Abstract
Purpose
This study aimed to investigate the optimal withdrawal time (WT) for initial surveillance colonoscopy after curative resection for colorectal cancer (CRC) by comparing anterior/low anterior resection (AR/LAR) and right hemicolectomy (RHC) groups.
Methods
This retrospective study analyzed 1,212 patients who underwent initial surveillance colonoscopy after CRC resection between 2015 and 2022. The patients were divided into the AR/LAR (n = 846) and RHC (n = 366) groups. The optimal WT was determined using receiver operating characteristic curve analysis and validated using logistic regression models. The adenoma and advanced neoplasia detection rates (ADR/ANDR) were evaluated based on the optimal WT.
Results
The optimal WT was 7 and 6 minutes in the AR/LAR and RHC groups, respectively. In multivariate analysis, WT ≥7 and ≥6 minutes in the AR/LAR (odds ratio [OR], 2.38; 95% confidence interval [CI], 1.75–3.24; P < 0.001) and RHC (OR, 2.64; 95% CI, 1.59–4.39; P = 0.001) groups, respectively, were significant factors for adenoma detection. In the AR/LAR group, ADR was 41.5% for WT ≥7 minutes compared to 21.9% for WT <7 minutes (P < 0.001). In the RHC group, ADR for WT ≥6 minutes was 33.9% compared to 15.8% for WT <6 minutes (P < 0.001). The ANDR also significantly improved with longer WTs in both groups.
Conclusion
This study suggests that a minimum WT of 7 and 6 minutes for AR/LAR and RHC patients, respectively, during the initial surveillance colonoscopy after CRC resection is optimal for maintaining a satisfactory ADR and ANDR. These findings highlight the importance of tailoring colonoscopic procedures according to the type of surgical resection.
Colorectal cancer (CRC) remains a significant global health concern, with surveillance colnoscopy playing a crucial role in improving survival rates after curative resection [12]. Studies have shown that over 50% of all metachronous CRCs are detected within 3 years of surgery [3]. Thus, early surveillance colonoscopy, which typically begins within the first year after surgery, is particularly important [4].
Withdrawal time (WT) is a critical factor in determining the colonoscopy quality. For standard screening colonoscopies, a minimum WT of 6 minutes is widely recommended, as it has been associated with higher adenoma detection rates (ADR) [5]. However, the optimal WT for postsurgical surveillance colonoscopy remains unclear, especially considering the altered colonic anatomy following resection. The colon-sidedness of right- and left-sided CRC exhibits distinct characteristics in terms of demographics, molecular features, and prognosis [6]. In addition to the different status of the remaining colon after surgery, the different nature of the polyps, including the smaller and sessile morphology found in the right-sided colon, may require more meticulous examination during colonoscopy [7].
This study aimed to investigate the optimal WT for initial surveillance colonoscopy after curative resection for CRC. The patients were categorized into 2 groups based on their surgical procedures: anterior/low anterior resection (AR/LAR) and right hemicolectomy (RHC). This approach considers the potential differences in the remaining colon length, characteristics, and impact of colon-sidedness on surveillance outcomes. The primary objective was to determine the optimal WT for each surgical group and to evaluate its impact on the ADR and advanced neoplasia detection rate (ANDR). By focusing on different surgical treatments, we aimed to provide tailored recommendations that could contribute to performing more effective surveillance colonoscopy in CRC, considering the anatomical and physiological changes resulting from different surgical procedures.
The Institutional Review Board of the Korea University Guro Hospital approved the ethical clearance of this study (No. 2024GR0214). This study was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
