Interpretation/comparison with previous studies
It is well known that various inhaled halogenated anesthetic agents can induce a preconditioning-like effect, which has been demonstrated to reduce ischemic myocardial damage in experimental models [
9] and in some clinical studies [
10,
11]. However, the temporal activity of APC varies among different anesthetics, and there are significant uncertainties in the existing literature regarding their activity and potency. In the first study to explore the potential differences among agents known to induce anesthetic preconditioning, halothane, isoflurane, desflurane, and sevoflurane were evaluated using an
in vivo rabbit coronary ligation model [
9].
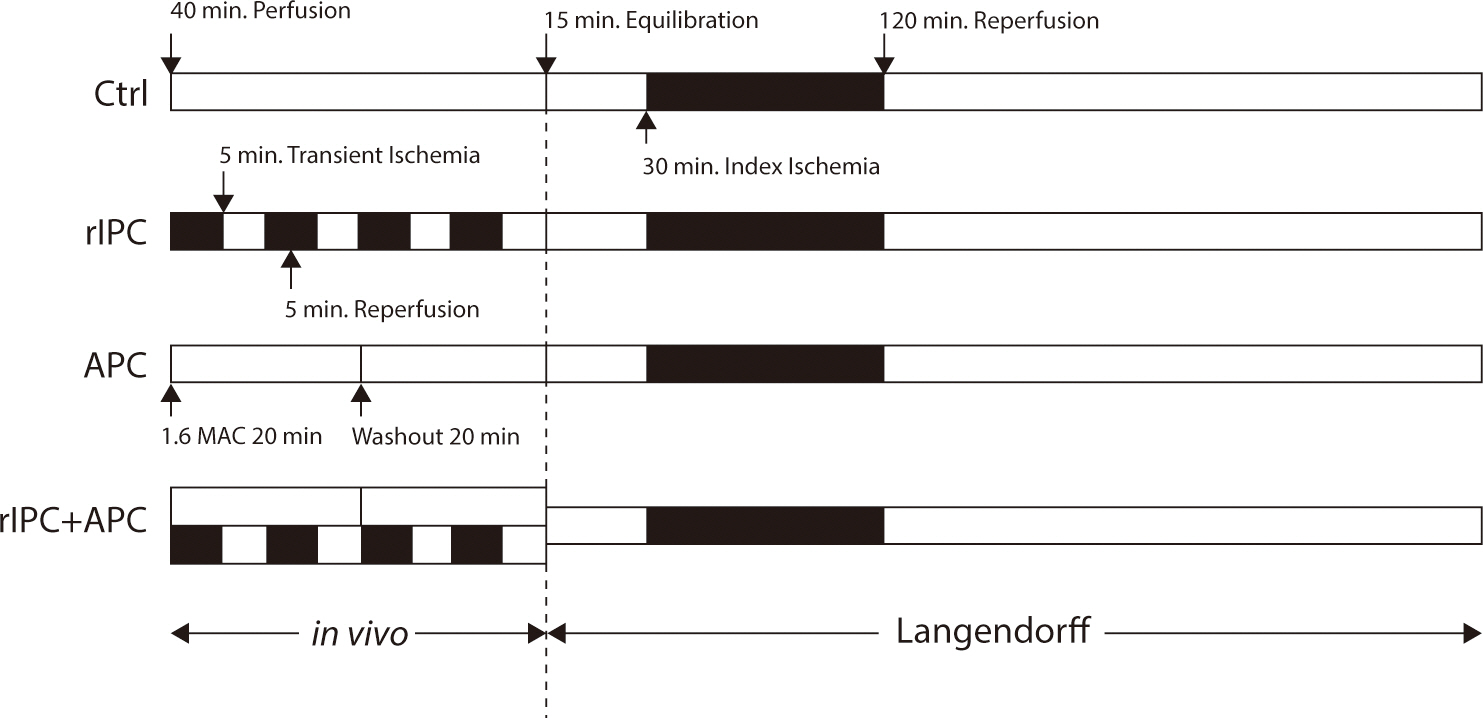
The anesthetic protocol was consistent across all groups, involving a 30-minute administration of 1 minimum alveolar concentration (MAC) of each anesthetic, followed by a 15-minute washout period, and then a 30-minute period of circumflex coronary artery occlusion. Halothane, isoflurane, and desflurane were found to be protective, significantly reducing the size of subsequent infarcts. However, sevoflurane did not confer myocardial protection when administered according to their protocol. It has been proposed that the washout period may be a critical factor in the efficacy of sevoflurane in this model. In a previous study [
12], administering 1 MAC of sevoflurane for 30 minutes immediately before ischemia reduced infarct size in dogs. However, the same dosage followed by a 30-minute washout period did not yield a reduction in infarct size. Interestingly, introducing an additional 2 minutes of local ischemia during the 30-minute washout period led to a decrease in infarct size, with the level of cardioprotection being comparable to that achieved by sevoflurane alone, without a washout period.
