Abstract
The gonadotropin-releasing hormone (GnRH) stimulation test is the gold standard for differentiating central precocious puberty (CPP) from exaggerated thelarche (ET). Because of this test's limitations, previous studies have clarified the clinical and laboratory factors that predict CPP. The present study investigated the early diagnostic significance of pelvic ultrasound in girls with CPP. The GnRH stimulation test and pelvic ultrasound were performed between March 2007 and February 2015 in 192 girls (aged <8 years) with signs of early puberty and advanced bone age. Ninety-three of 192 patients (48.4%) were diagnosed as having CPP and the others (51.6%) as having ET. The CPP group had higher uterine volumes (4.31±2.79 mL) than did the ET group (3.05±1.97 mL, p=0.03). No significant differences were found in other ultrasonographic parameters. By use of receiver operating characteristic curve analysis, the most predictive parameter for CPP was a uterine volume of least 3.30 mL, with an area under the curve of 0.659 (95% confidence interval: 0.576-0.736). The CPP group had significantly higher uterine volumes than did the ET group, but there were no reliable cutoff values in pelvic ultrasound for differentiating between CPP and ET. Pelvic ultrasound should be combined with clinical and laboratory tests to maximize its diagnostic value for CPP.
Precocious puberty is defined as early pubertal development that occurs at ages <9 years for boys and <8 years for girls. Central precocious puberty (CPP, or gonadotropin-dependent precocious puberty) is caused by the pubertal function of the hypothalamic-pituitary-gonadal (HPG) axis and is dependent on gonadotropin-releasing hormone (GnRH). In contrast, incomplete precocious puberty (IPP) develops when there are signs of a secondary sexual characteristic, such as the development of breasts and pubic hair, without accompanying changes in the HPG axis. Representative types of IPP include premature thelarche (PT), wherein the breasts develop, and premature adrenarche, wherein pubic and armpit hairs appear or acne develops.
CPP eventually affects the physical growth of the child and includes a number of negative effects such as the increased occurrence of secondary diseases, including polycystic ovary syndrome, obesity, and metabolic syndrome. PT, which affects a large proportion of the total number of IPP patients, is a normal variant that requires observation without special treatment. However, among its variants is an intermediate stage in which physical changes occur in the entire body (with an increase in bone age and growth acceleration) because of estrogen, but without a complete progression toward puberty. Laboratory hormonal values and pelvic ultrasonographic findings of girls experiencing this intermediate status are close to the median value between PT and CPP, which creates difficulties in diagnosing these conditions in the clinical field. This intermediate stage is reported under various names, including exaggerated thelarche (ET), midlevel precocious puberty, atypical PT, thelarche variant, and nonpersistent CPP.12345
The gold standard in verifying HPG activity is the response of gonadotropin to a GnRH stimulation test. Although this test has the advantage of being highly specific, it has low sensitivity and other disadvantages, such as the need for an intravenous line and that it is time-consuming.2 Hence, the possibility of replacing this test with ultrasonography, which is noninvasive and relatively easy to perform, has been continuously reviewed. Although a standard for using ultrasonography for CPP and IPP detection has been established, consensus on its use in the case of children has not yet been established in South Korea.
In this study, we aimed to investigate the early diagnostic significance of pelvic ultrasound in girls with CPP in comparison with girls with ET. This study also presented a review of the literature.
The subjects of this study were young female patients who presented to the Clinic of Pediatric Endocrinology of our hospital for evaluation of CPP from March 2007 to February 2015. The inclusion criteria for patients were as follows: (i) chronological age <8 years, (ii) children with early breast development and advanced bone age, (iii) children who satisfied the conditions above and who underwent a GnRH stimulation test and pelvic ultrasonography in our hospital, and (iv) children without other abnormal findings in the ultrasonography that might suggest a peripheral type of precocious puberty. From a total of 194 children who satisfied the criteria above, 192 were selected as the study sample. Two children were excluded for the following reasons: one showed a mature teratoma on pelvic ultrasonography and one was diagnosed with Mayer-Rokitansky-Küster-Hauser syndrome. Among the children described above, those with a peak luteinizing hormone (LH) value of >5 IU/L in the GnRH stimulation test were classified as having CPP, whereas those with a peak LH of <5 IU/L were classified as having ET.
