Abstract
Objectives: This study aimed to assess whether the current physician
workforce in Korea is sufficient to meet future healthcare demands, considering
demographic changes and increasing medical needs. The objective was to project
the future supply and demand for physicians and identify potential regional
disparities.
Methods: Data on outpatient and inpatient utilization rates were
obtained from the 2018 Health Insurance Statistical Yearbook, and population
projections were sourced from Statistics Korea (2017–2067). Medical
demand was estimated by multiplying these utilization rates by the population
projections. The supply of physicians was projected using a cohort-component
model that incorporated medical school quotas and age-specific attrition rates.
Two scenarios were developed to account for changes in productivity: Scenario 1
assumed a 50% decrease in productivity for physicians aged 65–75, and
Scenario 2 assumed a 75% decrease. Additionally, regional projections were
analyzed using data from provincial and secondary medical service areas.
Results: National-level projections suggest a looming shortage of
physicians, despite an increase in medical school admissions. Both scenarios
predict a physician shortage, particularly in regions such as North Gyeongsang,
South Chungcheong, and Jeju Island, by 2047. In contrast, Seoul is likely to see
a surplus of physicians. The regional analysis underscores substantial
disparities in physician distribution, with underserved areas experiencing
increasingly severe shortages.
Conclusion: The study concludes that without flexible adjustments to
medical school admission quotas and healthcare delivery systems, Korea will face
significant physician shortages in the coming decades. To address this, it is
necessary to increase the number of physicians in underserved regions and
improve the efficiency of healthcare utilization.
Estimating the demand for and supply of an appropriate number of physicians, and
planning for their adequate provision, is crucial for the proper functioning of
healthcare services.
This study was conducted to determine whether the current number of physicians is
adequate to meet the needs of a future society, considering that social changes,
such as demographic shifts, are expected to increase medical demand. Thus,
instead of evaluating whether the current physician workforce is excessive or
insufficient, this study projects the future physician workforce based on the
assumption that the number of physicians in 2018 was appropriate.
This study does not involve human subjects. Therefore, approval by the
institutional review board and the acquisition of informed consent were not
required.
This study is a simulation based on various data sources, including the Health
Insurance Statistical Yearbook, the Report of Statistics Korea, and the number
of physicians in Korea.
Since medical demand reflects the population's use of medical services, we
utilized data from the 2018 Health Insurance Statistical Yearbook to calculate
per capita outpatient and inpatient utilization by age and gender. We then used
population projection data from Statistics Korea (2017–2067) to estimate
medical demand. Assuming a workload ratio of 1:3 between outpatient and
inpatient services, we multiplied the outpatient demand by 3 to estimate the
total demand.
For the supply side, we estimated the number of physicians based on medical
school quotas using a cohort-component algorithm. We assumed a 95% pass rate for
students taking the national medical licensing examination, allowing for those
who were unsuccessful to retake the exam in subsequent years. We made
projections by age groups (20s, 30s, 40s, 50s, 60s, 65s, 70s), using the
mortality rates for each age group from 2018 Statistics Korea data to calculate
attrition rates. The retirement age was set at 75 years.
To calculate the balance between supply and demand, we first needed to quantify
medical demand in terms of the number of physicians required to meet it. We
estimated the daily workload for each physician, based on the assumption that
they work 265 days per year, using data from 2018. For physicians aged 65 to 75,
we adjusted their expected daily productivity to 50% of that of their younger
colleagues in Scenario 1, and to 75% in Scenario 2. Additionally, we factored in
an annual increase of 0.5% in the daily work capacity of a physician,
attributing this improvement to technological advancements. With these
calculations, we determined the required number of physicians each year and
compared it to the projected physician supply for that year.
