1. Ayano G, Demelash S, Gizachew Y, Tsegay L, Alati R. The global prevalence of attention deficit hyperactivity disorder
in children and adolescents: an umbrella review of
meta-analyses. J Affect Disord. 2023; 339:860–866. DOI:
10.1016/j.jad.2023.07.071. PMID:
37495084.

2. Takeda T, Tsuji Y, Akatsu R, Nomura T. Initial impact of the COVID-19 outbreak on ADHD symptoms among
university students in Japan. J Korean Acad Child Adolesc Psychiatry. 2023; 34(2):69–75. DOI:
10.5765/jkacap.220032. PMID:
37035788. PMCID:
PMC10080255.

3. Charatcharoenwitthaya K. The impact of lockdown during COVID-19 pandemic on physical and
mental health of adolescents. Siriraj Med J. 2022; 74(12):895–902. DOI:
10.33192/Smj.2022.105.

4. Thitamethee P, Likhitweerawong N, Louthrenoo O, Boonchooduang N. Chronic conditions and resilience: adolescent health behaviors in
the midst of the COVID-19 pandemic in Thailand. Glob Pediatr Health. 2024; 11:2333794X241274732. DOI:
10.1177/2333794X241274732. PMID:
39246305. PMCID:
PMC11378227.
5. Wüstner A, Otto C, Schlack R, Hölling H, Klasen F, Ravens-Sieberer U. Risk and protective factors for the development of ADHD symptoms
in children and adolescents: results of the longitudinal BELLA
study. PLoS One. 2019; 14(3):0214412. DOI:
10.1371/journal.pone.0214412. PMID:
30908550. PMCID:
PMC6433344.
6. Ra CK, Cho J, Stone MD, De La Cerda J, Goldenson NI, Moroney E, et al. Association of digital media use with subsequent symptoms of
attention-deficit/hyperactivity disorder among adolescents. JAMA. 2018; 320(3):255–263. DOI:
10.1001/jama.2018.8931. PMID:
30027248. PMCID:
PMC6553065.

7. Shi M, Liu L, Sun X, Wang L. Associations between symptoms of attention-deficit/hyperactivity
disorder and life satisfaction in medical students: the mediating effect of
resilience. BMC Med Educ. 2018; 18(1):164. DOI:
10.1186/s12909-018-1261-8. PMID:
30005708. PMCID:
PMC6043958.
8. Kim DH, Lee HJ, Lin Y, Kang YJ. Changes in academic performance in the online, integrated
system-based curriculum implemented due to the COVID-19 pandemic in a
medical school in Korea. J Educ Eval Health Prof. 2021; 18:24. DOI:
10.3352/jeehp.2021.18.24. PMID:
34551511. PMCID:
PMC8616727.

