Abstract
Recent advancements in malaria diagnostics have revolutionized the detection and management of this deadly disease. From traditional microscopy to rapid diagnostic tests and currently, to cutting-edge molecular techniques, such as isothermal amplification and different types of polymerase chain reactions, significant progress has been witnessed in enhancing the sensitivity, specificity, and accessibility of diagnostic tools. These innovations have enabled rapid and more accurate detection of malarial parasites, especially in regions with limited healthcare infrastructure. Furthermore, integrating information technology- and artificial intelligence-based applications with point of care devices has facilitated realtime data collection and decision-making, ultimately aiding global efforts toward malaria elimination. Although conventional techniques are still employed at field sites, challenges such as high sensitivity, species specificity, cost-effectiveness, scalability, and the emergence of drug-resistant strains persist. These challenges underscore the need for continuous research and development of novel malaria diagnostics.
Malaria remains a major global health challenge. Five Plasmodium species can infect humans: P. falciparum, P. vivax, P. malariae, P. ovale, and P. knowlesi. Among these, P. falciparum and P. vivax are the most prevalent globally, and severe malarial complications are most commonly associated with P. falciparum infections [1]. Recently, the zoonotic parasite P. knowlesi, which was misdiagnosed as P. malariae, has been classified as zoonotic malaria in southeastern countries in Asia [2].
In tropical regions, fever is a common symptom of several diseases including malaria. The accurate and early diagnosis of malaria is essential to prevent severe clinical cases and ensure timely treatment [3]. Prompt detection of malaria upon hospital admission is crucial for initiating treatment, reducing community transmission, preventing complications, improving patient outcomes, and maintaining the efficacy of antimalarial drugs. Minimizing misdiagnosis in primary care is vital for effective treatment and for avoiding unnecessary antimalarial drug use, which can lead to side effects and drug resistance. Therefore, improving diagnostic accuracy and reducing false positives are key to effective malaria control and patient care [4].
To address these challenges, reliable malaria diagnostic tests are essential. Accurate diagnosis enables monitoring of drug resistance patterns in malarial parasites. Healthcare providers can adjust treatment protocols and prevent the spread of drug-resistant parasites by identifying cases of treatment failure and tracking the emergence of antimalarial drug resistance [5]. Thus, a reliable and rapid diagnosis of malaria may be considered for the prevention of severe malaria at field sites in endemic countries [6].
Currently, the most frequently used method for diagnosing malaria, particularly in primary care settings and areas with limited laboratory access, is microscopic examination, which is the gold standard for the development of novel techniques such as rapid diagnostic tests (RDTs) and molecular methods. Several techniques are currently available for rapid malaria diagnosis, including RDTs, cytometric diagnosis, and molecular detection methods such as polymerase chain reaction (PCR), real-time PCR, nested PCR, qPCR, multiplex PCR, recombinase polymerase amplification (RPA), and loop-mediated isothermal amplification (LAMP). In addition, information technology (IT)- and artificial intelligence (AI)-based point-of-care (POC) devices have been integrated into diagnostic processes. Herein, we discuss the challenges and prospects associated with each diagnostic method.
Microscopy remains a crucial tool for diagnosing malaria because of its ability to accurately identify malarial parasites and provide valuable information for patient management and public health surveillance. The technique involves staining a thin blood smear and examining it under a microscope to detect the presence of malarial parasites. Over time, refinements in staining and microscopic methods have improved the accuracy and reliability of diagnoses. The World Health Organization (WHO) has developed standardized protocols for preparing and examining blood smears and criteria for classifying malarial species and quantifying parasite density [7,8].
Microscopy is considered the gold standard for laboratory confirmation of malaria because it allows direct visualization of malarial parasites in patient blood samples. Trained microscopists can accurately identify the presence of parasites, distinguish between different species and developmental stages in infected erythrocytes, and quantify parasite density, thereby providing valuable information for patient management [6,9].
Five species of human malarial parasites (P. falciparum, P. vivax, P. malariae, P. ovale, and P. knowlesi) have distinct morphological features when observed under a microscope. This distinction is important because different species may require different treatment regimens and accurate species identification helps ensure appropriate therapy.
Microscopic diagnosis requires trained and experienced laboratory technicians and microscopists. Accurately identifying malarial parasites under a microscope demands expertise and proficiency, and prolong turnaround times to obtain diagnostic results [10]. This process is labor-intensive and time-consuming and requires skilled personnel to prepare and examine slides manually. Maintaining an adequate laboratory infrastructure, equipment, and supplies for microscopy can be challenging in remote or resource-limited settings. Limited access to electricity, clean water, and trained personnel may affect the reliability and availability of microscopy services. It may be difficult to diagnose mixed infections where more than one malarial parasite species coexists in the same individual in highly endemic areas. Distinguishing between different parasite species and accurately quantifying the parasite density in mixed infections can be challenging and may lead to misdiagnosis.
Despite these disadvantages, microscopic examination remains an important diagnostic tool for malaria, particularly in areas where molecular or RDTs are unavailable. Efforts to address the limitations of microscopy include personnel training programs, quality assurance measures, and the development of complementary diagnostic technologies.
Immunodiagnostic techniques, including immunochromatography-based RDTs, enzyme-linked immunosorbent assays, and flow cytometry, are extensively employed to detect Plasmodium infections. Among these, RDTs stand out as the preferred method for detecting specific antigens such as parasite lactate dehydrogenase (pLDH), P. falciparum histidine-rich protein 2 (PfHRP2), and Plasmodium aldolase (pAldolase), as well as antibodies associated with malaria parasites. Over the past decade, RDTs have emerged as an alternative diagnostic tool for malaria when high-quality microscopy is unavailable or unreliable [11].
The RDT utilizes a lateral flow immunochromatographic method involving the interaction of dye-labeled antibodies with parasite-specific antigens in blood samples on a nitrocellulose strip, resulting in a visible line. The intensity of the line color indicates the quantity of parasite antigens present in the blood samples [12]. It can identify a range of species from P. falciparum to non-falciparum parasites, P. vivax, P. malariae, P. ovale, and P. knowlesi.
According to the WHO quality assurance guidelines [13], RDTs must reliably detect the following: (a) less than 200 parasites/μL, equivalent to 0.004% parasitemia for P. falciparum and P. vivax, (b) a false-positive rate of less than 10%, and (c) an invalid rate of less than 5%.
