Abstract
Peroxisome proliferator-activated receptor gamma (PPAR-γ) is a ligand-activated transcription factor and plays an important role in growth, differentiation, and inflammation in different tissues. In this study, we investigated the effects of 15d-PGJ2, a high-affinity ligand of PPAR-γ, on dedifferentiation and on inflammatory responses such as COX-2 expression and PGE2 production in rabbit articular chondrocytes with a focus on ERK-1/-2, p38 kinase, and PPAR-γ activation. We report here that 15d-PGJ2 induced dedifferentiation and/or COX-2 expression and subsequent PGE2 production. 15d-PGJ2 treatment stimulated activation of ERK-1/-2, p38 kinase, and PPAR-γ. Inhibition of ERK-1/-2 with PD98059 recovered 15d-PGJ2-induced dedifferentiation and enhanced PPAR-γ activation, whereas inhibition of p38 kinase with SB203580 potentiated dedifferentiation and partially blocked PPAR-γ activation. Inhibition of ERK-1/-2 and p38 kinase abolished 15d-PGJ2-induced COX-2 expression and subsequent PGE2 production. Our findings collectively suggest that ERK-1/-2 and p38 kinase oppositely regulate 15d-PGJ2-induced dedifferentiation through a PPAR-γ-dependent mechanism, whereas COX-2 expression and PGE2 production is regulated by ERK-1/-2 through a PPAR-γ-independent mechanism but not p38 kinase in articular chondrocytes. Additionally, these data suggest that targeted modulation of the PPAR-γ and mitogen-activated protein kinase pathway may offer a novel approach for therapeutic inhibition of joint tissue degradation.
Cartilage is developed by the differentiation of mesenchymal cells into chondrocytes (1). Differentiated chondrocytes in articular cartilage maintain homeostasis by synthesizing cartilage-specific matrix molecules. However, this homeostasis is destroyed during pathogenesis of cartilage disease, such as arthritis. Cartilage destruction during arthritis involves the loss of differentiated phenotype (dedifferentiation) and apoptotic death of chondrocytes, which is caused by the production of pro-inflammatory cytokines such as interleukin (IL)-1β (2).
Peroxisome proliferator-activated receptor (PPAR)-γ is a member of the nuclear receptor superfamily of ligand-dependent transcription factors. PPAR-γ forms a heterodimeric complex with the retinoid X receptor (3) and binds to specific nucleotide motifs (direct repeats with single spacing, DR1) located in the promoter of target genes. It was originally characterized as a regulator of adipocyte differentiation and lipid metabolism (4, 5). Recently, PPAR-γ was also shown to be expressed in other cell types, including endothelial cells and chondrocytes (6, 7). PPAR-γ ligands inhibit the IL-1β-induced nitric oxide (NO) and matrix metalloproternase-13 (MMP-13) production, as well as a decrease of proteoglycan synthesis (8). The presence of the expression of the PPAR-γ in chondrocytes may provide a new insight in the understanding of the mechanisms which lead to the loss of cartilage homeostasis.
The cyclopentenone prostaglandins (PGs) are important regulators of cellular function in a variety of tissues, including bone and cartilage. PGD2 is a mediator of allergy and inflammation (9). PGJ2 is formed within the cyclopentenone ring of the endogenous prostaglandin PGD2 by a nonenzymatic reaction. PGJ2 is metabolized further to yield Δ12-2 and 15-deoxy-Δ12,14 PGJ2 (15d-PGJ2). The PGJ family is involved in mediating various biological effects including the regulation of cell cycle progression and inflammatory responses (10). In contrast to classical PGs, which bind to cell surface G protein-coupled receptors, 15d-PGJ2 is a natural ligand of a nuclear receptor, PPAR-γ. This receptor behaves as a ligand-activated transcription factor through its DNA binding domain, which recognizes response elements in the promoter of some target genes linked to apoptosis, cell proliferation, and differentiation and inflammation (11, 12). Recent data showed the presence of PPAR-γ in rat cartilage and human synovial tissues (5) and indicated that 15d-PGJ2 is the most potent endogenous ligand for PPAR-γ yet discovered (13).
Mitogen-activated protein (MAP) kinases are serine/threonine kinases that regulate a variety of processes, including cell growth, proliferation, apoptosis, and extracellular matrix accumulation. Our previous studies in articular chondrocytes indicated that NO caused apoptosis and dedifferentiation, which are mediated by MAP kinases subtypes extracellular signal-regulated protein kinase (ERK) and p38 kinase (14). These MAP kinases play opposing roles, with activated ERK-1/-2 inducing dedifferentiation, COX-2 expression, and inhibiting NO-induced apoptosis, while p38 kinase signaling triggers apoptosis, COX-2 expression, and maintains the differentiated status.