A retrospective analysis was performed on patients who underwent their first surveillance colonoscopy following curative resection for CRC without distant metastases between January 2015 and December 2022 in a tertiary referral hospital. The following information was collected: age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) grade, TNM stage based on the American Joint Committee on Cancer Manual (8th edition), and surgical name. Data regarding the initial surveillance colonoscopy were gathered, including the proportion of sedation, bowel preparation scale, time after surgery, and time records of the colonoscopy procedures. Pathological reports of polypectomy were gathered, including polyp or ADRs, mean number of detected polyps, size of the largest polyp, and name of the diagnosis. Patients who did not receive a complete assessment of the entire colon prior to surgery due to obstruction or perforation, and for whom data on the preoperative colonoscopy was not available were excluded from this study. Patients with “poor” or “inadequate” bowel preparation at the initial surveillance colonoscopy were also excluded. Furthermore, patients who underwent total colectomy, subtotal colectomy, left hemicolectomy, or transverse colectomy were excluded. Patients were classified into 2 groups based on the surgical treatment received: AR/LAR and RHC.
Colonoscopies were conducted by 2 board certificated colorectal surgeons specializing in colonoscopy. The results of general colonoscopy performed by these endoscopists, not surveillance colonoscopy after CRC surgery, are shown in Supplementary Table 1. Bowel preparation was performed using either 4-L polyethylene glycol or oral sulfate tablets (sodium sulfate, potassium sulfate, and magnesium sulfate). The quality of bowel preparation was measured using the Aronchick scale (“inadequate,” “poor,” “fair,” “good,” and “excellent”) by the endoscopists. Conscious sedation was selectively induced using intravenous midazolam and propofol. Insertion time was defined as the time from the anus to the cecum or ileocolic anastomosis. WT was defined as the duration from the cecum or ileocolic anastomosis to the anus, omitting the time spent on polypectomy. Under the guidance of endoscopists, trained nurses recorded the time data at designated locations. Data on the characteristics of the polyps, such as number, size, and diagnosis, were collected based on histological and pathological findings. Advanced neoplasia included polyps of ≥1 cm, dysplasia, tubulovillous adenoma, villous adenoma, and cancer. Non-advanced adenomas included adenomas of <1 cm and no dysplasia or villous morphology.
The primary endpoint was optimal WT for adenoma detection in the AR/LAR and RHC groups. The secondary endpoint was the ADR and ANDR of the 2 groups according to the optimal WT. ADR was calculated by dividing the number of patients who had at least 1 adenoma by the total number of patients. ANDR was calculated by dividing the number of patients with advanced neoplasia by the total number of patients.
The Student t-test was used to assess the differences in continuous variables, including the interval after surgery, procedure time, and number and size of polyps. The chi-square test or Fisher exact test was used for discrete variables, including age, sex, BMI, ASA grade, cancer stage, sedation, bowel preparation scales, and rates of lesion detection. The receiver operating characteristic (ROC) curve was plotted and the area under the ROC curve (AUC) was evaluated to determine the optimal cutoff value of WT for adenoma detection. The optimal WT was validated using 2 methods using the logistic regression model. First, univariate and multivariate logistic regression analyses were performed to analyze the association between optimal WT and adenoma detection. Second, to analyze the dose-response relationship between WT and adenoma detection, restricted cubic spline (RCS) models fitted from the logistic regression model were used to adjust for significant variables in the multivariate analysis. Two-sided P-values of <0.05 were considered statistically significant. All statistical analyses were performed using the pROC and rms packages in the R software ver. 4.2.2 (The R Foundation).
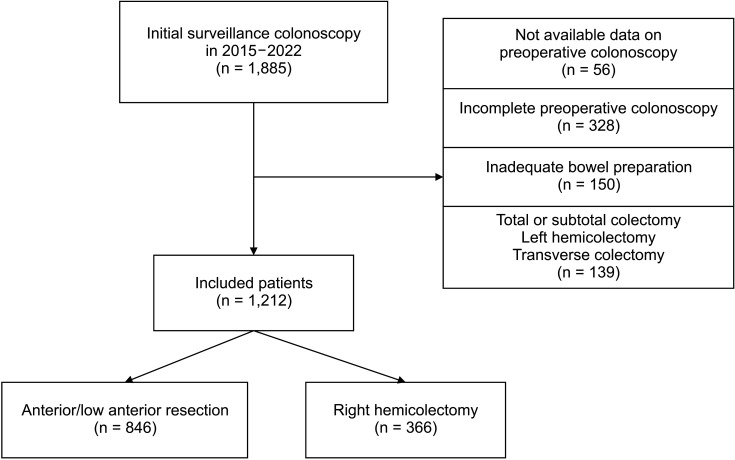
A total of 1,885 individuals who underwent initial surveillance colonoscopies following curative resections for CRC were included in this study (Fig. 1). After excluding 673 patients who had incomplete preoperative colonoscopy (n = 328), inadequate bowel preparation (n = 150), surgery other than AR/LAR or RHC (n = 139), and unavailable data on preoperative colonoscopy (n = 56), 1,212 patients (846 in the AR/LAR group and 366 in the RHC group) were included in this study. Table 1 compares the clinical characteristics of the 2 groups. The proportion of patients aged ≥75 years was higher in the RHC group compared to the AR/LAR group (n = 78, 21.3% vs. n = 130, 15.4%; P = 0.015). The AR/LAR group had a higher prevalence of male patients than the RHC groups (n = 538, 63.6% vs. n = 180, 50.3%; P < 0.001). The proportion of patients with stages 0 and I disease was higher in the AR/LAR groups than in the RHC group (n = 347, 41.0% vs. n = 123, 33.6%; P = 0.002).
