Introduction
Background
Objectives
Methods
Ethics statement
Study design
Eligibility criteria
Information sources
Search strategy
Selection and data collection process
Data items
Study risk of bias assessment
Effect measures
Synthesis methods
Results
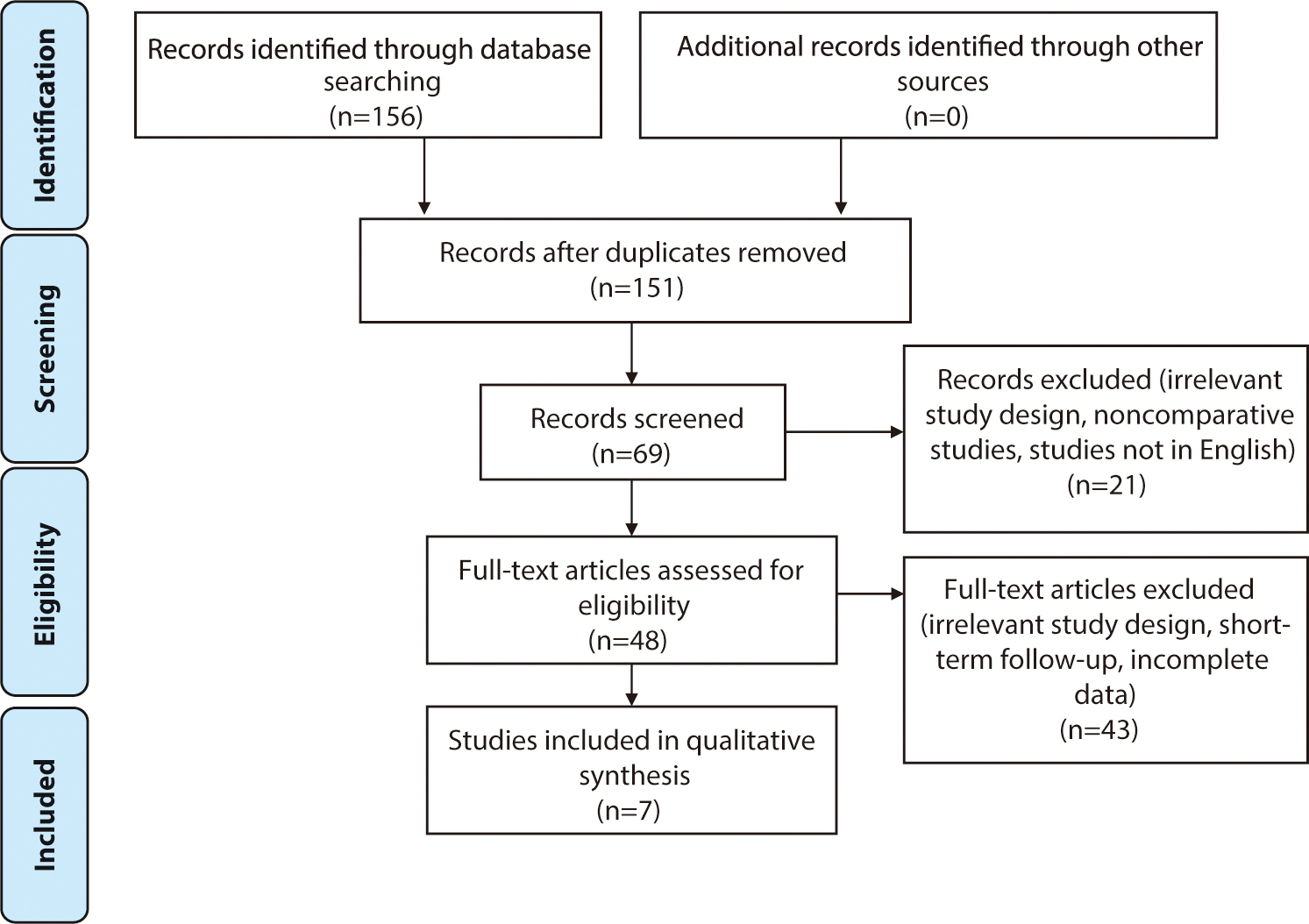
Study selection
Study characteristics
Risk of bias in studies
Results of syntheses
Baseline characteristics
Table 1.