Other recent studies have identified PPAR-γ as a substrate of mitogen-activated protein kinases (15). The transcriptional activity of PPAR-γ is positively modulated by ligand binding and negatively regulated by phosphorylation mediated by the MEK/ERK signaling pathway. Also, PPAR-γ is efficiently phosphorylated by JNK/SAPK (c-Jun N-terminal kinase or stress-activated protein kinase) but only weakly phosphorylated by p38 (4). Evidence that 15d-PGJ2 modulates MAP kinase activity is conflicting. It has been shown that 15d-PGJ2 activates JNK in untreated HeLa cells (16), but blocks IL-1-induced JNK phosphorylation in rodent pancreatic islets (17). Similarly, induction of macrophage apoptosis by 15d-PGJ2 was shown to depend on the p38 MAP kinase; however, 15d-PGJ2 appeared to decrease phosphorylation of p38 (18), a step necessary for its activity. These data imply that the effects of 15d-PGJ2 on MAP kinases may be cell-context specific.
Therefore, in this study, we investigated whether PPAR-γ activators may modulate the differentiation and inflammatory responses (COX-2 expression/PGE2 production) in primary culture rabbit articular chondrocytes. We additionally characterized the signaling mechanism of regulation of 15d-PGJ2-induced dedifferentiation and inflammation, focusing on the roles of MAP kinases. Here, we report that 15d-PGJ2-induced dedifferentiation and COX-2 expression/PGE2 production is regulated by modulation of MAP kinases activation.
Rabbit articular chondrocytes were isolated from the cartilage of 2-week-old New Zealand white rabbits as described previously (19). Cartilage slices were dissociated enzymatically for 4 hr in 0.2% collagenase type II (381 U/mg solid, Sigma) in Dulbecco's modified Eagle's medium (DMEM; Gibco-BRL, Gaithersburg, MD, U.S.A.). Individual cells were suspended in DMEM supplemented with 10% (v/v) fetal bovine-calf serum, 50 µg/mL streptomycin, and 50 units/mL penicillin and plated on culture dishes at a density of 5×104 cells/cm2. After 4 days in culture, the cells were treated with the indicated pharmacological reagents for 1 hr prior to 15d-PGJ2 (Calbiochem, San- diego, CA, U.S.A.), such as SB203580 (Calbiochem) to inhibit p38 kinase and PD98059 (Calbiochem) to inhibit MEK-1/-2. The transfected cells, which were cultured in complete medium for 24 hr, were used for further analysis as indicated in each experiment. Differentiation status of articular chondrocytes was determined by immunoblot analysis by examining the expression of type II collagen as described below. Alternatively, cells cultured for various time periods were stained with Alcian blue to localize the sulfated cartilage matrix. Alcian blue bound to sulfated glycosaminoglycans was extracted with 4M guanidine-HCl and quantitated by measuring the absorbance at 600 nm.
Whole cell lysates were prepared by extracting proteins using a buffer containing 50 mM Tris-HCl, pH 7.4, 150 mM NaCl, 1% Nonidet P-40, and 0.1% sodium dodecyl-sulfate (SDS), supplemented with protease inhibitors (10 µg/mL leupeptin, 10 µg/mL pepstatin A, 10 µg/mL aprotinin and 1 mM of 4-[2-aminoethyl] benzenesulfonyl fluoride) and phosphatase inhibitors (1 mM NaF and 1 mM Na3VO4). The proteins were size-fractionated by SDS-polyacrylamide gel electrophoresis and transferred to a nitrocellulose membrane. The nitrocellulose sheet was then blocked with 3% non-fat dry milk in Tris-buffered saline. The following antibodies were used: anti-COX-2 (Cayman Chemical Ann Arbor, MI, U.S.A.), pp38 (Cell signaling, Beverly, MA, U.S.A.), pERK, ERK-2, p38, PPAR-γ, and SOX-9 (Santa Cruz Biotechnology Inc., Santa Cruz, CA, U.S.A.), and type II collagen (Chemicon, Temecula, CA, U.S.A.). Blots were developed using a peroxidase-conjugated secondary antibody on a chemiluminescence system.
PGE2 production was determined by measuring the levels of cellular and secreted PGE2 using an assay kit (Amersham Pharmacia Biotech, NJ, U.S.A.). Briefly, chondrocytes were seeded in standard 96-well microtiter plates at 2×104 cells/well. Following addition of the indicated pharmacological reagents, the supernatant was used to quantify the amount of PGE2, according to the manufacturer's protocol. PGE2 levels were calculated using a PGE2 standard curve.
Rabbit joint cartilage explants (~125 µL) were fixed in 4% paraformaldehyde in PBS for 24 hr at 4℃, washed with PBS, dehydrated in ethanol, embedded in paraffin, and sectioned at 4 µm thickness as described previously (23). The sections were stained by standard procedures using antibodies against type II collagen and COX-2 and Alcian blue staining, and visualized by developing with a kit purchased from DAKO (Carpinteria, CA, U.S.A.), following the procedure recommended by the manufacturer.
Expression and distribution of type II collagen and COX-2 in rabbit articular chondrocytes were determined by indirect immunofluorescence microscopy, as described previously (19). Briefly, chondrocytes were fixed with 3.5% paraformaldehyde in PBS for 10 min at room temperature. The cells were permeabilized and blocked with 0.1% Triton X-100 and 5% fetal calf serum in PBS for 30 min. The fixed cells were washed and incubated for 1 hr with antibody (10 µg/mL) against type II collagen and COX-2. The cells were washed, incubated with rhodamine- or fluorescein-conjugated secondary antibodies for 30 min, and observed under a fluorescence microscope.