We reviewed the medical records of the subjects retrospectively. The medical records of the children were retrieved, and clinical data at the GnRH stimulation test (height, weight, chronological age, bone age, body mass index [BMI]) were investigated. Standard deviation scores of the children' height, weight, and BMI were computed by using the LMS method presented in the 2007 Korean national growth chart. The Greulich-Pyle method was used for bone age measurement. For the GnRH stimulation test, LH and follicle-stimulating hormone (FSH) levels were measured right before and 30 and 60 min after the intravenous injection of 100 µg of compound LH-releasing hormone.67 Serum LH and FSH levels were measured with KIP1311 and KIP0841-0844 kits, respectively (Diasource, Louvain-la-Neuve, Belgium), using an immunoradiometric assay, whereas estradiol levels were measured by using a radioimmunoassay technique (Coat-A-Count Estradiol; Siemens, Erlangen, Germany). Pelvic ultrasonography was performed by skilled doctors in the Department of Radiology of our hospital. Using a conventional full-bladder 4- to 7-MHz transducer and iU22 xMATRIX (Phillips, Bothwell, WA, USA), the uterine length, transverse diameter, fundal anteroposterior diameter (fundus), and cervical anteroposterior diameter (cervix) were measured. The uterine volume was calculated according to the ellipse formula (length×transverse diameter×fundal anteroposterior diameter×0.5233). The ratio of the fundal to cervical anteroposterior diameter (fundus/cervix ratio) was also calculated. The height, width, and length of the ovaries were measured. The volume of each ovary was computed by using the same ellipse formula as for the uterus.
The test and measurement values of the analysis data were expressed as means±standard deviations. After dividing the patient group by using the peak LH value as a criterion, Student's t-test was performed to compare the differences between the two groups. For verification of the diagnostic value of the ultrasonography, a logistic regression analysis and receiver operating characteristic (ROC) curve analysis were performed, in which the two groups, CPP and ET, were the dependent variables, and the uterine length, uterine volume, maximum ovarian volume (between left and right), and uterine/cervix (U/C) ratio were the independent variables. The optimal cutoff values were evaluated by using the Youden index (J),8 which is defined by
The significance level for the statistical analysis was set at 5%, and the SAS Enterprise Guide 6.1 (SAS Institute, Cary, NC, USA) and MedCalc (version 15.8) software programs were used.
Among a total of 192 children, 93 were classified as having CPP (48.4%) and 99 as having ET (51.6%). In terms of clinical values, the CPP group was significantly taller, but BMI standard deviation scores were not significantly different between the two groups. Girls with CPP showed a difference in bone age and chronological age of 1.96±0.88 years, which was significantly higher than that of ET girls of 1.61±1.00 years (p=0.01). The laboratory values in the GnRH stimulation test, including those of serum basal LH, serum basal FSH, peak serum FSH, and peak LH/FSH ratio, were significantly higher in the CPP group (Table 1).
Although the CPP group showed higher uterine volumes, with a significant difference compared with the ET group, no significant difference was observed in the other three measures of uterine length, fundus/cervix ratio, and maximum ovarian volume (Table 2).
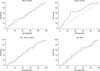
Univariate logistic regression was performed with each ultrasonographic parameter as an independent variable to evaluate the value of pelvic ultrasonography in girls for early diagnosis of CPP. However, no reliable predictor was found. The area under the curve with 95% confidence interval (CI) for each ultrasonographic parameter was 0.546 (0.472-0.619) for uterine length, 0.537 (0.447-0.625) for maximum ovarian volume, 0.519 (0.417-0.619) for U/C ratio, and 0.659 (0.576-0.736) for uterine volume. According to the ROC analysis for each ultrasonographic measure, uterine length showed a sensitivity of 33.33% and a specificity of 79.79% at the cutoff value of 4.09 cm. The maximum ovarian volume showed sensitivity of 85.00% and a specificity of 26.09% at a cutoff value of 3.5 mL. The U/C ratio showed a sensitivity of 68.00% and a specificity of 45.10% at the cutoff value of 1.45. The uterine volume, the most predictive parameter for CPP in our study, showed a sensitivity of 64.18% and a specificity of 71.79% at the cutoff value of 3.30 mL (Table 3, Fig. 1).
The GnRH stimulation test performed in girls with early symptoms of puberty compared to their chronological age, such as a marked increase in bone age and development in the breast region, is regarded as the gold standard for a diagnosis of CPP. However, this test takes a long time because blood collection has to be performed several times. Moreover, this test has a relatively high cost and low sensitivity, despite its high specificity. The reason for the low sensitivity is that the predominant LH response generally progresses at a relatively later stage among patients with precocious puberty.910 Meanwhile, pelvic ultrasonography is a useful tool for female organ measurement inside the pelvis. It is noninvasive and relatively easy to use. Moreover, abnormalities inside the uterus can be directly identified. In fact, in this study, one child was diagnosed with a unilateral ovarian mature teratoma and another girl was diagnosed with Mayer-Rokitansky-Küster-Hauser syndrome. Owing to these advantages, a number of studies have confirmed the potential of ultrasonography as an alternative to blood tests in the diagnosis of precocious puberty in girls. In a comparison of parameters before and after puberty in a patient group stratified according to age and puberty stage, each parameter in the pelvic ultrasonography showed a repetitive pattern, making it difficult to set an accurate cutoff value.1112 In this study, we performed a statistical analysis by using data from two groups including a target group of patients in a relatively simplified puberty stage classification (CPP or ET) to examine the effectiveness of ultrasonography. The study results indicated a significant difference in uterine volume.