There was no significant difference in the average intervals from surgery to the initial surveillance colonoscopy between the AR/LAR and RHC groups (1.08 ± 0.13 years and 1.06 ± 0.08 years, respecively; P = 0.438). The use of conscious sedation was more common in the RHC group than in the AR/LAR group (n = 70, 19.1% vs. n = 100, 11.8%; P = 0.001). The RHC group had a higher proportion of patients with “excellent” or “good” bowel preparation compared to the AR/LAR group (n = 299, 81.7% vs. n = 625, 73.9%; P = 0.004). The average insertion time in the RHC group was greater than that in the AR/LAR group (10.7 ± 6.8 minutes vs. 6.5 ± 4.9 minutes, P < 0.001). The average WT in the RHC group was 6.4 ± 2.1 minutes, which was less than the average WT in the AR/LAR group (7.8 ± 3.1 minutes, P < 0.001).
The percentage of patients who underwent polypectomies was higher in the AR/LAR group than in the RHC group (n = 329, 38.9% vs. n = 114, 31.1%; P = 0.012). The AR/LAR group had a higher number and larger size of polyps compared to the RHC group (n = 0.8 ± 1.4 and 0.7 ± 0.4 cm vs. n = 0.5 ± 0.9 and 0.6 ± 0.4 cm; P < 0.001 and P = 0.043, respectively). The ADR in the AR/LAR group was higher than that in the RHC group (n = 274, 32.4% vs. n = 92, 25.1%; P = 0.014). The ratio of advanced neoplasia in the AR/LAR group was not significantly different compared to that in the RHC group (n = 75, 8.9% vs. n = 23, 6.3%; P = 0.162).
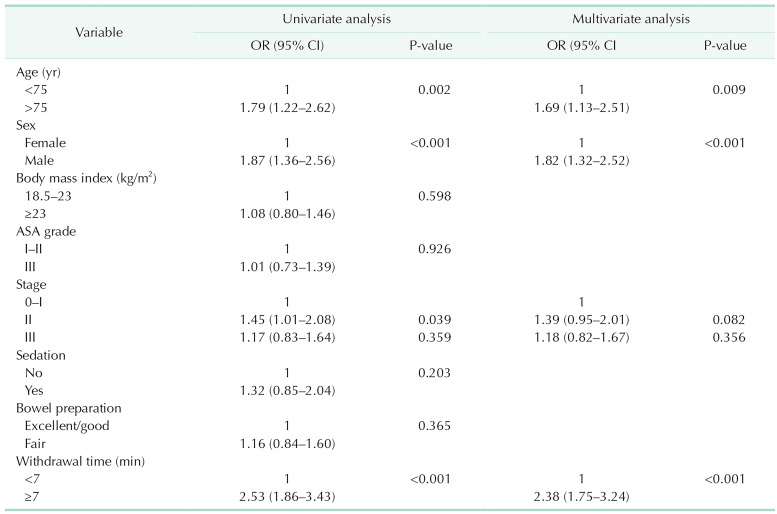
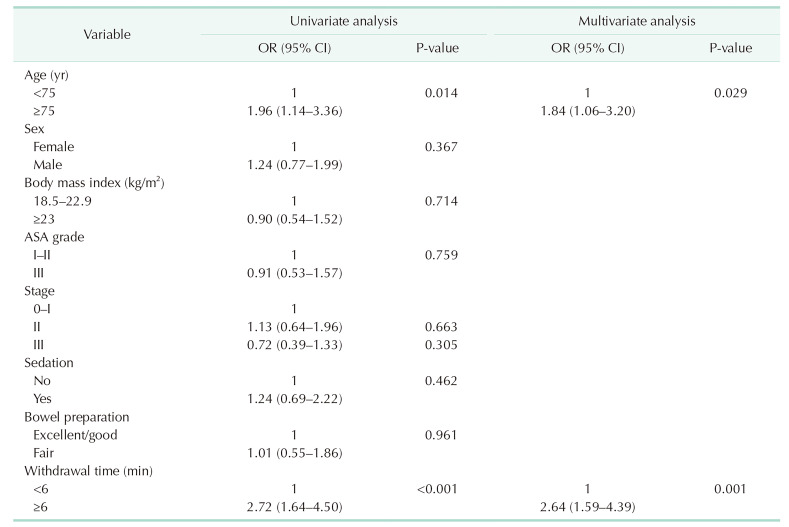
After plotting the ROC curve for WT and adenoma detection, the optimal cutoff value of WTs was analyzed as 7.05 minutes in the AR/LAR group (AUC, 0.647) and 6.05 minutes in the RHC group (AUC, 0.641) (Fig. 2). In the multivariate analysis for adenoma detection, older age of ≥75 years (odds ratio [OR], 1.69; 95% confidence interval [CI], 1.13–2.51; P = 0.009), male sex (OR, 1.82; 95% CI, 1.32–2.52; P < 0.001), and WT ≥7 minutes (OR, 2.38; 95% CI, 1.75–3.24; P < 0.001) were significant factors in the AR/LAR group (Table 2). Older age of ≥ 5 years (OR, 1.84; 95% CI, 1.06–3.20; P = 0.029) and WT ≥6 minutes (OR, 2.64; 95% CI, 1.59–4.39; P = 0.001) were significant factors for adenoma detection in the RHC group (Table 3). In the AR/LAR group, after adjusting for significant covariates, including age and sex, the RCS model showed a strong positive correlation between WT and adenoma detection in both linear (P < 0.001) and nonlinear (P = 0.014) patterns (Fig. 3). When WT reached or exceeded 7 minutes, the OR for adenoma detection increased significantly. In the RHC group, when the RCS model was adjusted for age, there was a linear relationship between WT and adenoma detection (linear, P < 0.001; nonlinear, P = 0.087). When the WT reached at least 6 minutes, the OR for adenoma detection in the RHC group gradually increased.
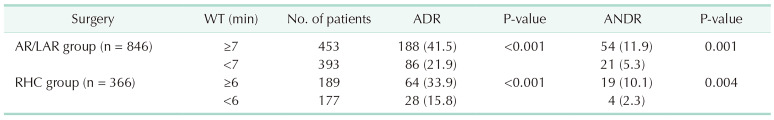
When the patients in the AR/LAR group were divided into WT ≥7 minutes (n = 453) and WT <7 minutes (n = 393) groups, ADRs were 41.5% (n = 188) and 21.9% (n = 86), respectively (P < 0.001) (Table 4). ANDRs of the AR/LAR group were 11.9% (n = 54) and 5.3% (n = 21) in the WT ≥7 minutes and WT <7 minutes groups, respectively (P = 0.001). In the RHC groups, ADRs were 33.9% (n = 64) in the WT ≥6 minutes (n = 189) group and 15.8% (n = 28) in the WT <6 minutes (n = 177) group (P < 0.001). In addition, ANDRs of the RHC group were 10.1% (n = 19) and 2.3% (n = 4) in the WT ≥6 minutes and WT <6 minutes groups, respectively (P = 0.004).
This study examined the optimal WT for the first surveillance colonoscopy following curative resection of both right- and left-sided CRC. ROC analysis revealed that the ideal WTs for the AR/LAR and RHC groups were 7 and 6 minutes, respectively. The cutoff values were evaluated using logistic regression models and were found to be appropriate for maintaining asatisfactory ADR and ANDR. Therefore, it is advisable to maintain a minimum WT of 6 minutes for initial surveillance colonoscopy following curative resection for CRC, even ifthe length of the colon is reduced after surgery. Furthermore, for patients who underwent AR or LAR, the minimum WT should be extended to 7 minutes.