The reporter construct (3xPPRE-TK-luc/pGL3) used in the transfections contained three copies of the PPRE site from the aP2 enhancer (ARE7) inserted upstream of a minimal thymidine kinase (TK) promoter in the pGL3 basic luciferase vector and RXRα cDNA (a gift from Dr. JB, Kim at Seoul National University). Transfection of the reporter vector was performed as described previously (20). Chondrocytes were grown in 10% fetal calf serum/DMEM and co-transfected with various reporter plasmids (1 µg) and pCMVβ-galactosidase plasmid (Clontech) using Lipofectamine (Life Technologies, Inc., Grand island, NY, U.S.A.), following the procedure recommended by the manufacturer. The transfected cells were cultured in complete medium for 24 hr and used for further assay. Cells were treated with increasing concentrations (0-20 µM) or times (0-24 hr) of 15d-PGJ2. Cell extracts were assayed for luciferase activity. Luciferase and β-galactosidase activities were determined using a luciferase assay (Promega, Madison, WI, U.S.A.) and Galacto-light system (Tropix, Inc., Bedford, MA, U.S.A.). The activities were corrected for transfection efficiency with β-gal activity and expressed as fold-induction relative to the level in untreated cells. Each assay was performed in triplicate.
The results are expressed as the means ± S.D. (Standard Deviation) values calculated from the specified number of determinations. Student's t-test was used to compare individual treatments with their respective control values. A probability of p<0.05 was taken as denoting a significant difference.
Rabbit articular chondrocytes in primary culture were treated with the natural ligand of PPAR-γ, 15d-PGJ2. 15d-PGJ2-treated chondrocytes suppress type II collagen (a marker for differentiation of chondrocytes) and SOX-9 (a major transcription factor that regulates type II collagen expression) expression in a time- and dose-dependent manner as determined by immunoblot analysis (Fig. 1A). As expected, 15d-PGJ2 treatment of cartilage explants blocked type II collagen expression and accumulation of sulfated proteoglycan, as determined via immunohistochemistry and Alcian blue staining, respectively (Fig. 1B). Consistent with the expression pattern of type II collagen, 15d-PGJ2 treatment led to a time- and dose-dependent decrease in the accumulation of sulfated proteoglycan (Fig. 1C, D). These results indicate that 15d-PGJ2 induces dedifferentiation of articular chondrocytes in both primary culture cells and cartilage explants.
The effect of 15d-PGJ2 on COX-2 expression and PGE2 production was investigated using both primary culture chondrocytes and cartilage explant cultures. In primary culture chondrocytes, 15d-PGJ2 increased protein levels of COX-2 in a time- and dose-dependent manner as determined by immunoblot analysis (Fig. 2A). COX-2 was increased 1 hr after 15d-PGJ2 treatment, and levels peaked at 12 hr. In cartilage explants, 15d-PGJ2 stimulated COX-2 expression as determined by immunohistochemical staining (Fig. 2B). Consistent with the induction of COX-2 expression, 15d-PGJ2 stimulated PGE2 production (Fig. 2C) that was detectable 3 hr after 15d-PGJ2 addition (Fig. 2D). These data indicate that 15d-PGJ2 not only causes dedifferentiatin of articular chondrocytes but also stimulates COX-2 expression and PGE2 production.
To investigate the signaling pathway stimulating dedifferentiation and/or COX-2 expression and PGE2 production of 15d-PGJ2-treated chondrocytes, we initially examined changes in the activity of ERK-1/-2 and p38 kinase. These two subtypes were selected for study, based on results from previous data (25) indicating that the proteins conversely regulate chondrocyte differentiation. When cells were treated with 15d-PGJ2, the ERK-1/-2 activity was transiently increased, as determined by immunoblot analysis with anti-phospho-ERK-1/-2 antibody (Fig. 3). Levels of ERK-1/-2 phosphorylation began to increase at 15 min, sustained levels at 1 hr, and decreased thereafter. Similar to the pattern of ERK activation, the p38 kinase activity was also transiently increased in 15d-PGJ2-treated cells (Fig. 3). The effects of 15d-PGJ2 on ERK-1/-2 and p38 kinase activity were time-dependent.
In an attempt to elucidate the role of PPAR-γ in 15d-PGJ2-induced dedifferentiation and COX-2 expression, we first determined the expression and transcription activity. As shown in Fig. 4A, 15d-PGJ2 treatment did not affect PPAR-γ expression, but caused activation of PPAR-γ in a time- and dose-dependent manner (Fig. 4B, C). These results show that 15d-PGJ2 caused activation of ERK-1/-2, p38 kinase and PPAR-γ in articular chondrocytes.
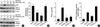