The commonly used antigens for commercially available RDTs include PfHRP2 and two enzymes from the Plasmodium parasite glycolytic pathways, namely, pLDH, and pAldolase. Specifically, PfHRP2, PfpLDH, and aldolase were used to detect P. falciparum, whereas Pv-pLDH and non-P. falciparum LDH (panpLDH) for detecting non-falciparum parasites, including P. vivax, P. ovale, P. malariae, and P. knowlesi [14,15].
Commercial assays that detect PfHRP2 and/or PfLDH include Bioline™ (Abbott Point of Care), CareStart™ (Access Bio), Binax NOW (Binax Inc.), First Response (Premier Medical Corporation Ltd), pfLDH (Mologic), NxTek™ Eliminate Malaria Pf test (Abbott Diagnostics Korea Inc.), One Step test for Malaria (Meril Diagnostics Pvt. Ltd), OptiMAL (DiaMed AG), Paracheck Pf (Orchid Biomedical Systems), ParaHIT® (Arkray Healthcare Pvt. Ltd), Parascreen (Tulip Diagnostics (P) Ltd), RapiGEN (RapiGEN Inc.), and STANDARD™ (SD Biosensor) [16].
PfHRP2 is produced during both the asexual and sexual stages in P. falciparum. This particular antigen becomes detectable within 24 to 48 hours following the invasion of new erythrocytes and remains in the plasma or serum for up to 3 weeks. This extended presence allows the detection of PfHRP2 even when parasites are not visible through microscopy because of sequestration. However, the persistence of PfHRP2 in the bloodstream after parasite clearance can result in false positives. In addition, in regions where parasites exhibit deletions in the pfhrp2 gene, PfHRP2-based RDTs may have reduced sensitivity, leading to inaccurate negative results.
In a previous report, the performance of the PfHRP2/pLDH Combo kit (CareStart) was compared with that of a microscopic examination in a malaria-endemic region in Uganda. The study confirmed that PfHRP2 RDTs had a high sensitivity of 88.8% (84.8%–92.0%) for variable parasite densities in blood samples and a high specificity of 98.9% (96.8%–99.0%) for detecting P. falciparum infections. However, false negative results were observed with PfHRP2-based RDTs in patients with low parasitemia and parasites lacking the pfhrp2 gene [17,18].
Another product from the same company, the CareStart™ Malaria pLDH (Pf/pan) Combo Test, has been evaluated in a field study in Madagascar [19]. This study reported sensitivities for P. falciparum that were comparable to those in the current study, including lower values at parasite densities < 100 parasites/μL (60.0%) and increased sensitivity at higher parasite densities at > 500 parasites/μL (100%).
Estimates from meta-analyses indicate that PfHRP2-detecting RDTs have an average sensitivity of 95.0% (95% confidence interval [CI]: 93.5%–96.2%) and an average specificity of 95.2% (95% CI: 93.4%–99.4%) [20]. In comparison, Pf-pLDH-detecting RDTs exhibited slightly lower sensitivities of 93.2% (95% CI: 88.0%–96.2%) but demonstrated higher specificities of 98.5% (95% CI: 96.7%–99.4%) [20]. The Pv-pLDH RDTs displayed a comparable pooled sensitivity of 95% (95% CI: 86%–99%) and specificity of 99% (95% CI: 99%–100%) relative to reference microscopy in endemic regions. However, in studies where Pv-pLDHdetecting RDTs were evaluated against PCR as the reference standard, sensitivities ranged from 59% to 77%, and specificities ranged from 97% to 100% [21].
The accuracy of RDTs for malaria can vary based on factors such as the RDT manufacturer, type of antigen targeted, density of parasites, genetic variation of pfhrp2/3 among P. falciparum parasites, overall prevalence of malaria, range of parasite species, optimal test performance, and immune response of patients in malaria-endemic regions. Despite the challenges associated with RDTs, they offer significant benefits compared to traditional microscopic analyses, especially in less accessible rural or remote areas. RDTs are cost-effective, do not require complex equipment, provide rapid results, and are easy to use. These features make RDTs highly suitable and accessible in areas with limited resources.
For both microscopic and cytometric diagnoses, the accurate identification and analysis of small numbers of malaria-infected blood cells in a large number of healthy cells is crucial. The first step involves distinguishing the physical and chemical attributes that differentiate parasite-infected red blood cells from other blood components and different malaria species [22].
Effective identification requires a detailed examination of well-prepared, stained smears under high magnification (1000×) using an oil immersion lens. Common staining methods include dihydroethidium, Hoechst 33342, or SYBR Green I for parasites and CD45 monoclonal antibody for leukocytes. This allows for distinguishing infected from non-infected red blood cells and assessing the parasite stages, which are essential for diagnosis and drug efficacy testing [23,24].
Cytometric assays that match microscopic examinations in terms of sensitivity and specificity are vital for malaria research and diagnostics. However, advanced cytometers using ultraviolet (UV) lasers for Hoechst detection are typically too large for field use and are better suited for high-throughput clinical and research settings, especially for antimalarial drug discovery [25].
Key diagnostic features include the examination of the nuclei for size, shape, texture, and cytoplasmic characteristics, including the presence of hemozoin. Hemozoin, a byproduct of hemoglobin digestion by the parasite, is detectable based on its magnetic, optical, and acoustic properties [26,27]. The Gazelle device (Hemex Health), which identifies malaria by analyzing hemozoin crystals in lysed blood samples, shows high sensitivity (97.6%) and specificity (96.8%) compared to microscopy, PCR, and RDT in P. falciparum endemic areas [28].
Despite its effectiveness, this method has drawbacks, including labor intensity, the need for skilled technicians, expensive equipment, and potential false positives with other infections. However, it remains a valuable screening tool and hemozoin-containing leukocyte counts may correlate with disease severity, although the findings vary [28]. Automated hematological analysis is a rapid, sensitive, and cost-effective method for evaluating suspected malaria cases in hospitals. Unusual scattergrams may result from white blood cells scattering light differently after phagocytosing parasites and incorporating hemozoins [26,29,30]. Although advanced flow cytometry can detect intraerythrocytic hemozoin, it is less suitable for P. falciparum diagnosis because of trace amounts of hemozoin in the circulating ring-stage parasites.