The anesthetic protocol used in the current study differed somewhat from those in earlier studies. We administered a slightly higher dose of sevoflurane (2.5 vol% compared to 1 MAC=2.36 vol% in the canine studies mentioned previously) and induced infarction using a Langendorff model. Despite a washout period of 20 minutes, we successfully demonstrated significant myocardial protection, achieving an approximate 50% reduction in myocardial infarction compared to the control group.
The data on the clinical effectiveness of sevoflurane as a cardioprotective agent are somewhat contradictory. In 2007, Piriou et al. [
13] investigated the effects of administering sevoflurane for 15 minutes before cardiopulmonary bypass in patients undergoing coronary artery surgery. This two-center study found no effect on postoperative troponin I levels compared to the control group. This contrasts with the findings of De Hert and colleagues, who reported cardioprotective properties of sevoflurane in patients undergoing similar surgeries [
14,
15]. In their studies, sevoflurane was administered throughout the cardiopulmonary bypass and appeared to provide a protective effect. However, the cardioprotective benefits were less certain when sevoflurane was administered only before the bypass or only after the completion of the coronary anastomosis.
rIPC is an emerging strategy to prevent myocardial damage during cardiac surgery. The effectiveness of local preconditioning of the heart and other organs has been recognized since it was first described by Murry in 1986 [
1]. Although highly effective in experimental models, the requirement to induce ischemia in the target tissue or organ before intervention has limited its clinical use. Remote preconditioning, or “preconditioning at a distance,” was initially described by Przyklenk in 1983 [
3]. In the foundational study, preconditioning the territory of the circumflex coronary artery reduced myocardial infarction following prolonged ligation of the left anterior descending coronary artery. Later studies in rodents demonstrated that similar protection could be achieved by transient ischemia of more distant organs, such as the kidney or mesentery [
7]. While remote preconditioning is as effective as local preconditioning, it has not been more clinically applicable than its local counterpart. However, transient limb ischemia as a stimulus for remote preconditioning of the heart shows greater potential. This straightforward technique, which employs a standard blood pressure cuff or tourniquet, has proven highly effective in animal models and, more recently, in clinical studies involving children and adults undergoing cardiovascular surgery [
5]. Notably, in most published animal studies and in two of the three positive clinical studies, these effects were observed to be additive to those of inhalational halogenated anesthetics [
5,
16].
In our own randomized trial focusing on remote preconditioning in children undergoing cardiac surgery with cardiopulmonary bypass, sevoflurane was administered only during the induction of anesthesia. This was followed by a fentanyl infusion and the inhalation of isoflurane throughout the procedure [
5]. Despite this regimen, remote preconditioning demonstrated additional benefits compared to the control group. Children who underwent remote preconditioning through transient limb ischemia before cardiopulmonary bypass exhibited decreased troponin release, lower inotrope scores, and enhanced lung function relative to controls. In a separate study involving adults scheduled for elective abdominal aortic aneurysm surgery, participants were randomized to undergo a single 10-minute episode of femoral artery occlusion prior to aortic cross-clamping [
16]. Although all patients received general anesthesia with inhaled desflurane for the duration of the operation, those in the preconditioned group experienced a highly significant reduction in the incidence of postoperative renal dysfunction and myocardial infarction.