The role of ERK-1/-2 and p38 kinase in 15d-PGJ2-induced dedifferentiation and COX-2 expression of chondrocytes was next investigated. The addition of SB203580 to 15d-PGJ2-treated chondrocytes accelerated the decreased type II collagen expression (Fig. 5A, upper panel) and proteoglycan synthesis (Fig. 5B) in a dose-dependent manner. SB203580 completely blocked both 15d-PGJ2-stimulated COX-2 expression (Fig. 5A, upper panel) and PGE2 production (Fig. 5C) and partially suppressed PPAR-γ activation (Fig. 5D). In contrast to the effects of p38 kinase inhibition, the blockade of ERK-1/-2 blocked 15d-PGJ2-induced decrease of type II collagen expression (Fig. 5A, lower panel) and proteoglycan synthesis (Fig. 5B). PD98059 partially blocked 15d-PGJ2-stimulated COX-2 expression (Fig. 5A, lower panel) but completely blocked PGE2 production (Fig. 5C), and potentiated PPAR-γ activation (Fig. 5D). Addition of PD98059 or SB203580 to 15d-PGJ2-treated chondrocytes displayed no cytotoxicity, as assessed by the conversion of a tetrazolium compound to its formazan product, as well as trypan blue exclusion (data not shown). Taken together, these results indicate that 15d-PGJ2-induced dedifferentiation is regulated by ERK-1/-2 activity but not by p38 kinase activity via PPAR-γ-dependent mechanism, whereas 15d-PGJ2-induced COX-2 expression and PGE2 production is regulated by ERK-1/-2 and p38 kinase via PPAR-γ-independent and -dependent mechanism, respectively.
Articular cartilage is a major component of the joint, and its mechanical properties depend on the integrity of the extracellular matrix, which is composed mainly of proteoglycans and collagens (21). Chondrocytes in normal articular cartilage are a unique cell type in that their differentiated phenotype is reversible. Chondrocyte phenotype is regulated by a balance of anabolic and catabolic molecular reactions that are involved in maintaining homeostasis of cartilage tissue (2). Differentiated chondrocytes lose their phenotype and transform into fibroblasts-like cells upon exposure to soluble factors such as IL-1β (22), retinoic acid (23), and NO (24), or during serial subculture in vitro (25). Such a destruction of homeostasis is believed to be involved in the pathophysiology of arthritis, rheumatoid arthritis (RA), and osteoarthritis (OA) (2, 26). Several inflammatory mediators, including NO and PG, have been implicated in the disease process of RA and OA. PGs are produced by cytokine-stimulated chondrocytes in arthritis-affected cartilage via induction of COX-2 expression (27).
In this study, we demonstrated that 15d-PGJ2 caused a loss of differentiated chondrocyte phenotype as demonstrated by inhibition of type II collagen expression and sulfated proteoglycan synthesis in a time- and dose-dependent manner. 15d-PGJ2 also induced COX-2 expression and PGE2 production. Inhibition of ERK-1/-2 with PD98059 recovered 15d-PGJ2-induced type II collagen expression, and potentiated PPAR-γ activation, whereas inhibition of p38 kinase with SB203580 decreased the type II collagen expression, and partially blocked PPAR-γ activation (Fig. 4). 15d-PGJ2-induced COX-2 expression and PGE2 production is regulated by ERK-1/-2 and p38 kinase signaling. The regulation of COX-2 expression has been shown to occur at both transcriptional and post-transcriptional levels, and structural information on the COX-2 gene promoter revealed binding sites for several transcription factors found in many cell types such as NF-κB and CAAT enhancer-binding protein, which are involved in transcription factors found in many cell types such as NF-κB and CAAT enhancer-binding protein, which are involved in transcription regulation of COX-2 (28). The stability of COX-2 mRNA regulated by sequences within the 3'-untranslated region is also an important regulatory mechanism of COX-2 expression (29). In addition, several studies linked COX-2 expression with MAPK subtypes including ERK-1/-2, p38 kinase, and c-Jun N-terminal kinase (30, 31). Therefore, our observation that 15d-PGJ2-induced expression and activity of COX-2 are regulated by ERK-1/-2 and p38 kinase signaling is consistent with the observations of others (30, 31). We observed in this study that 15d-PGJ2-induced dedifferentiation and/or COX-2 expression and PGE2 production are mediated by ERK-1/-2 and p38 kinase activation via PPAR-γ-dependent and -independent mechanism, respectively, in rabbit articular chondrocytes.
Taken together, these results suggest that PPAR-γ antagonists may provide a new therapeutic approach for RA and OA.
Figures and Tables
Fig. 1
15d-PGJ2 treatment of primary culture cells induces dedifferentiation. (A) Rabbit joint articular chondrocytes were treated with 10 µM 15d-PGJ2, the PPAR-γ activator, for the indicated time periods (upper panel, A) or with the indicated concentrations of 15d-PGJ2 for 24 hr (lower panel, A). Expression of type II collagen and SOX-9 was detected using immunoblot analysis. (B) Cartilage explants were untreated or treated with 10 µM 15d-PGJ2 for 24 hr. Type II collagen and proteoglycan were detected by immunohistochemical staining (×400) and Alcian blue staining (×400), respectively. (C , D) Chondrocytes were treated for the indicated time periods with 10 µM 15d-PGJ2 (C) of with the indicated concentrations of 15d-PGJ2 for 24 hr (D). Accumulation of sulfated glycosaminoglycan was quantified by Alcian blue staining. The data represent results of a typical experiment (A, B) or mean values±S.D. (C, D) from at least four independent experiments. *, p<0.05; †, p<0.01 compared with untreated cells.