In laboratory settings, single-color flow cytometers that utilize nucleic acid staining have traditionally been used to identify malaria-infected red blood cells. Recently, Sysmex (Kobe, Japan) developed an automated hematology analyzer to diagnose parasite-infected red blood cells using nucleic acid staining. This analyzer can differentiate between the malarial species P. falciparum and P. vivax by employing fluorescent dyes to enhance the fluorescence intensity [31]. Previous studies evaluating the performance of the Sysmex XN hematology analyzer for malaria detection have reported sensitivities ranging from 1.1% to 64.0% [32-35].
Nucleic acid amplification technology (NAAT) is a collection of techniques used to amplify small amounts of nucleic acids (DNA or RNA) at detectable levels. NAATs play a crucial role in different applications, including early and sensitive diagnosis of infectious diseases [36]. These technologies are essential for molecular biology, medical diagnostics, and research such as PCR [37], isothermal amplification techniques (LAMP) [38], RPA [39], nucleic acid sequence-based amplification [40], helicase-dependent amplification [41], strand displacement amplification [42], transcription-mediated amplification [43], rolling circle amplification [44], and multiple displacement amplification [45]. These technologies are highly sensitive owing to their capacity to amplify minute quantities of target DNA or RNA. NAAT-based molecular diagnostics show a unique sensitivity for infectious diseases, including malaria. The broad category of NAATs includes different forms of PCRs (multiplex, nested, real-time, and qPCR), LAMP, and molecular POC testings (POCTs).
One of the most noteworthy scientific breakthroughs in molecular genetics over the past decade has been the development of PCR. PCR is the most commonly employed genetic amplification method in laboratories owing to its robust thermal cycling process, specificity, simplicity, speed, and sensitivity. PCR has enabled the development of highly sensitive techniques for detecting malarial parasites, and its inherent specificity allows for precise identification of the parasite genome down to the species level [46].
Multiplex PCR is a variation of standard PCR that allows simultaneous amplification of multiple target DNA sequences in a single PCR experiment. This method uses multiple pairs of primers in a single PCR mixture to amplify different DNA segments specific to the organism or gene of interest. The principle of multiplex PCR is to increase the efficiency and productivity of PCR-based diagnostic tests by reducing the number of reactions required. In the context of malaria diagnostics, multiplex PCR is particularly valuable because it can differentiate between different Plasmodium species that cause malaria in a single test [47,48]. This is crucial for accurate diagnosis and appropriate treatment because different species may require different treatment regimens.
Primers are often designed based on 18S ribosomal RNA (rRNA) genes, which have higher multi-copy numbers (4–8 copies per parasite) than other single-copy targets in the genome. These genes have been used for Plasmodium species-specific diagnosis because of their high sensitivity [49,50]. Plasmodium spp. possess two distinct 18S rRNA subunits, each expressed at different stages of the parasite’s life cycle: one during the blood and liver stages and another during the sporozoite stage. These 18S rRNA genes differ in both sequence and size.
In addition to the 18S rRNA gene, several other high-copy genes have recently been reported as equivalent or better diagnostic targets, including telomere-associated repetitive element 2 (TARE-2; 250 copies/genome) and the acidic terminal sequence of the var gene (varATS; 59 copies/genome) [51]. These two target gene assays displayed higher sensitivity than 18S rRNA gene detection.
The introduction of nested PCR has significantly enhanced the performance and sensitivity of PCR for malaria diagnosis. Nested PCR is a two-step amplification process. In the first stage of PCR (Nest-1), primers specific to the Plasmodium genus are designed from the target sequence and used to amplify the target DNA from the samples. The amplified product from this initial reaction served as a template for the secondary PCR (Nest-2). Secondary PCR employed species-specific primers targeting all human Plasmodium species, as described by Snounou et al. (1993) [49] and Singh et al. (1999) [50]. The second stage (Nest-2) used Plasmodium species-specific primers to further amplify the target DNA. This technique is sensitive enough to detect malarial infections with parasitemia levels as low as 5–6 parasites/μL, making PCR-based techniques highly effective for diagnosing malaria [52-54].
The refined nested PCR technique assesses Plasmodium DNA within the highly conserved regions for genus identification and amplifies a variable region to enhance sensitivity and specificity for species-specific identification of the 18S rRNA gene [49,50,55-57]. Nested multiplex PCR can distinguish between the DNA of P. falciparum, P. vivax, P. malariae, P. ovale, and sometimes the less common P. knowlesi [58]. This allows specific identification and appropriate treatment decisions.
However, there is potential for cross-reactivity in Plasmodium species-specific reactions because of similarities in the primer-binding regions of 18S rRNA gene sequences used for PCR. Despite this, molecular approaches offer a highly precise diagnosis, enhancing the proper treatment and management of malaria.
Although traditional diagnostic PCR is sensitive and cost-effective, it requires considerable time from gene amplification to visualization, as well as expensive reagents and equipment. In comparison, several of today’s real-time PCR assays are probe-based, costly, and may not be effective for detecting all species in a single amplification reaction. Furthermore, melting curves were explored for additional species confirmation and validation in multiplex systems [59]. Previous studies have demonstrated that real-time PCR is both time- and cost-efficient, employing a single protocol to identify and distinguish five human Plasmodium species with detection limits for P. falciparum, P. vivax, and P. malariae of 0.064, 1.6, and 0.32 parasites/µL respectively, without cross-reactivity [60-62]. Advancements in real-time PCR technologies, including realtime qPCR, digital PCR (dPCR) [63], and digital droplet PCR (ddPCR) [64], now allow the detection of extremely low parasite densities (less than 0.2 parasites/µL). Although qPCR remains sensitive and effective, several advanced qPCR methods require probe-based techniques that are not only expensive but also often unsuitable for single-reaction conditions owing to specific needs for annealing, elongation temperatures, and cycle numbers. These sophisticated methods are predominantly utilized in well-equipped facilities within endemic regions, offering a potent alternative for malaria diagnosis using a molecular diagnostics toolkit.