Regional data were categorized into two groups: by province and by secondary
medical service area. Physician supply projections utilized age-specific
physician data from either the province or the secondary medical service area,
as specified in the 2016 data from the Ministry of Health and Welfare. Medical
demand for each province was estimated using population projections from
Statistics Korea for the years 2017 to 2047. As there were no distinct
projections available for secondary medical service areas, the 2018 population
ratios were applied to the national projections.
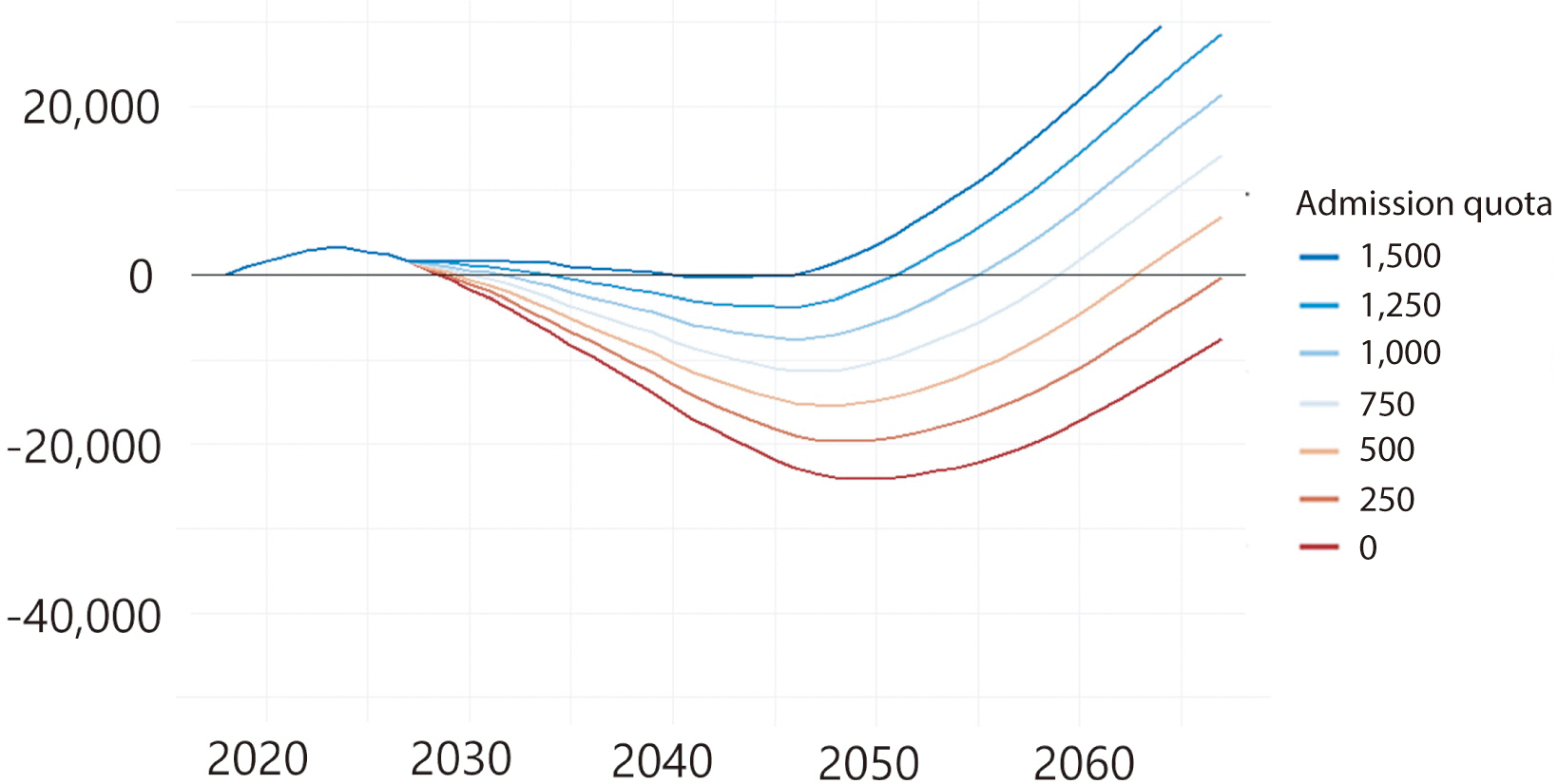
Assuming that the supply and demand of physicians were appropriately balanced
in 2018, even with an increase in the admission quota for medical schools
and graduate medical schools to 1,500 students starting in 2021, a shortage
of physicians is still predicted. However, since an excess in the physician
workforce may emerge after a certain period, it is necessary to implement
flexible adjustments by appropriately increasing or decreasing quotas (Fig. 1 and Table 1).