Fig. 2
15d-PGJ2 treatment of primary culture cells increases COX-2 expression and PGE2 production. (A) Primary culture chondrocytes were treated with 15d-PGJ2 (10 µM) for various time periods (upper panel) or with the indicated concentrations of 15d-PGJ2 for 24 hr (lower panel). COX-2 expression was determined by immunoblot analysis. (B) Articular chondrocytes were untreated or treated with 10 µM 15d-PGJ2 for 24 hr, and COX-2 expression was determined by immunohistochemical staining (×400). (C, D) Chondrocytes were treated for the indicated time periods with 10 µM 15d-PGJ2 (C) or with the indicated concentrations of 15d-PGJ2 for 24 hr (D). Levels of cellular and secreted PGE2 were determined by a assay kit. The data in A and B represent results of a typical experiment, and the data in C-D represent mean values±S.D. (n=4). *, p<0.05; †, p<0.01 compared with untreated cells.

Fig. 3
15d-PGJ2 treatment of primary culture cells stimulates ERK-1/-2 and p38 kinase activation. Chondrocytes were treated with 10 µM 15d-PGJ2 for the indicated periods. ERK-1/-2 and p38 kinase phosphorylation were detected using immunoblot analysis with anti-phospho-ERK-1/-2 and anti-phospho-p38 kinase antibodies. The data represent results of a typical experiment.