LAMP is a simple and efficient molecular diagnostic technique involving DNA amplification under isothermal conditions [65-67]. This method eliminates the need for sophisticated laboratory equipment when malaria-endemic field sites are expensive. LAMP can amplify DNA between 1 billion and 10 billion times within 15–60 min. This supports different methods of detection: visual inspection through the integration of f luorescent dyes, including SYBR Green I dye, or more automated detection approaches using cost-effective turbidimeters for real-time monitoring. Furthermore, the application of LAMP in malaria diagnostics has been enhanced by its integration into portable microfluidic chips [68]. This innovation is complemented by a streamlined DNA extraction process using simple boiling and spin techniques.
Unlike PCR, which relies on cycling at three different temperatures, the LAMP assay provides the advantage of amplifying nucleic acids (RNA and DNA) at a constant temperature, generally around 62℃–65℃, without the need for annealing or denaturation. This isothermal method significantly reduces the overall processing time and eliminates the requirements of a thermocycler. LAMP uses a strand-displacing Bst DNA polymerase to initiate synthesis, with two of its four to six primers forming loop structures that streamline subsequent amplification rounds. Moreover, the LAMP technique is highly tolerant to inhibitory substances found in blood samples, such as hemoglobin and metal ions, and can work efficiently with small quantities of blood applied to filter paper. However, the LAMP assay has several limitations: it currently suffers from inadequate accuracy, limited application in field settings due to the necessity of cold storage for reagents, burdensome blood sample preparation processes, and restricted multiplexing capabilities. In previous studies, blood samples were modified for DNA amplification using the boiling method without a complex extraction procedure [66].
LAMP has a high sensitivity and specificity for malaria diagnosis. Meta-analyses have reported that LAMP can achieve sensitivity rates ranging from 96% to 98% and specificity rates of approximately 95% compared with microscopy and PCR, making it an excellent tool for malaria diagnosis in both endemic and non-endemic settings [65,69,70] . The detection limit of LAMP for malaria diagnosis is notably low, and it can detect as few as 5 to 10 parasites per microliter of blood. This makes it highly effective for identifying low-density infections that may be missed by microscopy or RDTs [69,71] .
The LAMP assays for malaria are designed to be user-friendly and suitable for field conditions. They can provide results within an hour, with visual detection of DNA amplification typically achieved through fluorescence or turbidity changes that can be observed with the naked eye under UV light [66,71] . This quick turnaround time is beneficial for prompt diagnosis and treatment, particularly in remote areas that lack advanced laboratory infrastructure. Overall, LAMP is a valuable tool for malaria diagnosis owing to its high accuracy, low detection limits, and practicality in resource-limited settings.
Recently, RPA has emerged as a simpler alternative to PCR-based assays for the diagnosis of malaria. RPA targets a specific fragment of the 18S rRNA gene and uses strand-displacing DNA polymerase to form a recombinase-primer complex, eliminating the need for thermal cycling. This isothermal process operates at moderate temperatures (37℃–42℃) and can be completed in approximately 20 min using basic equipment such as a heating block.
The minimal equipment requirements of the RPA make it highly suitable for resource-limited laboratories because it can be conducted using a simple incubator. This simplicity and adaptability of position molecular POC-RPA make it a promising diagnostic tool for detecting malarial parasites, allowing for straightforward execution and result interpretation without specialized instruments. For the endpoint detection of RPA products, the combination of RPA with lateral flow assays (LFA) has become the preferred visual readout method. RPA-LFA assays have been successfully used to detect P. falciparum and P. knowlesi parasites [72-75].
Studies have demonstrated that RPA assays demonstrate high sensitivity (88%–100%) and specificity (100%) for P. falciparum and P. knowlesi, detecting as little as 100 fg of genomic DNA, which corresponds to a limit of detection of four parasites per reaction within 10 min. For example, the assay detected five copies/µL of synthetic Plasmodium DNA in under 30 min using synthetic copies of the 18S rRNA gene from Plasmodium species that infect humans. The sensitivity of this assay is comparable to other isothermal amplification methods and optical microscopy [76].
Designing effective RPA primers and probes remains a significant challenge, particularly for the development of multiplex RPA assays. This complexity arises from the need to test numerous primer and probe combinations to determine a functional set. Effective primer design must avoid the formation of primer dimers with lengths of 30–35 bases; otherwise, primers of up to 45 nucleotides may form secondary structures and artifacts. Overall, RPA is a novel, rapid, and sensitive molecular technique for malaria detection that offers a practical solution for POC testing in resource-limited settings.
POC molecular diagnostic devices for malaria are advancing rapidly, offering more efficient and fielddeployable options to improve diagnostic accuracy and accessibility, particularly in resource-limited settings. POC-NATs can rapidly detect the presence of malarial parasites with high sensitivity and specificity and typically involve three phases: sample preparation, nucleic acid amplification, and signal transduction. Despite significant advancements in the latter two phases, the initial step of sample preparation continues to be complex and labor-intensive, posing a challenge for the development of fully integrated POC molecular diagnostic tools. Efforts have been made to streamline and consolidate sample preparation processes in these devices through innovative integration techniques, the use of newly engineered materials, improved reagent storage, and fluid management systems [77,78]. A deeper understanding of the technologies involved in integrated POC molecular diagnostics, from sample preparation to signal transduction, is essential for driving forward innovations that can lead to personalized medicine and enhance global public health outcomes.
Recently, numerous researchers have explored nucleic acid testing for the detection of Plasmodium parasites and as a POC molecular diagnostic tool for malaria. Technical barriers to molecular POCT include the availability of thermocyclers, the need to optimize each reaction using appropriate materials, and the handling of nucleic acid amplification reagents. The most promising molecular POCT techniques include isothermal amplification methods, such as LAMP and RPA. Although PCR, multiplex PCR, and real-time PCR are commonly used, commercial molecular POCT products are currently limited to LAMP-based kits. Notable examples include the Loopamp Malaria Detection Kit (Eiken), which offers pan-genus-, P. vivaxspecific, and P. falciparum-specific kits. The RPA holds potential for the development of colorimetric RDTs because it can be formatted into a lateral flow cassette for easy visualization.
Microfluidic technologies have significantly enhanced the portability and functionality of POC diagnostic tools, enabling the development of robust, sensitive, and specific malaria diagnostic assays [79-81]. These devices automate nucleic acid extraction and amplification with minimal manual intervention, making them accessible to non-technical personnel. The complexity and cost of molecular diagnostics can be reduced by integrating sample processing and analytical functions into a single platform. Digital microfluidics and biosensors represent another breakthrough offering highly sensitive assays for the detection of infectious pathogens through advanced optical sensing. These platforms can be incorporated into portable devices to support sophisticated biochemical analyses [82-84].