WT during colonoscopy is crucial to the quality and efficacy of the procedure [8]. This refers to the time at which the colon is thoroughly examined and the endoscope is gradually withdrawn. This is important for detecting polyps and other abnormalities. A landmark study by Barclay et al. [5] demonstrated that endoscopists with a mean WT of ≥6 minutes had higher ADRs compared to those with shorter WTs. This finding was replicated in subsequent research, leading to the current recommendation of a minimum 6-minute WT for colonoscopies. Studies have shown that longer WTs are associated with a higher ADR and detection of precancerous lesions. Aziz et al. [9] performed a meta-analysis of 3 randomized controlled trials on the optimal WT during colonoscopy and reported that the 9-minute WT improved the ADR and adenoma per colonoscopy rate compared with the 6-minute WT. The authors recommended that a minimum 9-minute WT is required to improve colonoscopy quality. However, another prospective cohort study found that when WT was >8 minutes, the adenoma detection OR no longer changed significantly after a WT of >8.24 minutes [10]. The authors of this study acknowledged that although there is a direct correlation between the length of the WT and ADR, longer procedures would lead to increased patient discomfort and decreased colonoscopy efficiency. Therefore, determining the optimal WT is important to perform colonoscopies more efficiently.
The surveillance colonoscopy plays an essential part in enhancing the survival rates of patients with CRC following surgery [11]. Early surveillance colonoscopy within 3 years after surgery is advisable because the cumulative incidence of non-anastomotic recurrence during this period is reported to be approximately 53.7% of all non-anastomotic recurrences [3]. Furthermore, a study conducted using population-based data from the Netherlands Cancer Registry revealed that over 43% of all metachronous CRCs occurring within 3 years were classified as missed lesions prior to surgery [12]. The proportion of anastomotic CRCs that occurred within the first year following surgery was 1.7% of all anastomotic CRCs [3]. Therefore, it is generally recommended to conduct an initial surveillance colonoscopy within 1 year after surgery to clear metachronous and missed lesions during the perioperative period.
The optimal WT for initial surveillance colonoscopy in patients with CRC should be determined, considering both the reduced colon length after resection and the time needed to detect all metachronous and missed lesions. Jung et al. [13] previously investigated the relationship between WT and ADR during surveillance colonoscopy after CRC surgery. The researchers found that a WT of ≥8 minutes had significantly higher ADRs compared to shorter WTs (49.1% vs. 32.2%, P < 0.001). The study concluded that thorough observation with 8–10 minutes of WT is necessary for optimal adenoma detection in postoperative surveillance colonoscopy, despite the shorter colon length due to surgery. They also identified a positive linear relationship between the WT and ADR, which is consistent with our results. In addition, they showed similar results to our study for average polyp sizes (Jung et al. [13], 6.0 mm; current study, 6.5 mm) and average ANDR (Jung et al. [13], 7.6%; current study, 8.0%). However, there are several differences. First, Jung et al.’s study [13] included multiple endoscopists (8), resulting in significant variability in average WT (6.4–10.9 minutes) and ADR (29.3%–50.6%). In contrast, our study included only 2 endoscopists, which contributed to data consistency and uniformity. Second, the optimal WT determined by ROC curve analysis in the study by Jung et al. [13] was 7.8 minutes, which was longer than that in our study. This difference could be attributed to the Jung group’s longer average WT of 8.1 minutes compared to our 7.3 minutes. Lastly, while Jung et al. [13] did not analyze WT according to the type of surgery, our study categorized all patients into 2 groups based on their surgical treatment: the AR/LAR and RHC groups. Patients who underwent AR/LAR or RHC were analyzed independently because of potential variations in the characteristics of the residual colon. Mostpatients with AR/LAR have the remaining colonlocated on the right side, whereas patients with RHC have the colon primarilyon the left side. The anatomical structures of the right- and left-sided colons differ, and the features of polyps that dominate the right side are distinct from those that dominate the left side [7]. Therefore, we separately evaluated the optimal WTs of patients with AR/LAR and RHC to identify differences in initial surveillance colonoscopy.