Fig. 4
15d-PGJ2 treatment of primary culture cells stimulates PPAR-γ transcriptional activity. (A) Chondrocytes were treated with 10 µM 15d-PGJ2 for the indicated periods (upper panel), or with the indicated concentrations of 15d-PGJ2 for 24 hr (lower panel). (B, C) Primary culture chondrocytes cells were co-transfected with reporter plasmids (3xPPRE-TK-Luc/pGL3) and RXRα expression plasmids (RXRα/pSG5). pCMV β-galactosidase plasmid was used as an internal control for the transfection efficiency. Transfected cells were treated with 15d-PGJ2 (10 µM) for various time periods (B) or with the indicated concentrations of 15d-PGJ2 for 24 hr (C). The cell extracts were assayed for luciferase activity and β-galactosidase activity. The data in A represent results of a typical experiment, and the data in B-C represent mean values±S.D. (n=4). *, p<0.05; †, p<0.01 compared with untreated cells.

Fig. 5
Dedifferentiation and COX-2 expression is regulated by MAP kinases activation through a modulation of PPAR-γ-transcriptional activity. (A) Articular chondrocytes were treated with 10 µM 15d-PGJ2 in the absence or presence of the indicated concentrations of SB203580 (SB) or PD98059 (PD). p38 kinase and ERK phosphorylation, type II collagen and COX-2 were detected by immunoblot analysis. (B, C) Chondrocytes were untreated or treated with 10 µM PD or SB and exposed to 10 µM 15d-PGJ2 for 24 hr. Accumulation of sulfated proteoglycan was quantified by Alcian blue staining (B). PGE2 levels were determined using an assay kit (C). (D) Primary culture chondrocytes were co-transfected with reporter plasmids (3xPPRE-TK-Luc/pGL3) and RXRα expression plasmids (RXRα/pSG5). pCMV β-galactosidase plasmid was used as an internal control for the transfection efficiency. Transfected cells were treated with 10 µM PD or 10 µM SB and then with 10 µM 15d-PGJ2 for 24 hr. The cell extracts was assayed for luciferase activity and β-galactosidase activity. The data represent results of a typical experiment (A) or mean values±S.D. (B-D) from at least four independent experiments. *, p<0.05;†, p<0.01 compared with 15d-PGJ2.
References
1. DeLise AM, Fischer L, Tuan RS. Cellular interactions and signaling development. Osteoarthrtis Cartilage. 2000. 8:309–334.
2. Sandell LJ, Aigner T. Articular cartilage and changes in arthritis. An introduction: cell biology of osteoarthritis. Arthritis Research. 2001. 3:107–113.