Advancements in telemedicine and mobile technologies have further enhanced malaria diagnosis. Systems such as the Malaria Case Notification System in Zanzibar and the Mobile-based Surveillance Quest using IT in India use mobile and web-based technologies to streamline malaria surveillance and diagnostics [8587]. These initiatives highlight the potential of digital health solutions in combating malaria. Integrated POC molecular diagnostic devices are making significant progress in providing rapid, accurate, and accessible malaria diagnostics, which are essential for effective disease management and elimination.
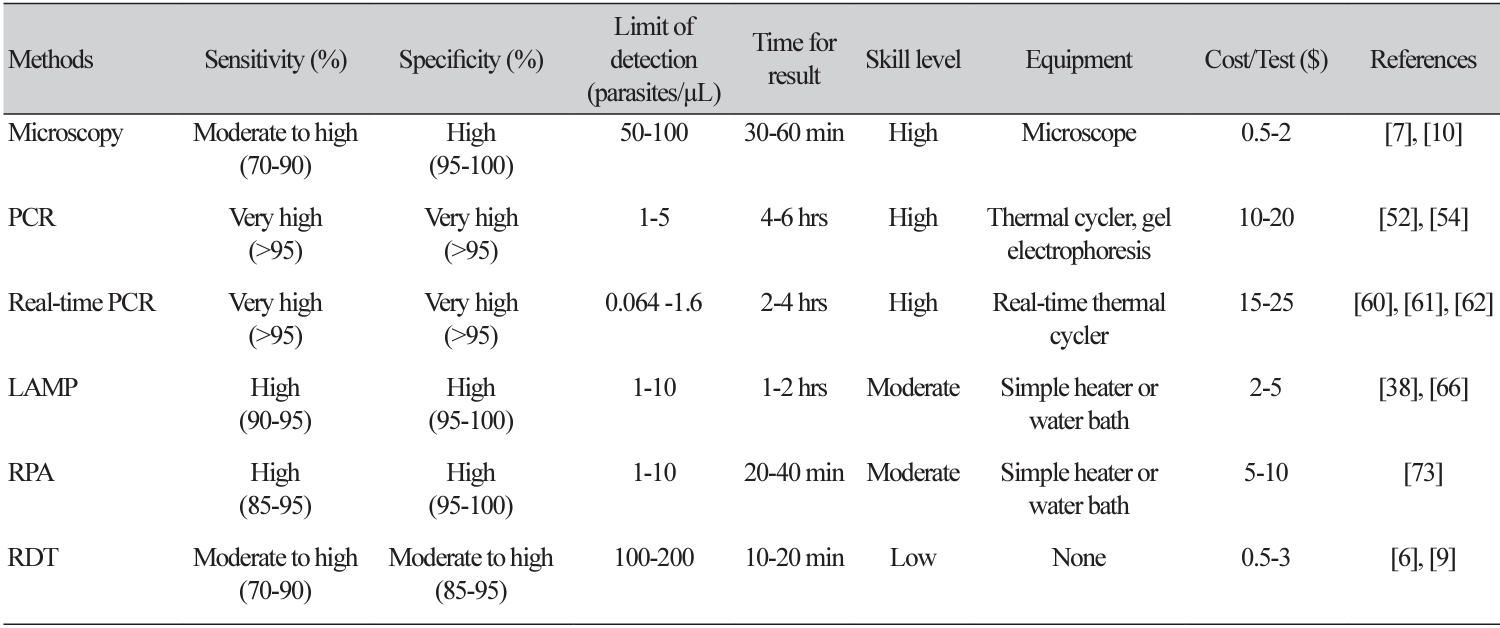
This review provides a comprehensive comparison of six diagnostic techniques, namely microscopy, PCR, real-time PCR, LAMP, RPA, and RDTs (Table 1).
Microscopy is the preferred method for malaria diagnosis because of its high reliability and costeffectiveness. RDTs offer valuable advantages, such as swift results, simplicity, and low cost, making them particularly useful in remote areas. Recently, certain RDT quality improvements have been achieved for the diagnosis of clinical cases and are used widely in low-income endemic countries by the WHO and non-government organizations. Cytometric techniques present an option for parasite identification and the quantification of parasite density, especially in cases of low parasitemia. However, their utilization requires well-trained technicians and expensive equipment in hospitalized institutions and is useful for the highthroughput screening of antimalarial drugs. PCR-based tests, including real-time PCR, multiplex PCR, and nested PCR, are preferred because of their ability to provide comprehensive information on the parasite load, species, and drug resistance. Nevertheless, their reliance on skilled professionals and consistent electricity supply poses challenges, rendering them less feasible in low-resource settings or POCT. Isothermal DNA amplification methods such as LAMP and RPA exhibit potential for field-based malaria diagnosis. LAMP and RPA assays are rapid, straightforward, and require affordable equipment. When combined with IT- and AI-based technologies, they offer compelling prospects for POC diagnostics owing to their simplicity, affordability, and impressive sensitivity and specificity, particularly when suited for malaria diagnosis in remote areas.
Ethics statement
This was not a human population study; therefore, approval by the institutional review board and informed consent were not required.
Funding
This study was supported by a National Research Foundation of Korea (NRF) grant (NRF2021R1A2C2008235) funded by the Korean government (MSIP) and a grant from the Basic Science Research Program (NRF-R1A4A1031574 to E.T.H.) funded by the Ministry of Science, ICT, and Future Planning.
REFERENCES
1. Dalrymple U, Mappin B, Gething PW. Malaria mapping: understanding the global endemicity of falciparum and vivax malaria. BMC Med 2015;13:140.
2. Millar SB and Cox-Singh J. Human infections with Plasmodium knowlesi—zoonotic malaria. Clin Microbiol Infect 2015;21:640-8.
3. Akafity G, Kumi N, Ashong J. Diagnosis and management of malaria in the intensive care unit. J Intensive Med 2024;4:3-15.