However, a logistic regression analysis of the ultrasonographic measures of this study did not confirm the variables that significantly affected CPP progress. There may be several reasons for this. One of the possibilities is the lack of variables for forming a proper regression model. Buzi et al. suggested a specific standard according to the shape and size of the follicle in the ovary (solid, microcystic, paucicystic, multicystic, and macrocystic) as another index for expressing the stage of puberty progression.13 In addition, uterine morphology is considered to be another reliable marker of progression of puberty in a few studies.141516 Before puberty, the uterus has a tubular shape with a funfundus/cervix ratio of around 1. At the start of puberty, the development of the fundus becomes prominent owing to hormonal influences, resulting in an increase in the fundus/cervix ratio (>1). Because of this, adding another variable would help to form an accurate regression model that is closer to reality. However, in the imaging study performed in our hospital, the relevant item was omitted from the ultrasonographic evaluation owing to technical problems. Hence, diversification of the ultrasonography items is be an important task for future study.
Regarding the cutoff value for the clinical application of pelvic ultrasonography, Haber et al. suggested a cutoff value with high sensitivity and specificity, with a uterine volume cutoff value of 1.8 mL, ovarian volume of 1.2 mL, and uterine length of 3.6 cm.2 De Vries et al. suggested a uterine volume cutoff value of 2.0 mL, with 88.8% sensitivity and 89.4% specificity, and a uterine length cutoff value of 3.4 cm, with 80.2% sensitivity and 57.8% specificity.7 Binay et al. suggested a uterine length cutoff value of 3.0 cm (93.1% sensitivity, 86.6% specificity) and an ovarian volume cutoff value of 1.3 mL (72.7% sensitivity, 90.0% specificity).17 In our study, uterine length showed 33.33% sensitivity and 79.79% specificity in the case of a cutoff value of 4.09 cm. Uterine volume showed 64.18% sensitivity and 71.79% specificity in the case of a 3.3-mL cutoff value, and ovarian volume showed 85.00% sensitivity and 26.09% specificity in the case of a 3.5-mL cutoff value. We hypothesized several reasons for these obvious differences.
First, being a retrospective study, the research goal was not accurately set at the stage of data collection. Many patients had only a partial record of pelvic ultrasound findings, so despite the large number of patients who could have been included in the study, the number of patients who were finally included in the statistical analysis was greatly reduced. Patients in the early stage of ET tend to have undeveloped and small intrapelvic organs; thus, there is the possibility that the ultrasonographic parameters of these patients might be hard to measure and therefore that these patients were easily excluded from this study. On the basis of this supposition, we hypothesized that the majority of ET patients in our study were biased to the late stage. The incomprehensible result of several of the clinical characteristics of ET patients in this study being similar to, and for some parameters higher than, those of CPP patients could be explained by this hypothesis. Second, a normal, non- CPP patient group was not included as a control group. Ethnic and geographical differences could also cause the results to differ from previous data.
In this study, we found that uterine volume showed a meaningful difference between the two groups. However, the cutoff values obtained through ROC curves were quite different from those of previously published studies and showed considerably low sensitivity and specificity, making it difficult to use these as diagnostic criteria in practice. Although the use of ultrasonography as a diagnostic criterion has a number of advantages for children, pelvic ultrasound should be performed by expert practitioners and in combination with clinical and laboratory tests to maximize their diagnostic value for CPP. Additional effort could also be made to establish geographic and ethnic characteristics of pelvic ultrasonographic parameters in Korean girls with CPP.
Figures and Tables
FIG. 1
Receiver operator characteristic curves of pelvic ultrasonographic measurements for the diagnosis of central precocious puberty for uterine length, uterine volume, maximum ovarian volume and uterus/cervix ratio.
References
1. Garibaldi LR, Aceto T Jr, Weber C. The pattern of gonadotropin and estradiol secretion in exaggerated thelarche. Acta Endocrinol (Copenh). 1993; 128:345–350.