Conclusion
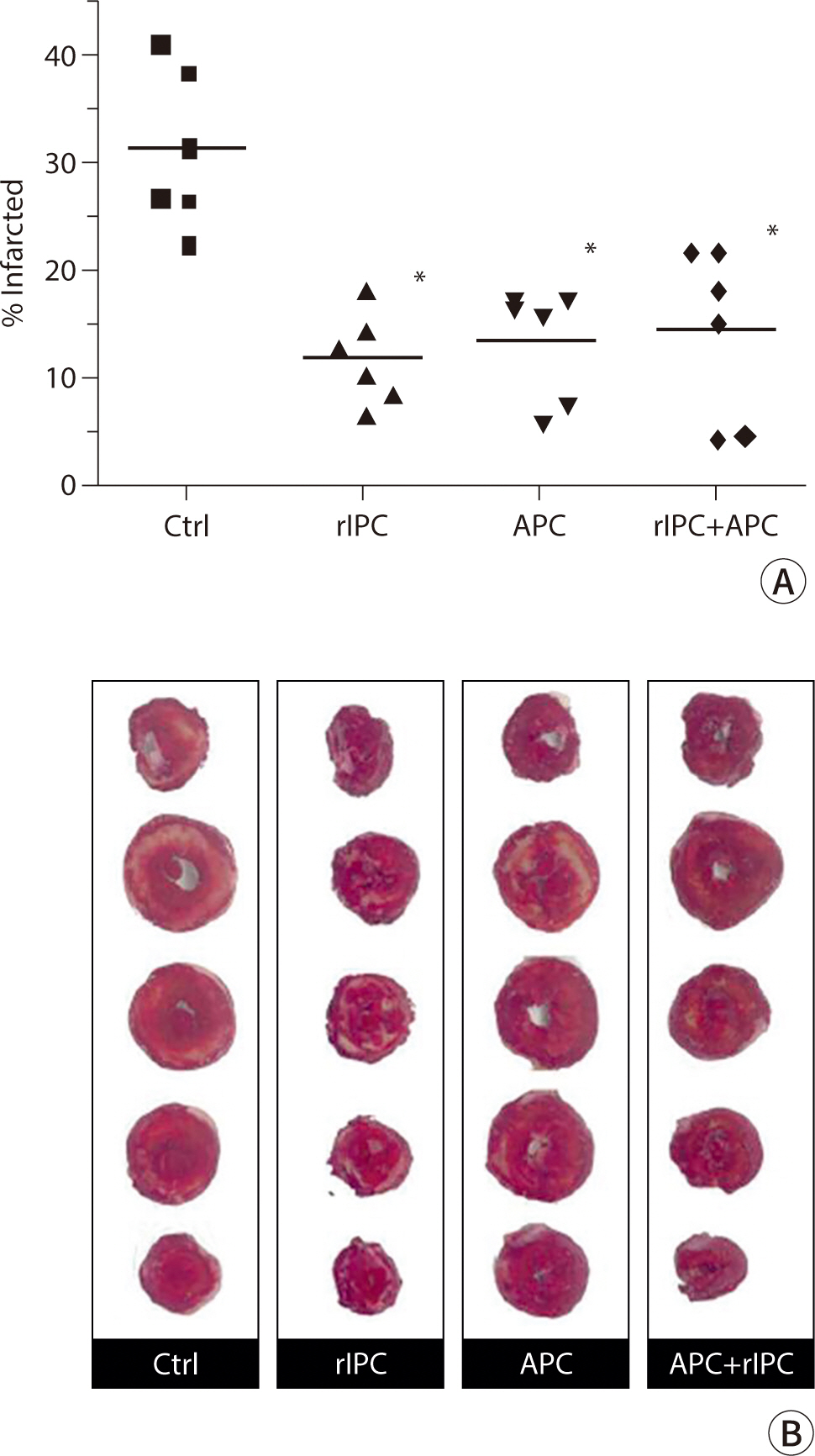
The previous clinical studies do not clarify whether the combination of inhaled anesthesia and remote preconditioning has an additive, neutral, or detrimental effect on optimal myocardial protection. Therefore, the current study is timely in assessing this potential interaction. The level of protection provided by sevoflurane was comparable to that achieved through remote preconditioning via transient limb ischemia. Notably, when both were administered together, the degree of protection remained unchanged.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download