In our study, colonoscopy results differed between right- and left-sided CRC. The polypectomy detection rate and ADR in the AR/LAR group were higher than those in the RHC group (38.9% and 32.4% vs. 31.1% and 25.1%; P = 0.021 and P = 0.014, respectively). The mean WT (7.8 ± 3.1 minutes) and optimal WT (7.05 minutes) of the AR/LAR group were longer than those of the RHC group (6.4 ± 2.1 minutes and 6.05 minutes, respectively). Additionally, when each group was divided into subgroups based on the cutoff value of optimal WT (7.05 in the AR/LAR group and 6.05 in the RHC group), there was a significant difference in ANDR between subgroups within each group. In the AR/LAR group, the subgroup with a WT ≥7 minutes had an ANDR of 11.9%, which was twice as high as the subgroup with a WT <7 minutes (P = 0.001). Furthermore, within the RHC group, the incidence of ANDR in the subgroup with a WT ≥6 minutes was 10.2%, which was 4 times greater than the incidence in the subgroup with a WT <6 minutes (P = 0.004). Thus, to perform initial surveillance colonoscopy more efficiently, it is advisable to adhere to the optimal WTs according to the surgical treatments and consider other factors in patients with CRC.
The longer optimal WT and higher ADR in the AR/LAR group than those in the RHC group could be attributed to anatomical differences and surgical techniques. Central vessel ligation, a common technique for improving oncological outcomes, results in a considerably fixed range of resected colons for RHC, whereas surgeons have more flexibility in determining the extent of resection for AR/LAR. In addition, the length of the resected colon is generally longer for right-sided tumors than for left-sided tumors, potentially explaining the higher ADR and WT in the AR/LAR group [1415]. Moreover, right-sided polyps tend to be smaller and more sessile, making them harder to detect during colonoscopy, whereas left-sided polyps are generally larger and pedunculated [1617]. These anatomical differences necessitate careful examination to thoroughly detect and manage polyps in the right-sided colon, thereby contributing to the longer WT in the AR/LAR group. In addition, the right-sided colon is the largest part of the colon and has a saccular morphology with tangential trabecula [18]. This large diameter and distinct structure can pose challenges during colonoscopy, necessitating careful maneuvering to avoid complications. Right-sided polyp location has been reported as a significant risk factor for major complications, including bleeding and perforation, during colonoscopic polypectomy [19]. Thus, the larger diameter and specific anatomical features of the right colon increase the complexity and risks associated with polypectomy, resulting in a longer WT in the AR/LAR group.
In addition to WTs, several additional characteristics, such as advanced age, male sex, obesity, and insufficient bowel preparation, significantly affect the enhancement ofADR during colonoscopy [202122]. In our study, the effect of bowel preparation could not be evaluated because we excluded patients with “poor” and “inadequate” bowel preparation. BMI was not a significant factor in either the AR/LAR or RHC groups. However, older age and male sex were significantly associated with ADR in both groups. In the multivariate analysis, older age (≥75 years) was a significant factor in both groups. Male sex was found to have a significant association with higher ADR in the AR/LAR group but not in the RHC group. This difference may be attributed to the small number of patients in the RHC group.
This study has some limitations. First, the retrospective design of the study could have led to a bias in data selection between the AR/LAR and RHC groups. Second, because of the significant dependence on the technical expertise of endoscopists, it is essential to validate the findings of this study by integrating a greater number of endoscopists and collecting data from multiple centers. Third, the WT was calculated by excluding the time spent on polypectomy; however, it was impossible to exclude the time spent on suctioning the luminal fluid or contents. Thus, data from colonoscopies with “fair” bowel preparation may have influenced the analytical outcomes.
In conclusion, this study suggests that a minimum WT of 7 minutes for AR/LAR patients and 6 minutes for RHC patients are optimal for maintaining a satisfactory ADR and ANDR. These findings emphasize the importance of tailoring colonoscopy procedures based on the type of surgical resection performed, potentially leading to more effective detection of metachronous lesions and improved treatment outcomes for patients with CRC.
Notes
References
1. Baik SM, Lee RA. National cancer screening program for colorectal cancer in Korea. Ann Surg Treat Res. 2023; 105:333–340. PMID: 38076601.