3. Isenmann I, Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature. 1990. 347:645–650.

4. Tontonoz P, Hu E, Spiegelman BM. Stimulation of adipogenesis in fibroblasts by PPAR gamma 2, a lipid-activated transcription factor. Cell. 1994. 79:1147–1156.
5. Chawla A, Schwar EJ, Dimaculangan DD, Lazar MA. Peroxisome proliferator-activated receptor (PPAR) gamma: adipose-predominant expression and induction early in adipocyte differentiation. Endocrinology. 1994. 135:798–800.

6. Xin X, Yang S, Kowalski J, Gerritsen ME. Peroxisome proliferator-activated receptor gamma ligands are potent inhibitors of angiogenesis in vitro and in vivo. J Biol Chem. 1999. 274:9116–9121.
7. Bordji K, Grillasca JP, Gouze JN, Magdalou J, Schohn H, Keller JM, Bianchi A, Dauca M, Netter P, Terlain B. Evidence for the presence of peroxisome proliferator-activated receptor (PPAR) alpha and gamma and retinoid Z receptor in cartilage. PPARgamma activation modulates the effects of interleukin-1beta on rat chondrocytes. J Biol Chem. 2000. 275:12243–12250.
8. Fahmi H, Di Battista JA, Pelletier JP, Mineau F, Ranger P, Martel-Pelletier J. Peroxisome proliferator-activated receptor gamma activators inhibit interleukin-1beta-induced nitric oxide and matrix metalloproteinase 13 production in human chondrocytes. Arthritis Rheum. 2001. 44:595–607.
9. Matsuoka T, Hirata M, Tanaka H, Takashi Y, Murata T, Kabashima K, Sugimoto Y, Kobayashi T, Ushikubi F, Aze Y, Eguhi N, Urade Y, Yoshida N, Kimura K, Mizoguchi A, Honda Y, Nagai H, Narumiya S. Prostaglandin D2 as a mediator of allergic asthma. Science. 2000. 287:2013–2017.

10. Cuzzocrea S, Wayman NS, Mazzon E, Dugo L, Di Paola R, Serraino I, Britti D, Chattergee PK, Caputi AP, Thiemermann C. The cyclopentenone prostaglandin 15-deoxy-Delta (12,14)-prostaglandin J(2) attenuates the development of acute and chronic inflammation. Mol Pharmacol. 2002. 61:997–1007.
11. Kliewer SA, Lenhard JM, Willson TM, Patel I, Morris DC, Lehmann JM. A prostaglandin J2 metabolite binds peroxisome proliferator-activated receptor gamma and promotes adipocyte differentiation. Cell. 1995. 83:813–819.
12. Tugwood JD, Montague CT. Biology and toxicology of PPARgamma ligands. Hum Exp Toxicol. 2002. 21:429–437.
13. Bishop-Bailey D, Hla T. Endothelial cell apoptosis induced by the peroxisome proliferator-activated receptor (PPAR) ligand 15-deoxy-Delta12, 14-prostaglandin J2. J Biol Chem. 1999. 274:17042–17048.
14. Kim SJ, Kim HG, Oh CD, Hwang SG, Song WK, Yoo YJ, Kang SS, Chun JS. p38 kinase-dependent and -independent Inhibition of protein kinase C zeta and -alpha regulates nitric oxide-induced apoptosis and dedifferentiation of articular chondrocytes. J Biol Chem. 2002. 277:30375–30381.
15. Camp HS, Tafuri SR, Leff T. c-Jun N-terminal kinase phosphorylates peroxisome proliferator-activated receptor-gamma1 and negatively regulates its transcriptional activity. Endocrinology. 1999. 140:392–397.
16. Rossi A, Kapahi P, Natoli G, Takahashi T, Chen Y, Karin M, Santoro MG. Anti-inflammatory cyclopentenone prostaglandins are direct inhibitors of IkappaB kinase. Nature. 2000. 403:103–108.
17. Maggi LB, Sadeghi H, Weigand C, Scarim AL, Heitmeier MR, Corbett JA. Anti-inflammatory actions of 15-deoxy-delta 12,14-prostaglandin J2 and troglitazone: evidence for heat shock-dependent and -independent inhibition of cytokine-induced inducible nitric oxide synthase expression. Diabetes. 2000. 49:346–355.

