR, Peterson PA, Teyton L, Wilson IA. An alphabeta T cell receptor structure at 2.5 A and its orientation in the TCR-MHC complex. Science. 1996. 274:209–219.
31. Rigby AS, Silman AJ, Voelm L, Gregory JC, Ollier WE, Khan MA, Nepom GT, Thomson G. Investigating the HLA component in rheumatoid arthritis: an additive (dominant) mode of inheritance is rejected, a recessive mode is preferred. Genet Epidemiol. 1991. 8:153–175.

32. Fries JF, Wolfe F, Apple R, Erlich H, Bugawan T, Holmes T, Bruce B. HLA-DRB1 genotype associations in 793 white patients from a rheumatoid arthritis inception cohort: frequency, severity, and treatment bias. Arthritis Rheum. 2002. 46:2320–2329.

33. Gjertson DW, Terasaki PI. HLA 1998. 1998. Kansas: American Society for Histocampatibility and Immunogenetics;202–221.
36. Brintnell W, Zeggini E, Barton A, Thomson W, Eyre S, Hinks A, Silman AJ, Worthington J. Evidence for a novel rheumatoid arthritis susceptibility locus on chromosome 6p. Arthritis Rheum. 2004. 50:3823–3830.

37. Jawaheer D, Li W, Graham RR, Chen W, Damle A, Xiao X, Monteiro J, Khalili H, Lee A, Lundsten R, Begovich A, Bugawan T, Erlich H, Elder JT, Criswell LA, Seldin MF, Amos CI, Behrens TW, Gregersen PK. Dissecting the genetic complexity of the association between human leukocyte antigens and rheumatoid arthritis. Am J Hum Genet. 2002. 71:585–594.

38. Mok JW, Lee YJ, Kim JY, Lee EB, Song YW, Park MH, Park KS. Association of MICA polymorphism with rheumatoid arthritis patients in Koreans. Hum Immunol. 2003. 64:1190–1194.

39. Song EY, Park MH, Kang SJ, Park HJ, Kim BC, Tokunaga K, Akaza T, Juji T. HLA class II allele and haplotype frequencies in Koreans based on 107 families. Tissue Antigens. 2002. 59:475–486.

40. Saito S, Ota S, Yamada E, Inoko H, Ota M. Allele frequencies and haplotypic associations defined by allelic DNA typing at HLA class I and class II loci in the Japanese population. Tissue Antigens. 2000. 56:522–529.

41. Ncbi.nlm.nih.gov [homepage on the Internet]. updated 2006 Oct 30; cited 2006 Nov 29. Bethesda: National Center for Biotechnology Information;Available from:
http://www.ncbi.nlm.nih.gov/projects/mhc/ihwg.cgi
.
Notes
This research was supported by the Intelligent Microsystem Center (IMC; http://www.microsystem.re.kr), which carries out one of the 21st centrury's Frontier R&D Projects sponsored by the Korea Ministry of Commerce, Industry and Energy.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download