Basic characteristics of studies
| No | Author | Intervention | Control | Sample size (n) | Gender (male/female) | Mean age (yr) | Fracture classification | Follow-up (mo) |
|---|---|---|---|---|---|---|---|---|
| Immobilization methods | ||||||||
| 1 | Park et al. [6] | PC SAC | PC LAC |
I: 36 C: 33 |
I: 2/34 C: 4/29 |
I: 66.1 C: 67.5 |
Stable fracture | 6 |
| 2 | Caruso [7] | PC SAC | PC LAC |
I: 37 C: 37 |
I: 3/33 C: 4/32 |
I: 72.3 C: 69.5 |
Extra-articular and dorsal displacement (type 2R3A2.2) | 3 |
| 3 | Okamura et al. [8] | PC SAC | PC LAC |
I: 64 C:64 |
I: 23/41 C: 17/47 |
I: 60.52±14.74 C: 62.97±13.03 |
2R3A2/2R3A3/2R3C1 /2R3C2/2R3C3 |
6 |
| Immobilization periods | ||||||||
| 1 | Christersson et al. [9] | PC 10 d | PC 10 d+3 wk |
I: 54 C: 55 |
I: 7/47 C: 4/51 |
I: 67 C: 64.7 |
2R3A3/2R3C2/2R3C3 | 12 |
| 2 | Bentohami et al. [10] | PC 3 wk | PC 5 wk |
I: 36 C: 36 |
I: 10/26 C: 13/23 |
I: >60 yr in 41.67% of
patients C: >60 yr in 50% of patients |
Stable fractures | 12 |
| 3 | Boersma et al. [11] | PC 1 wk | PC 4–5 wk |
I: 26 C: 14 |
I: 7/19 C: 4/10 |
I: 52.3±16.2 C: 56.5±9.6 |
2R3A/2R3B/2R3C | 12 |
| 4 | Olech et al. [12] | PC 4 wk | PC 6 wk |
I: 26 C: 24 |
33 women+17 men |
I: 71.34±4.99 C: 72.2±5.46 |
Stable fractures | 12–18 |
Outcomes of plaster casting
Table 2.
Comparison of clinical outcomes
| No | Author | Conclusion | DASH | PRWE | Mayo Wrist Score | VAS | Complication |
|---|---|---|---|---|---|---|---|
| Immobilization methods | |||||||
| 1 | Park et al. [6] | SACs were as effective as LACs for stable distal radius fractures in older patients. Furthermore, they were more comfortable and introduced fewer restrictions on daily activities. |
SAC: 30±15 LAC: 26.8±14.3 |
NA | NA |
SAC: 2.5±1.2 LAC: 2.1±0.84 |
NA |
| 2 | Caruso et al. [7] | Patients treated with SACs had comparable radiological and functional scores to those treated with LACs, with fewer complications secondary to immobilization of the elbow joint. |
SAC: 0.8
(0–2.1) LAC: 1.7 (0–2.5) |
NA | NA | NA | NA |
| 3 | Okamura et al. [8] | SACs demonstrated no difference in DASH outcomes, comparable reduction maintenance, and fewer adverse effects than LACs. |
6 mo: SAC: 9.88 LAC: 9.44 |
NA | NA |
6 mo (wrist): SAC: 4.89 LAC: 7.03 6 mo (shoulder): SAC: 2.69 LAC: 3.52 |
SAC: 9 LAC: 19 Most common: shoulder pain, malunion |
| Immobilization periods | |||||||
| 1 | Christersson et al. [9] | PC removal 10 d after reduction in moderately displaced DRFs is not recommended. | NA | NA | NA | Insignificant pain difference at 12 mo (P=0.92) | NA |