18. Hortelano S, Castrillo A, Alvarez AM, Bosca L. Contribution of cyclopentenone prostaglandins to the resolution of inflammation through the potentiation of apoptosis in activated macrophages. J Immunol. 2000. 165:6525–6531.

19. Yoon YM, Kim SJ, Oh CD, Ju JW, Song WK, Yoo YJ, Huh TL, Chun JS. Maintenance of differentiated phenotype of articular chondrocytes by protein kinase C and extracellular signal-regulated protein kinase. J Biol Chem. 2002. 277:8412–8420.

20. Oh CD, Chang SH, Yoon YM, Lee SJ, Lee YS, Kang SS, Chun JS. Opposing role of mitogen-activated protein kinase subtypes, ERK-1/2 and p38, in the regulation of chondrogenesis of mesenchymes. J Biol Chem. 2000. 275:5613–5619.

21. Poole AR. Mc Carthy DJ, Koopman WJ, editors. Arthritis and Allied Conditions. 2003. 12th Ed.Philadelphia: Lea and Febiger;279–333.
22. Goldring MB, Birkhead J, Sandell LJ, Kimura T, Krane SM. Interleukin 1 suppresses expression of cartilage-specific types II and IX collagens and increases types I and III collagens in human chondrocytes. J Clin Invest. 1988. 82:2026–2037.

23. Ryu JH, Kim SJ, Kim SH, Oh CD, Hwang SG, Chun CH, Oh SH, Seong JK, Huh TL, Chun JS. Regulation of the chondrocyte phenotype by beta-catenin. Development. 2002. 129:5541–5550.

24. Kim SJ, Ju JW, Oh CD, Yoon YM, Song WK, Kim JH, Yoo YJ, Bang OS, Kang SS, Chun JS. ERK-1/2 and p38 kinase oppositely regulate nitric oxide-induced apoptosis of chondrocytes in association with p53, caspase-3, and differentiation status. J Biol Chem. 2002. 277:1332–1339.

25. Benya PD, Padilla SR, Nimni ME. Independent regulation of collagen types by chondrocytes during the loss of differentiated function in culture. Cell. 1978. 15:1313–1321.

26. Gay S, Gay RE, Koopman WJ. Molecular and cellular mechanisms of joint destruction in rheumatoid arthritis: two cellular mechanisms explain joint destruction? Ann Rheum Dis. 1993. 52:Suppl 1. S39–S47.

27. Myers LK, Kang AH, Postlethwaite AE, Rosloniec EF, Morham SG, Shlopov , Goorha S, Ballou LR. The genetic ablation of cyclooxygenase 2 prevents the development of autoimmune arthritis. Arthritis Rheum. 2000. 43:2687–2693.

28. Sheng H, Williams CS, Shao J, Liang P, DuBois RN, Beauchamp RD. Induction of cyclooxygenase-2 by activated Ha-ras oncogene in Rat-1 fibroblasts and the role of mitogen-activated protein kinase pathway. J Biol Chem. 1998. 273:22120–22127.
29. Faour WH, He Y, He QW, de ladurantaye M, Quintero M, Mancini A, Di Battista JA. Prostaglandin E(2) regulates the level and stability of cyclooxygenase-2 mRNA through activation of p38 mitogen-activated protein kinase in interleukin-1 beta-treated human synovial fibroblasts. J Biol Chem. 2001. 276:31720–31731.
30. Matsuura H, Sakaue M, Subbaramaiah K, Kamitani H, Eling TE, Dannenberg AJ, Tanabe T, Inoue H, Arata J, Jetten AM. Regulation of cyclooxygenase-2 by interferon gamma and transforming growth factor alpha in normal human epidermal keratinocytes and squamous carcinoma cells. Role of mitogen-activated protein kinases. J Biol Chem. 1999. 274:29138–29148.
31. Guan Z, Buckman SY, Miller BW, Springer LD, Morrison AR. Interleukin-1beta-induced cyclooxygenase-2 expression requires activation of both c-Jun NH2-terminal kinase and p38 MAPK signal pathways in rat renal mesangial cells. J Biol Chem. 1998. 273:28670–28676.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download