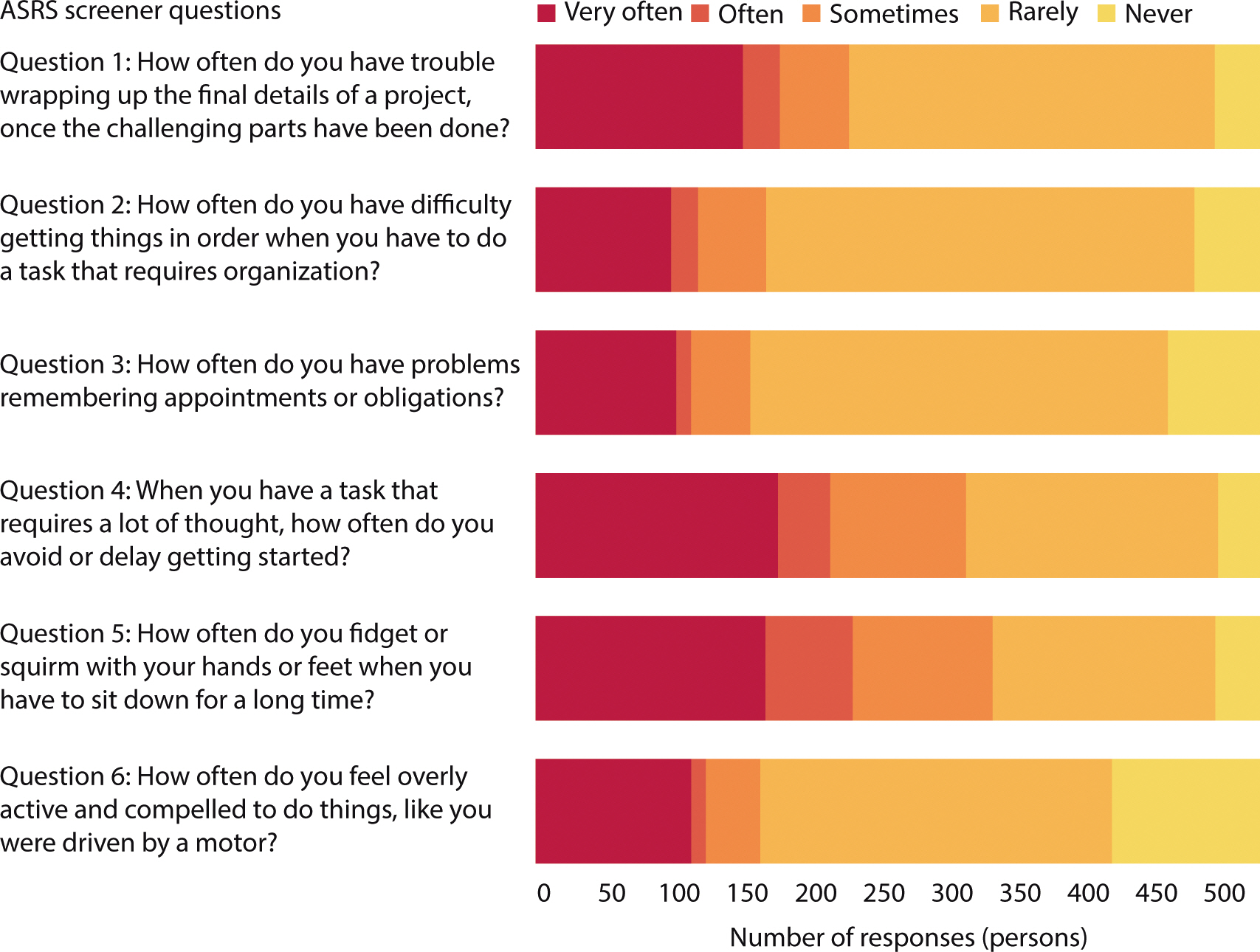
9. Bussaratid S, Atsariyasing W, Wannarit K, Pukrittayakami P, Hosiri T, Wiwatwararom N, et al. Reliability and validity study of adult ADHD Self-Report Scale
(ASRS) screener v1. 1 Thai version. J Psychiatr Assoc Thailand. 2016; 61(2):145–154.
10. Visanuyothin T, Wachiradilok P, Pavasuthiapaisit C. 597 – Prevalence of ADHD and ODD: a national survey in
Thailand 2012. Eur Psychiatry. 2013; 28:Supplement 1. 1. DOI:
10.1016/S0924-9338(13)75869-3.
11. Gimbach S, Vogel D, Fried R, Faraone SV, Banaschewski T, Buitelaar J, et al. ADHD medicine consumption in Europe after COVID-19: catch-up or
trend change? BMC Psychiatry. 2024; 24(1):112. DOI:
10.1186/s12888-024-05505-9. PMID:
38336744. PMCID:
PMC10854136.
12. Rutherford L, Stark A, Ablona A, Klassen BJ, Higgins R, Jacobsen H, et al. Health and well-being of trans and non-binary participants in a
community-based survey of gay, bisexual, and queer men, and non-binary and
two-spirit people across Canada. PLoS One. 2021; 16(2):0246525. DOI:
10.1371/journal.pone.0246525. PMID:
33571252. PMCID:
PMC7877578.
14. Randell NJS, Charlton SG, Starkey NJ. Driving with ADHD: performance effects and environment demand in
traffic. J Atten Disord. 2016; 24(11):1570–1580. DOI:
10.1177/1087054716658126. PMID:
27401237.

15. Paiboonsithiwong S, Kunanitthaworn N, Songtrijuck N, Wongpakaran N, Wongpakaran T. Learning styles, academic achievement, and mental health problems
among medical students in Thailand. J Educ Eval Health Prof. 2016; 13:38. DOI:
10.3352/jeehp.2016.13.3. PMID:
26767720. PMCID:
PMC4751292.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download