Treatment
- Treatment for scabies should be chosen based on factors such as age, clinical form, and overall health status. Additionally, close contacts should be treated simultaneously with the patient, irrespective of symptom presence.
- Topical 5% permethrin is the first-line treatment for both classic and crusted scabies. When the use of topical 5% permethrin is not feasible, alternative treatments include topical 10% crotamiton or oral ivermectin.
- Treatment is deemed unsuccessful if there is an exacerbation of pruritus, the emergence of new characteristic skin lesions such as burrows, or if mites continue to be detected after the treatment.
Table 1.
Drugs available in Korea for the treatment of scabies
Treatment of classic scabies
Topical 5% permethrin
Topical 10% crotamiton
Topical 5%–10% sulfur
Topical 1% lindane
Oral ivermectin
Treatment of crusted scabies
- The medications used to treat crusted scabies are similar to those for classic scabies; however, the frequency of application and dosage may differ.
- Due to is high transmissibility, isolation is recommended to prevent the risk of spreading the infection.
- While some cases of scabies are treated solely with topical permethrin, in countries where oral ivermectin is accessible and approved, it is often used concurrently. For crusted scabies that is resistant to topical permethrin alone, a combination of oral ivermectin and topical treatments may be considered. However, there are currently no standardized guidelines regarding the frequency and intervals of topical applications or their combination with oral medications for treating crusted scabies. Typically, permethrin ointment is applied daily for one week and then twice weekly until no mites or eggs are detected [9]. Ivermectin is administered on days 0, 1, 7, 8, and 14, with optional additional doses on days 21 and 28 [7]. The treatment regimens for ivermectin are categorized into three phases based on the severity of the symptoms of crusted scabies: Phase 1 includes days 0, 1, and 7; Phase 2 includes days 0, 1, 7, 8, and 14; Phase 3 includes days 0, 1, 7, 8, 14, 21, and 28 [8].
- The removal of the thick crust associated with crusted scabies aids in treatment. Consequently, keratolytic agents such as 5%–10% salicylic acid, 10% urea, and 5% lactic acid, which are not typically used in treating classic scabies, can be employed to enhance drug penetration and improve treatment efficacy.
- If secondary bacterial infections with organisms such as Streptococcus pyogenes or Staphylococcus aureus are present, appropriate antibiotics should be administered [9].
Precautions in scabies treatment
- Simultaneously treat individuals who have been in contact with or are cohabitating with a scabies patient.
- For classic scabies, thoroughly apply the medication from the neck down to the feet, covering all skin areas. This includes under the nails and in skin folds, such as the groin. After applying the medication, it should remain on the skin for an adequate period (at least 8 hours) before it is washed off.
- For infants, young children, and certain older adults with scalp or facial involvement, the treatment should be applied over the entire body, including the face and scalp.
- Wearing plastic gloves during application is recommended, as excessive absorption of the medication through the palms can cause numbness, tingling, or a stinging sensation.
Treatment failure
Treatment for children, pregnant women, and institutional outbreaks
Children
Pregnant and breastfeeding women
Treatment in institutional outbreaks
Table 2.
Summary of drugs for scabies treatment in children, pregnant and breastfeeding women
Scabies-related itching
- The itching associated with scabies can significantly affect quality of life and may continue for some time even after all mites have been eradicated. This necessitates proactive management from the onset.
- Moisturizers, oral antihistamines, and topical steroids can help alleviate itching associated with scabies.
Mechanism of itching in scabies patients
Treatment of itching in scabies patients
Prevention and infection control
- Scabies patients require contact precautions or isolation until 24 hours after the final application of treatment.
- Close contacts should receive a single preventive treatment, even if they are asymptomatic, and should then be monitored for the development of symptoms over a 6-week period.
- The patient's clothing, bedding, and linens must be laundered and dried using heat. Additionally, medical equipment and items, as well as the surrounding environment that the patient has touched, should be disinfected with alcohol or other standard methods.
- When a case of scabies is identified, it is essential to isolate the patient, manage contacts, and control the environment to prevent transmission (Table 3).
Table 3.