2. Lautenbach E, Forde KA, Neugut AI. Benefits of colonoscopic surveillance after curative resection of colorectal cancer. Ann Surg. 1994; 220:206–211. PMID: 8053743.
3. Fuccio L, Rex D, Ponchon T, Frazzoni L, Dinis-Ribeiro M, Bhandari P, et al. New and recurrent colorectal cancers after resection: a systematic review and metaanalysis of endoscopic surveillance studies. Gastroenterology. 2019; 156:1309–1323. PMID: 30553914.

4. Kahi CJ, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, et al. Colonoscopy surveillance after colorectal cancer resection: recommendations of the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2016; 111:337–346. PMID: 26871541.

5. Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006; 355:2533–2541. PMID: 17167136.

6. Petrelli F, Tomasello G, Borgonovo K, Ghidini M, Turati L, Dallera P, et al. Prognostic survival associated with left-sided vs right-sided colon cancer: a systematic review and meta-analysis. JAMA Oncol. 2017; 3:211–219. PMID: 27787550.
7. Yang JF, Noffsinger AE, Agrawal D, Yang QH. Colorectal cancer anatomic distribution patterns remain the same after sessile serrated adenoma/polyp considered cancer precursor: a 9-year comparison study from community-based endoscopy centers. J Gastrointest Oncol. 2016; 7:917–923. PMID: 28078114.