4. Ayong L, Moukoko CEE, Mbacham WF. Diagnosing malaria: methods, tools, and field applicability. Methods Mol Biol 2019;2013:73-82.
5. Ippolito MM, Moser KA, Kabuya JB, Cunningham C, Juliano JJ. Antimalarial drug resistance and implications for the WHO global technical strategy. Curr Epidemiol Rep 2021;8:46-62.
6. Moody A. Rapid diagnostic tests for malaria parasites. Clin Microbiol Rev 2002;15:66-78.
7. Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg 2007;77:119-27.
8. WHO. Malaria microscopy quality assurance manual – version 2. 2nd ed. Geneva: World Health Organization;2016:158.
9. Murray CK, Gasser RA, Jr., Magill AJ, Miller RS. Update on rapid diagnostic testing for malaria. Clin Microbiol Rev 2008;21:97-110.
10. WHO. Basic malaria microscopy. part I: learner’s guide. 2nd ed. Geneva: World Health Organization;2010:90.
11. WHO. The role of RDTs in malaria control. https://www.who.int/teams/global-malariaprogramme/case-management/diagnosis/rapid-diagnostic-tests/role-in-malaria-control [Online] (last visited on 26 August 2024).
12. WHO. How malaria RDTs work. https://www.who.int/teams/global-malaria-programme/casemanagement/diagnosis/rapid-diagnostic-tests/how-malaria-rdts-work [Online] (last visited on 26 August 2024).
13. WHO. World malaria report 2018. Geneva: World Health Organization;2018:210.
14. Mukkala AN, Kwan J, Lau R, Harris D, Kain D, Boggild AK. An update on malaria rapid diagnostic tests. Curr Infect Dis Rep 2018;20:49.
15. Tan AF, Sakam SSB, Rajahram GS, William T, Abd Rachman Isnadi MF, Daim S, et al. Diagnostic accuracy and limit of detection of ten malaria parasite lactate dehydrogenasebased rapid tests for Plasmodium knowlesi and P. falciparum. Front Cell Infect Microbiol 2022;12:1023219.
16. WHO. Malaria rapid diagnostic test performance. Results of WHO product testing of malaria RDTs: round 8 (2016-2018). Geneva: World Health Oragnization;2018:172.
17. Maltha J, Gillet P, Jacobs J. Malaria rapid diagnostic tests in endemic settings. Clin Microbiol Infect 2013;19:399-407.
18. Bwire GM, Ngasala B, Kilonzi M, Mikomangwa WP, Felician FF, Kamuhabwa AAR. Diagnostic performance of CareStart malaria HRP2/pLDH test in comparison with standard microscopy for detection of uncomplicated malaria infection among symptomatic patients, Eastern Coast of Tanzania. Malar J 2019;18:354.
19. Ratsimbasoa A, Randriamanantena A, Raherinjafy R, Rasoarilalao N, Menard D. Which malaria rapid test for Madagascar? Field and laboratory evaluation of three tests and expert microscopy of samples from suspected malaria patients in Madagascar. Am J Trop Med Hyg 2007;76:481-5.
20. Abba K, Deeks JJ, Olliaro P, Naing CM, Jackson SM, Takwoingi Y, et al. Rapid diagnostic tests for diagnosing uncomplicated P. falciparum malaria in endemic countries. Cochrane Database Syst Rev 2011;2011:CD008122.
21. Abba K, Kirkham AJ, Olliaro PL, Deeks JJ, Donegan S, Garner P, et al. Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or Plasmodium vivax malaria in endemic countries. Cochrane Database Syst Rev 2014;2014:CD011431.
22. Shapiro HM, Apte SH, Chojnowski GM, Hanscheid T, Rebelo M, Grimberg BT. Cytometry in malaria—a practical replacement for microscopy? Curr Protoc Cytom 2013;Chapter 11:11.20.1-11.20.23.
23. Grimberg BT, Erickson JJ, Sramkoski RM, Jacobberger JW, Zimmerman PA. Monitoring Plasmodium falciparum growth and development by UV flow cytometry using an optimized Hoechst-thiazole orange staining strategy. Cytometry A 2008;73:546-54.
24. Malleret B, Claser C, Ong AS, Suwanarusk R, Sriprawat K, Howland SW, et al. A rapid and robust tri-color flow cytometry assay for monitoring malaria parasite development. Sci Rep 2011;1:118.
25. Tiendrebeogo RW, Adu B, Singh SK, Dodoo D, Dziegiel MH, Mordmuller B, et al. Highthroughput tri-colour flow cytometry technique to assess Plasmodium falciparum parasitaemia in bioassays. Malar J 2014;13:412.
26. Hanscheid T, Valadas E, Grobusch MP. Automated malaria diagnosis using pigment detection. Parasitol Today 2000;16:549-51.
27. Frita R, Rebelo M, Pamplona A, Vigario AM, Mota MM, Grobusch MP, et al. Simple flow cytometric detection of haemozoin containing leukocytes and erythrocytes for research on diagnosis, immunology and drug sensitivity testing. Malar J 2011;10:74.
28. Kumar R, Verma AK, Shrivas S, Thota P, Singh MP, Rajasubramaniam S, et al. First successful field evaluation of new, one-minute haemozoin-based malaria diagnostic device. EClinicalMedicine 2020;22:100347.
29. Mendelow BV, Lyons C, Nhlangothi P, Tana M, Munster M, Wypkema E, et al. Automated malaria detection by depolarization of laser light. Br J Haematol 1999;104:499-503.
30. Kramer B, Grobusch MP, Suttorp N, Neukammer J, Rinneberg H. Relative frequency of malaria pigment-carrying monocytes of nonimmune and semi-immune patients from flow cytometric depolarized side scatter. Cytometry 2001;45:133-40.
31. Toya Y, Tougan T, Horii T, Uchihashi K. Lysercell M enhances the detection of stage-specific Plasmodium-infected red blood cells in the automated hematology analyzer XN-31 prototype. Parasitol Int 2021;80:102206.
32. Dumas C, Bienvenu AL, Girard S, Picot S, Debize G, Durand B. Automated Plasmodium detection by the Sysmex XN hematology analyzer. J Clin Pathol 2018;71:594-9.
33. Dumas C, Tirard-Collet P, Mestrallet F, Girard S, Jallades L, Picot S, et al. Flagging performance of Sysmex XN-10 haematology analyser for malaria detection. J Clin Pathol 2020;73:676-7.