Recommended measures for scabies prevention
Patient contact precautions and isolation
Contact management
Environmental management
Conclusion
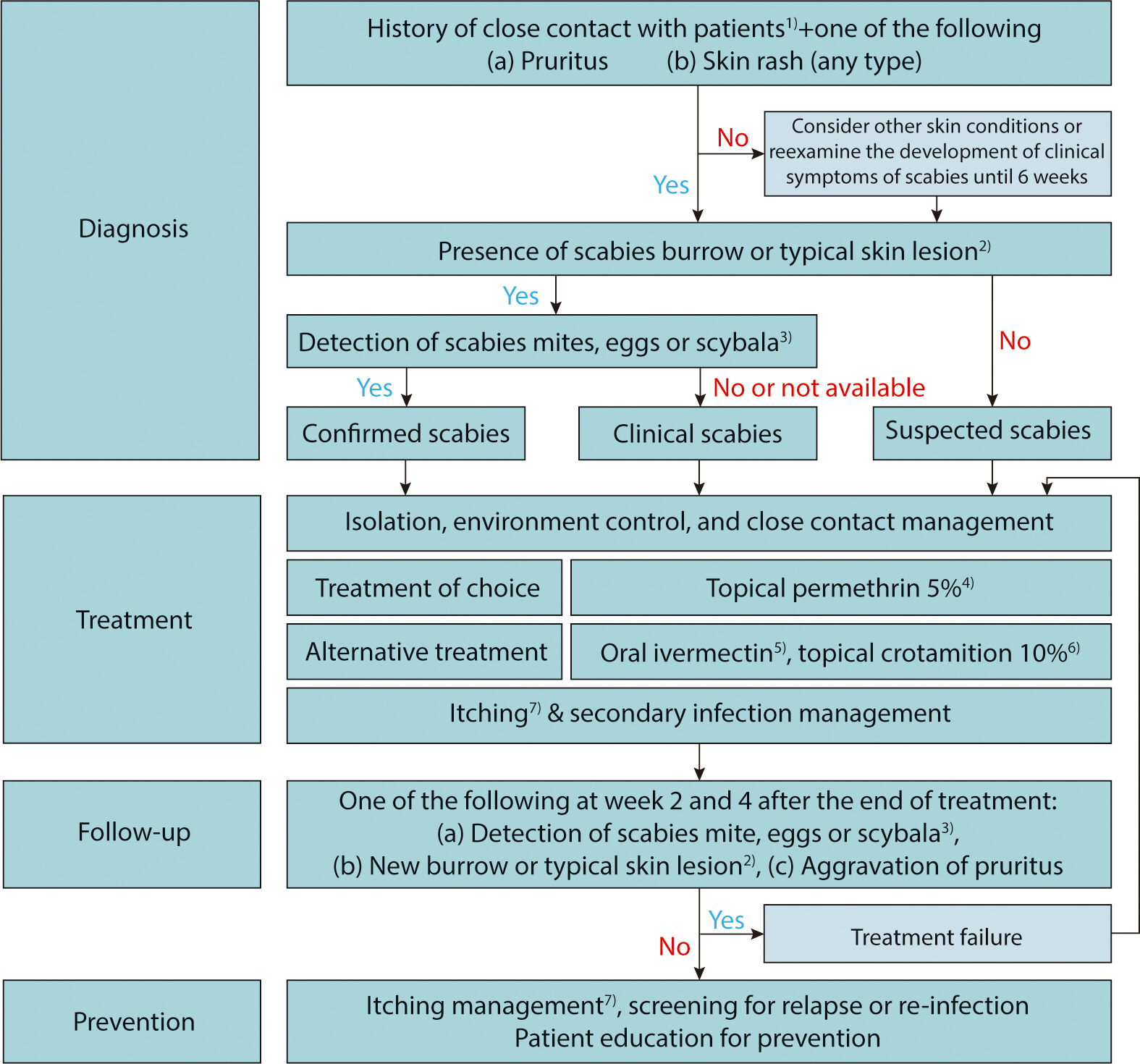
Fig. 1.
Proposed algorithm for the diagnosis and treatment of scabies in Korea. 1) One of the following: (a) Skin contact with an individual diagnosed with scabies, (b) sexual contact with an individual diagnosed with scabies (especially nodular scabies), (c) brief direct contact with linens (such as towels, clothing, and bedding) used by an individual diagnosed with scabies (especially crusted scabies); 2) One of the following: (a) Typical erythematous papules or vesicles in a typical distribution including the periumbilical area, inner thigh, buttock, axilla, inner forearm, (b) multiple nodules in genital area or axilla, (c) multiple papules, vesicles, or pustules in the palmoplantar distribution of an infant; 3) Light microscopy, dermoscopy, or other high-resolution imaging techniques including could be used; 4) In general, apply on the whole body, except the face and scalp, at least 30 minutes after taking a shower. For treatment of infants and older adults, it should be applied to the lesion on the scalp and face; the recommended doses are as follows: 25–30 g (1 tube) for adults, 15 g (1/2 tube) for ages 6–12 years, and up to 7.5 g (1/4 tube) for ages 2–5 years; cleansed out after at least 8–12 hours of application. Application is repeated after 7–10 days. For crusted scabies, 5% permethrin cream should be applied daily for a week, then twice weekly until any mite or egg is not identified. However, 5% permethrin cream is not permitted for use in patients aged <2 years and pregnant or lactating women in Korea; therefore, Centers for Disease Control and Prevention guidelines recommend using 5% permethrin cream in patients older than 2 months and pregnant or lactating women; 5) For classic scabies, the recommended dose is 200 μg/kg twice weekly; For crusted scabies, ivermectin is administered on days 0, 1, 7, 8, 14, 21, and 28. Safety in patients who are pregnant or weigh <15 kg is not established; 6) Apply repeatedly for 3–5 days (i.e., days 1, 2, 3, and 8), and leave on for at least 8 hours; it can be used for children and pregnant or lactating women cautiously; 7) Emollients, H1 antihistamines, topical or systemic steroids (in selected cases), topical calcineurin inhibitors, and narrow-band ultraviolet B could be used.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download