8. Shin R, Lee S, Han KS, Sohn DK, Moon SH, Choi DH, et al. Guidelines for accreditation of endoscopy units: quality measures from the Korean Society of Coloproctology. Ann Surg Treat Res. 2021; 100:154–165. PMID: 33748029.

9. Aziz M, Haghbin H, Gangwani MK, Nawras M, Nawras Y, Dahiya DS, et al. 9-Minute withdrawal time improves adenoma detection rate compared with 6-minute withdrawal time during colonoscopy: a meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2023; 57:863–870. PMID: 37389958.

10. Zhao M, Xu Y, Zhu H, Chen J, Sun W, Yang D, et al. A prospective cohort study of the relationship between the withdrawal time and the detection rate of colorectal adenoma. Scand J Gastroenterol. 2022; 57:1131–1137. PMID: 35465795.
11. Rusiecki J, Cifu AS. Colonoscopy surveillance after colorectal cancer resection. JAMA. 2017; 318:2346–2347. PMID: 29260211.

12. le Clercq CM, Winkens B, Bakker CM, Keulen ET, Beets GL, Masclee AA, et al. Metachronous colorectal cancers result from missed lesions and non-compliance with surveillance. Gastrointest Endosc. 2015; 82:325–333. PMID: 25843613.

13. Jung DH, Lee JI, Huh CW, Kim MJ, Youn YH, Choi YH, et al. Withdrawal time of 8 minutes is associated with higher adenoma detection rates in surveillance colonoscopy after surgery for colorectal cancer. Surg Endosc. 2021; 35:2354–2361. PMID: 32440929.

14. Bostanci MT, Yilmaz I. Surgical resection length and harvested lymph nodes in colon cancer. J Coll Physicians Surg Pak. 2021; 31:798–804. PMID: 34271779.
15. Üstüner MA, Aksel B, Dogan L. The minimum length of colonic segment to be removed for adequate lymph node dissection in colorectal cancer. Hellenic J Surg. 2020; 92:110–114.

16. Gupta S, Balasubramanian BA, Fu T, Genta RM, Rockey DC, Lash R. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012; 10:1395–1401. PMID: 22835574.

17. Montgomery E. Serrated colorectal polyps: emerging evidence suggests the need for a reappraisal. Adv Anat Pathol. 2004; 11:143–149. PMID: 15096728.
18. Bartolí R, Boix J, Odena G, De la Ossa ND, de Vega VM, Lorenzo-Zúñiga V. Colonoscopy in rats: an endoscopic, histological and tomographic study. World J Gastrointest Endosc. 2013; 5:226–230. PMID: 23678375.
19. Heldwein W, Dollhopf M, Rösch T, Meining A, Schmidtsdorff G, Hasford J, et al. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy. 2005; 37:1116–1122. PMID: 16281142.

20. Maratt JK, Dickens J, Schoenfeld PS, Elta GH, Jackson K, Rizk D, et al. Factors associated with surveillance adenoma and sessile serrated polyp detection rates. Dig Dis Sci. 2017; 62:3579–3585. PMID: 29043592.