34. M’Baya B, Mfune T, Samon A, Hwandih T, Munster M. Evaluation of the Sysmex XN-31 automated analyser for blood donor malaria screening at Malawi Blood Transfusion Services. Vox Sang 2022;117:346-53.
35. Kagaya W, Takehara I, Kurihara K, Maina M, Chan CW, Okomo G, et al. Potential application of the haematology analyser XN-31 prototype for field malaria surveillance in Kenya. Malar J 2022;21:252.
36. Huggett JF, O’Sullivan DM, Cowen S, Cleveland MH, Davies K, Harris K, et al. Ensuring accuracy in the development and application of nucleic acid amplification tests (NAATs) for infectious disease. Mol Aspects Med 2024;97:101275.
37. Saiki RK, Scharf S, Faloona F, Mullis KB, Horn GT, Erlich HA, et al. Enzymatic amplification of beta-globin genomic sequences and restriction site analysis for diagnosis of sickle cell anemia. Science 1985;230:1350-4.
38. Notomi T, Okayama H, Masubuchi H, Yonekawa T, Watanabe K, Amino N, et al. Loopmediated isothermal amplification of DNA. Nucleic Acids Res 2000;28:E63.
39. Piepenburg O, Williams CH, Stemple DL, Armes NA. DNA detection using recombination proteins. PLoS Biol 2006;4:e204.
40. Compton J. Nucleic acid sequence-based amplification. Nature 1991;350:91-2.
41. Vincent M, Xu Y, Kong H. Helicase-dependent isothermal DNA amplification. EMBO Rep 2004;5:795-800.
42. Walker GT, Fraiser MS, Schram JL, Little MC, Nadeau JG, Malinowski DP. Strand displacement amplification--an isothermal, in vitro DNA amplification technique. Nucleic Acids Res 1992;20:1691-6.
43. Kwoh DY, Davis GR, Whitfield KM, Chappelle HL, DiMichele LJ, Gingeras TR. Transcription-based amplification system and detection of amplified human immunodeficiency virus type 1 with a bead-based sandwich hybridization format. Proc Natl Acad Sci U S A 1989;86:1173-7.
44. Fire A and Xu SQ. Rolling replication of short DNA circles. Proc Natl Acad Sci U S A 1995;92:4641-5.
45. Dean FB, Hosono S, Fang L, Wu X, Faruqi AF, Bray-Ward P, et al. Comprehensive human genome amplification using multiple displacement amplification. Proc Natl Acad Sci U S A 2002;99:5261-6.
46. Zheng Z and Cheng Z. Chapter 4- advances in molecular diagnosis of malaria. Adv Clin Chem 2017;80:155-92.
47. Padley D, Moody AH, Chiodini PL, Saldanha J. Use of a rapid, single-round, multiplex PCR to detect malarial parasites and identify the species present. Ann Trop Med Parasitol 2003;97:131-7.
48. Kho WG, Chung JY, Sim EJ, Kim MY, Kim DW, Jongwutiwes S, et al. A multiplex polymerase chain reaction for a differential diagnosis of Plasmodium falciparum and Plasmodium vivax. Parasitol Int 2003;52:229-36.
49. Snounou G, Viriyakosol S, Jarra W, Thaithong S, Brown KN. Identification of the four human malaria parasite species in field samples by the polymerase chain reaction and detection of a high prevalence of mixed infections. Mol Biochem Parasitol 1993;58:283-92.
50. Singh B, Bobogare A, Cox-Singh J, Snounou G, Abdullah MS, Rahman HA. A genus- and species-specific nested polymerase chain reaction malaria detection assay for epidemiologic studies. Am J Trop Med Hyg 1999;60:687-92.
51. Hofmann N, Mwingira F, Shekalaghe S, Robinson LJ, Mueller I, Felger I. Ultra-sensitive detection of Plasmodium falciparum by amplification of multi-copy subtelomeric targets. PLoS Med 2015;12:e1001788.
52. Snounou G and Singh B. Nested PCR analysis of Plasmodium parasites. Methods Mol Med 2002;72:189-203.
53. Zimmerman PA, Mehlotra RK, Kasehagen LJ, Kazura JW. Why do we need to know more about mixed Plasmodium species infections in humans? Trends Parasitol 2004;20:440-7.
54. Berzosa P, de Lucio A, Romay-Barja M, Herrador Z, Gonzalez V, Garcia L, et al. Comparison of three diagnostic methods (microscopy, RDT, and PCR) for the detection of malaria parasites in representative samples from Equatorial Guinea. Malar J 2018;17:333.
55. Wang B, Han SS, Cho C, Han JH, Cheng Y, Lee SK, et al. Comparison of microscopy, nestedPCR, and Real-Time-PCR assays using high-throughput screening of pooled samples for diagnosis of malaria in asymptomatic carriers from areas of endemicity in Myanmar. J Clin Microbiol 2014;52:1838-45.
56. Nyunt MH, Kyaw MP, Thant KZ, Shein T, Han SS, Zaw NN, et al. Effective high-throughput blood pooling strategy before DNA extraction for detection of malaria in low-transmission settings. Korean J Parasitol 2016;54:253-9.
57. Sattabongkot J, Tsuboi T, Han ET, Bantuchai S, Buates S. Loop-mediated isothermal amplification assay for rapid diagnosis of malaria infections in an area of endemicity in Thailand. J Clin Microbiol 2014;52:1471-7.
58. Miguel-Oteo M, Jiram AI, Ta-Tang TH, Lanza M, Hisam S, Rubio JM. Nested multiplex PCR for identification and detection of human Plasmodium species including Plasmodium knowlesi. Asian Pac J Trop Med 2017;10:299-304.
59. Mangold KA, Manson RU, Koay ES, Stephens L, Regner M, Thomson RB, Jr., et al. Realtime PCR for detection and identification of Plasmodium spp. J Clin Microbiol 2005;43:243540.
60. Perandin F, Manca N, Calderaro A, Piccolo G, Galati L, Ricci L, et al. Development of a realtime PCR assay for detection of Plasmodium falciparum, Plasmodium vivax, and Plasmodium ovale for routine clinical diagnosis. J Clin Microbiol 2004;42:1214-9.