Even assuming that the productivity of physicians aged 65 and over decreases
not by 50% but by 75%, a shortage of physicians is still predicted, even
with an increase in the admission quota to 1,500 students starting in 2021.
However, this scenario could also lead to an excess of the physician
workforce after a certain period. Therefore, measures to appropriately
adjust the quotas are deemed necessary (Table 2).
The projection of physician workforce supply and demand by region revealed that
Seoul had the highest concentration of physicians, with a ratio exceeding
1.14–1.16 physicians per 1,000 population as of 2018. In contrast,
regions such as Chungcheong, Jeolla, Gyeongsang Provinces, and Jeju Island had
fewer than 1 physician per 1,000 population. Given the current trends, by 2047,
these regions are expected to face a more severe shortage of physicians.
In an analysis of 56 secondary medical service areas, Hongseong was identified as
having the most significant physician shortage in 2018, with approximately 1.58
fewer physicians per 1,000 people than the national average. This shortage was
closely followed by Mungyeong and Sokcho, each with a deficit of 1.45 physicians
per 1,000 population, Sacheon with 1.42, and both Jincheon and Andong with 1.40.
On the other hand, Seoul had the highest surplus of physicians in 2018, with
about 1.02 more physicians per 1,000 population than the national average.
Following Seoul were Yangsan with 0.64 additional physicians per 1,000
population, Bucheon with 0.21, Gwangju with 0.18, and Busan with 0.16.
In 2018, most secondary medical service areas in metropolitan cities had an
excess of physicians, whereas areas experiencing a shortage of physicians were
predominantly found in the Chungcheong, Jeolla, and Gangwon regions.
Assuming no increase in medical school quotas, projections for the physician
supply and demand in 2035 suggest a deepening shortage in Hongseong, which
already had the most significant shortage in 2018. By 2035, the shortage is
expected to reach approximately 2.29 physicians per 1,000 population. Following
closely are Mungyeong, with a projected shortage of 2.19 physicians per 1,000
population, Andong with 2.12, Sacheon with 2.10, and Sokcho with 2.04, all of
which are anticipated to experience worsening shortages compared to 2018.
Conversely, areas like Seoul, Yangsan, Bucheon, Suwon, and Cheonan are expected
to have an excess of physicians. The surplus is particularly notable in Seoul
and Yangsan, where the excess is predicted to exceed 1.41 and 1.12 physicians
per 1,000 population, respectively, relative to 2018.
According to the regional supply and demand projection scenarios from a study on the
adequacy of the physician workforce, the areas anticipated to experience the most
significant shortages of physicians by 2047—excluding the Gyeonggi area in
the metropolitan region—are North Gyeongsang Province, South Chungcheong
Province, North Chungcheong Province, South Jeolla Province, and Jeju Island.
Therefore, it will be necessary to increase the number of physicians providing
medical services in regions experiencing shortages. Meanwhile, according to 2018
OECD data, South Korea has fewer clinical physicians than the OECD average, yet it
records the highest number of outpatient visits per capita, at 16.9 times per year.
This indicates a significant imbalance in physician supply and demand, underscoring
an urgent need to enhance healthcare utilization behaviors and the overall
healthcare delivery system.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download