21. Mitsuhashi S, Azari J, Dioguardi V, Bilello J, Tang M, Kastenberg D. Age matters: adenoma detection rates in average-risk screening patients aged 45 to 49 compared with those aged 50 to 54. J Clin Gastroenterol. 2024; 58:896–901. PMID: 38059772.
22. Zhou W, Yao L, Wu H, Zheng B, Hu S, Zhang L, et al. Multi-step validation of a deep learning-based system for the quantification of bowel preparation: a prospective, observational study. Lancet Digit Health. 2021; 3:e697–e706. PMID: 34538736.
SUPPLEMENTARY MATERIALS
Supplementary Table 1 can be found via https://doi.org/10.4174/astr.2024.107.4.212.
Supplementary Table 1
Clinical characteristics of general colonoscopy for the 2 colorectal surgeons
Fig. 2
Receiver operating characteristic (ROC) curves of the optimal withdrawal time for adenoma detection in different surgical treatment groups. (A) Anterior/low anterior resection (AR/LAR). (B) Right hemicolectomy (RHC). AUC, area under the ROC curve.
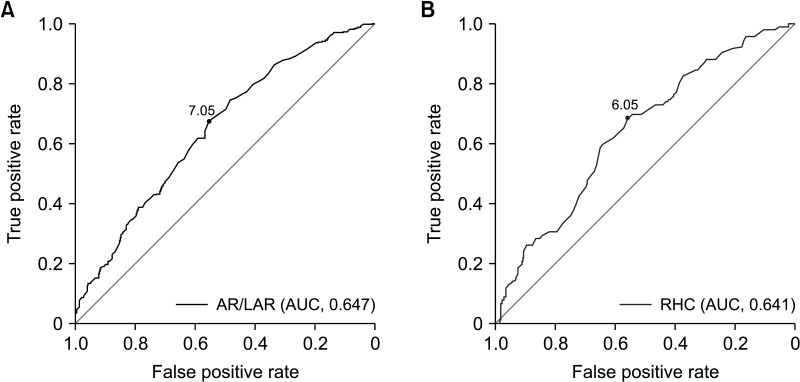
Fig. 3
Restricted cubic spline regression analysis for adenoma detection rate and withdrawal time of different surgical treatment groups. (A) Anterior/low anterior resection. Adjusted to age of <75 years and male sex. (B) Right hemicolectomy. Adjusted to age of <75 years. CI, confidence interval.
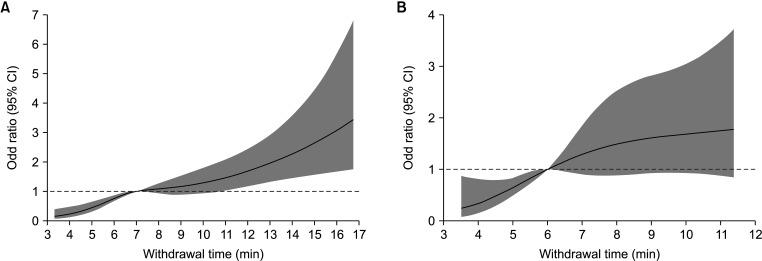
Table 1
Clinical characteristics of patients according to the surgical treatments
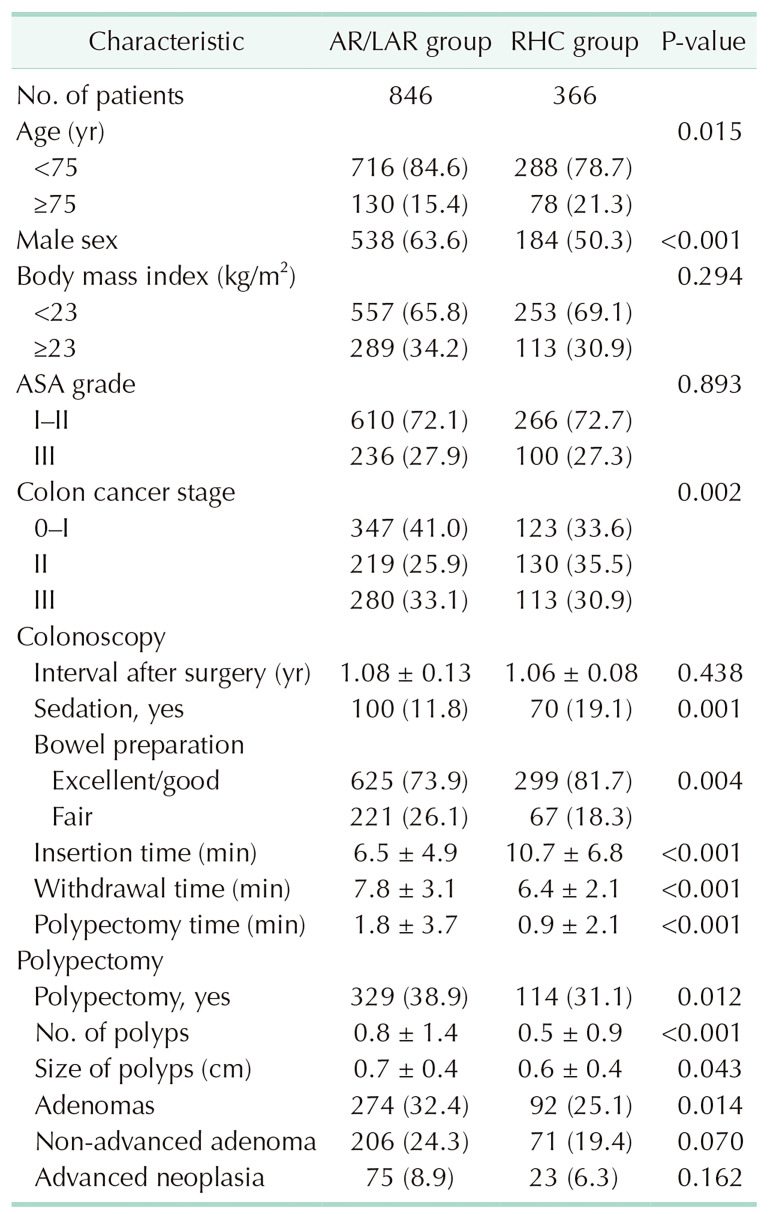
Values are presented as number only, number (%), or mean ± standard deviation.
AR/LAR, anterior resection/low anterior resection; RHC, right hemicolectomy; ASA, American Society of Anesthesiologists.
Advanced neoplasia: ≥1 cm in size, high-grade dysplasia, tubulovillous or villous adenoma, and cancer; non-advanced adenoma: <1 cm in size, without dysplasia and villous morphology.
Table 2
Univariate and multivariate analysis for adenoma detection in the anterior/low anterior resection group




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download