61. Rougemont M, Van Saanen M, Sahli R, Hinrikson HP, Bille J, Jaton K. Detection of four Plasmodium species in blood from humans by 18S rRNA gene subunit-based and speciesspecific real-time PCR assays. J Clin Microbiol 2004;42:5636-43.
62. Sazed SA, Kibria MG, Alam MS. An optimized real-time qPCR method for the effective detection of human malaria infections. Diagnostics (Basel) 2021;11:736.
63. Srisutham S, Saralamba N, Malleret B, Renia L, Dondorp AM, Imwong M. Four human Plasmodium species quantification using droplet digital PCR. PLoS One 2017;12:e0175771.
64. Mahendran P, Liew JWK, Amir A, Ching XT, Lau YL. Correction: droplet digital polymerase chain reaction (ddPCR) for the detection of Plasmodium knowlesi and Plasmodium vivax. Malar J 2023;22:324.
65. Han ET, Watanabe R, Sattabongkot J, Khuntirat B, Sirichaisinthop J, Iriko H, et al. Detection of four Plasmodium species by genus- and species-specific loop-mediated isothermal amplification for clinical diagnosis. J Clin Microbiol 2007;45:2521-8.
66. Han ET. Loop-mediated isothermal amplification test for the molecular diagnosis of malaria. Expert Rev Mol Diagn 2013;13:205-18.
67. Oriero EC, Jacobs J, Van Geertruyden JP, Nwakanma D, D’Alessandro U. Molecular-based isothermal tests for field diagnosis of malaria and their potential contribution to malaria elimination. J Antimicrob Chemother 2015;70:2-13.
68. Kolluri N, Klapperich CM, Cabodi M. Towards lab-on-a-chip diagnostics for malaria elimination. Lab Chip 2017;18:75-94.
52. Morris U and Aydin-Schmidt B. Performance and application of commercially available loopmediated isothermal amplification (LAMP) kits in malaria endemic and non-endemic settings. Diagnostics (Basel) 2021;11:336.
70. Picot S, Cucherat M, Bienvenu AL. Systematic review and meta-analysis of diagnostic accuracy of loop-mediated isothermal amplification (LAMP) methods compared with microscopy, polymerase chain reaction and rapid diagnostic tests for malaria diagnosis. Int J Infect Dis 2020;98:408-19.
71. Nguyen TK, Jun H, Louis JM, Mazigo E, Lee WJ, Youm HC, et al. Enhancing malaria detection in resource-limited areas: a high-performance colorimetric LAMP assay for Plasmodium falciparum screening. PLoS One 2024;19:e0298087.
72. Cordray MS and Richards-Kortum RR. A paper and plastic device for the combined isothermal amplification and lateral flow detection of Plasmodium DNA. Malar J 2015;14:472.
73. Kersting S, Rausch V, Bier FF, von Nickisch-Rosenegk M. Rapid detection of Plasmodium falciparum with isothermal recombinase polymerase amplification and lateral flow analysis. Malar J 2014;13:99.
74. Lai MY, Ooi CH, Lau YL. Rapid detection of Plasmodium knowlesi by isothermal recombinase polymerase amplification assay. Am J Trop Med Hyg 2017;97:1597-9.
75. Lalremruata A, Nguyen TT, McCall MBB, Mombo-Ngoma G, Agnandji ST, Adegnika AA, et al. Recombinase polymerase amplification and lateral flow assay for ultrasensitive detection of low-density Plasmodium falciparum infection from controlled human malaria infection studies and naturally acquired infections. J Clin Microbiol 2020;58:e01879-19. .
76. Cordray MS and Richards-Kortum RR. Emerging nucleic acid-based tests for point-of-care detection of malaria. Am J Trop Med Hyg 2012;87:223-30.
77. Choi G and Guan W. Sample-to-answer microfluidic nucleic acid testing (NAT) on lab-on-adisc for malaria detection at point of need. Methods Mol Biol 2022;2393:297-313.
78. Kshirsagar A, Choi G, Santosh V, Harvey T, Bernhards RC, Guan W. Handheld purificationfree nucleic acid testing device for point-of-need detection of malaria from whole blood. ACS Sens 2023;8:673-83.
79. Parihar A, Parihar DS, Ranjan P, Khan R. Role of microfluidics-based point-of-care testing (POCT) for clinical applications. In: Kahn R, et al. eds. Advanced microfluidics based pointof-care diagnostics. 1st ed. Boca Raton: CRC Press; 2022. p. 22.
80. Reboud J, Xu G, Garrett A, Adriko M, Yang Z, Tukahebwa EM, et al. Paper-based microfluidics for DNA diagnostics of malaria in low resource underserved rural communities. Proc Natl Acad Sci U S A 2019;116:4834-42.
81. Lehnert T and Gijs MAM. Microfluidic systems for infectious disease diagnostics. Lab Chip 2024;24:1441-93.
82. Ho M, Sathishkumar N, Sklavounos AA, Sun J, Yang I, Nichols KP, et al. Digital microfluidics with distance-based detection - a new approach for nucleic acid diagnostics. Lab Chip 2023;24:63-73.
83. Das D, Lin CW, Chuang HS. LAMP-based point-of-care biosensors for rapid pathogen detection. Biosensors (Basel) 2022;12:1068.
84. Hu S, Jie Y, Jin K, Zhang Y, Guo T, Huang Q, et al. All-in-one digital microfluidics system for molecular diagnosis with loop-mediated isothermal amplification. Biosensors (Basel) 2022;12:324.
85. Chibi M, Wasswa W, Ngongoni C, Baba E, Kalu A. Leveraging innovation technologies to respond to malaria: a systematized literature review of emerging technologies. Malar J 2023;22:40.
86. Guo X, Khalid MA, Domingos I, Michala AL, Adriko M, Rowel C, et al. Smartphone-based DNA diagnostics for malaria detection using deep learning for local decision support and blockchain technology for security. Nat Electron 2021;4:615-24.
87. Laktabai J, Platt A, Menya D, Turner EL, Aswa D, Kinoti S, et al. A mobile health technology platform for quality assurance and quality improvement of malaria diagnosis by community health workers. PLoS One 2018;13:e0191968.




 Citation
Citation Print
Print


 XML Download
XML Download