| 2 | Bentohami et al. [10] | Equal patient-reported outcomes between 3 wk and 5 wk of plaster cast immobilization. |
I: 0 C: 12.5 |
I: 5.0 C: 8.8 |
NA |
I: 3.1 C: 2.6 |
No complication in fracture healing, no non-union or CRPS |
| 3 | Boersma et al. [11] | 1 wk of PC treatment for nonreduced DRFs resulted in comparable functional outcomes, pain scores, complication rates, and secondary displacement. |
I: 4.6±9.5 C: 3.5±4.1 |
I: 2.9±6.6 C: 2.1±3.3 |
NA |
4 wk: I: 2.2±1.7 C:1.9±2.0 |
I: 1 C: 4 Most common: ulnar sided wrist pain, DRUJ pain, CRPS |
| 4 | Olech et al. [12] | Similar VAS and Mayo Wrist Scores between the two groups. The greatest volar tilt angle occurred after 6 wk of PC. No significant differences in other radiological parameters between the two groups. | NA | NA |
I: 58.46 ±21.24 C: 61.87 ±22.97 |
VAS pain: I: 2.53±3.06 C: 3.58±2.56 VAS activity: I: 7.61 ±1.83 C: 7.58 ±2.3 |
NA |
DASH, Disabilities of the Arm, Shoulder, and Hand; PRWE, Patient-Rated Wrist Evaluation; VAS, visual analog scale; SAC, short arm cast; LAC, long arm cast; NA, not available; PC, plaster cast; I, intervention; C, control; DRF, distal radius fracture; DRUJ, distal radioulnar joint; CRPS, complex regional pain syndrome.
Table 3.
Comparison of radiological outcomes
| No | Author | Volar tilt (°) | Radial inclination (°) | Radial length (mm) | Ulnar variance (mm) |
|---|---|---|---|---|---|
| Immobilization methods | |||||
| 1 | Park et al. [6] |
3 mo: - SAC: –0.2±6.0 - LAC: 3.9±6.2 6 mo: - SAC: –3.6±5.6 - LAC: 2.3±6.2 |
3 mo: - SAC: 13.4±6.5 - LAC: 15.4±6.1 6 mo: - SAC: 10.1±7.1 - LAC: 12.4±6.9 |
3 mo: - SAC: 5.0±3.7 - LAC: 6.2±2.6 6 mo: - SAC: 3.1±3.9 - LAC: 4.5±2.9 |
NA |
| 2 | Caruso et al. [7] |
3 mo: SAC: 0 ([–4.5]–8) LAC: 0 ([–4]–7.5) |
3 mo: SAC: 22 (19–24.5) LAC: 21 (17.5–23) |
3 mo: SAC: 9 (7–10) LAC: 8 (6–10) |
3 mo: SAC: 0 (0–1) LAC: 0 ([0.5]–2.25) |
| 3 | Okamura et al. [8] |
SAC: –1.04 LAC: –1.27 |
SAC: 18 LAC: 16.31 |
SAC: 7.89 LAC: 7.49 |
SAC: 1.41 LAC: 1.93 |
| Immobilization periods | |||||
| 1 | Christersson et al. [9] |
12 mo: the 10-d group exhibited 1.1° more redisplacement (P=0.48) than the 1-mo group |
12 mo: the 10-d group exhibited 3.2° more redisplacement (P=0.002) than the 1-mo group |
12 mo: The 10-d group demonstrated 0.7 mm more axial compression (P=0.02) than the 1-mo group |
NA |
| 2 | Bentohami et al. [10] | 1 Patient in each group showed secondary displacement | |||
| 3 | Boersma et al. [11] | NA | NA | NA | NA |
| 4 | Olech et al. [12] |
I: 9.13±7.12 C: 3.29±5.11 |
I: 1.9±1.62 C: 2.45±2.47 |
I: 0.55±2.84 C: 0.25±1.03 |
NA |




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download