2. Pescovitz OH, Hench KD, Barnes KM, Loriaux DL, Cutler GB Jr. Premature thelarche and central precocious puberty: the relationship between clinical presentation and the gonadotropin response to luteinizing hormone-releasing hormone. J Clin Endocrinol Metab. 1988; 67:474–479.

3. Stanhope R. Premature thelarche: clinical follow-up and indication for treatment. J Pediatr Endocrinol Metab. 2000; 13:Suppl 1. 827–830.

4. Stanhope R, Brook CC. Thelarche variant: a new syndrome of precocious sexual maturation? Acta Endocrinol (Copenh). 1990; 123:481–486.

5. Schwarz HP, Tschaeppeler H, Zuppinger K. Unsustained central sexual precocity in four girls. Am J Med Sci. 1990; 299:260–264.
6. Herter LD, Golendziner E, Flores JA, Moretto M, Di Domenico K, Becker E Jr, et al. Ovarian and uterine findings in pelvic sonography: comparison between prepubertal girls, girls with isolated thelarche, and girls with central precocious puberty. J Ultrasound Med. 2002; 21:1237–1246.
7. de Vries L, Horev G, Schwartz M, Phillip M. Ultrasonographic and clinical parameters for early differentiation between precocious puberty and premature thelarche. Eur J Endocrinol. 2006; 154:891–898.

9. Haber HP, Wollmann HA, Ranke MB. Pelvic ultrasonography: early differentiation between isolated premature thelarche and central precocious puberty. Eur J Pediatr. 1995; 154:182–186.

10. Aritaki S, Takagi A, Someya H, Jun L. A comparison of patients with premature thelarche and idiopathic true precocious puberty in the initial stage of illness. Acta Paediatr Jpn. 1997; 39:21–27.

11. Salardi S, Orsini LF, Cacciari E, Partesotti S, Brondelli L, Cicognani A, et al. Pelvic ultrasonography in girls with precocious puberty, congenital adrenal hyperplasia, obesity, or hirsutism. J Pediatr. 1988; 112:880–887.

12. Herter LD, Golendziner E, Flores JA, Becker E Jr, Spritzer PM. Ovarian and uterine sonography in healthy girls between 1 and 13 years old: correlation of findings with age and pubertal status. AJR Am J Roentgenol. 2002; 178:1531–1536.

13. Buzi F, Pilotta A, Dordoni D, Lombardi A, Zaglio S, Adlard P. Pelvic ultrasonography in normal girls and in girls with pubertal precocity. Acta Paediatr. 1998; 87:1138–1145.

14. Ziereisen F, Guissard G, Damry N, Avni EF. Sonographic imaging of the paediatric female pelvis. Eur Radiol. 2005; 15:1296–1309.

15. Haber HP, Mayer EI. Ultrasound evaluation of uterine and ovarian size from birth to puberty. Pediatr Radiol. 1994; 24:11–13.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download