1. Pilgrim T, Piccolo R, Heg D, et al. Ultrathin-strut, biodegradable-polymer, sirolimus-eluting stents versus thin-strut, durable-polymer, everolimus-eluting stents for percutaneous coronary revascularisation: 5-year outcomes of the BIOSCIENCE randomised trial. Lancet. 2018; 392:737–746. PMID:
30170848.
2. Kufner S, Joner M, Thannheimer A, et al. Ten-year clinical outcomes from a trial of three limus-eluting stents with different polymer coatings in patients with coronary artery disease. Circulation. 2019; 139:325–333. PMID:
30586724.
3. Madhavan MV, Kirtane AJ, Redfors B, et al. Stent-related adverse events >1 year after percutaneous coronary intervention. J Am Coll Cardiol. 2020; 75:590–604. PMID:
32057373.
4. Kong MG, Han JK, Kang JH, et al. Clinical outcomes of long stenting in the drug-eluting stent era: patient-level pooled analysis from the GRAND-DES registry. EuroIntervention. 2021; 16:1318–1325. PMID:
31543496.
5. Scheller B, Speck U, Abramjuk C, Bernhardt U, Böhm M, Nickenig G. Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation. 2004; 110:810–814. PMID:
15302790.
6. Her AY, Shin ES, Bang LH, et al. Drug-coated balloon treatment in coronary artery disease: recommendations from an Asia-Pacific Consensus Group. Cardiol J. 2021; 28:136–149. PMID:
31565793.
7. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019; 40:87–165. PMID:
30165437.
8. Jeger RV, Farah A, Ohlow MA, et al. Long-term efficacy and safety of drug-coated balloons versus drug-eluting stents for small coronary artery disease (BASKET-SMALL 2): 3-year follow-up of a randomised, non-inferiority trial. Lancet. 2020; 396:1504–1510. PMID:
33091360.
9. Rissanen TT, Uskela S, Eränen J, et al. Drug-coated balloon for treatment of de-novo coronary artery lesions in patients with high bleeding risk (DEBUT): a single-blind, randomised, non-inferiority trial. Lancet. 2019; 394:230–239. PMID:
31204115.
10. Lee SY, Cho YK, Kim SW, et al. Clinical results of drug-coated balloon treatment in a large-scale multicenter Korean registry study. Korean Circ J. 2022; 52:444–454. PMID:
35491479.
11. Ellis SG, Roubin GS, King SB 3rd, et al. Angiographic and clinical predictors of acute closure after native vessel coronary angioplasty. Circulation. 1988; 77:372–379. PMID:
2962787.
12. Cappelletti A, Margonato A, Rosano G, et al. Short- and long-term evolution of unstented nonocclusive coronary dissection after coronary angioplasty. J Am Coll Cardiol. 1999; 34:1484–1488. PMID:
10551696.
13. Leimgruber PP, Roubin GS, Anderson HV, et al. Influence of intimal dissection on restenosis after successful coronary angioplasty. Circulation. 1985; 72:530–535. PMID:
3160507.
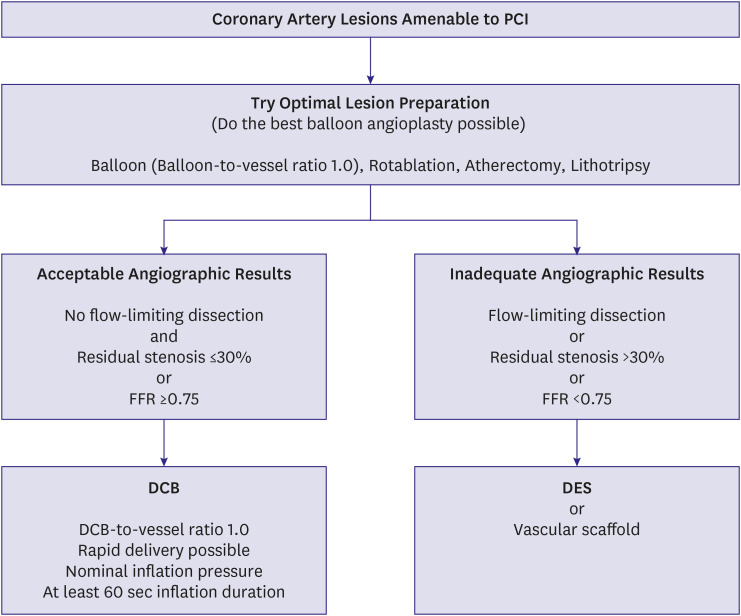
14. Jeger RV, Eccleshall S, Wan Ahmad WA, et al. Drug-coated balloons for coronary artery disease: third report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020; 13:1391–1402. PMID:
32473887.
15. Shin ES, Ann SH, Balbir Singh G, Lim KH, Kleber FX, Koo BK. Fractional flow reserve-guided paclitaxel-coated balloon treatment for de novo coronary lesions. Catheter Cardiovasc Interv. 2016; 88:193–200. PMID:
26423017.
16. Chung JH, Lee KE, Her AY, et al. Comparison of fractional flow reserve and angiographic characteristics after balloon angioplasty in de novo coronary lesions. Int J Cardiovasc Imaging. 2019; 35:1945–1954. PMID:
31214851.
17. Chung JH, Shin ES, Her AY, et al. Instantaneous wave-free ratio-guided paclitaxel-coated balloon treatment for de novo coronary lesions. Int J Cardiovasc Imaging. 2020; 36:179–185. PMID:
31598811.
18. Shin ES, Ann SH, Jang MH, et al. Impact of scoring balloon angioplasty on lesion preparation for DCB treatment of coronary lesions. J Clin Med. 2023; 12:6254. PMID:
37834898.
19. Ueno K, Morita N, Kojima Y, et al. Safety and long-term efficacy of drug-coated balloon angioplasty following rotational atherectomy for severely calcified coronary lesions compared with new generation drug-eluting stents. J Interv Cardiol. 2019; 2019:9094178. PMID:
31772551.
20. Lv S, Ma X, Zhou Y, et al. Intracoronary imaging versus coronary angiography to guide drug-coated balloon intervention in coronary artery disease: a propensity-matched pilot study analysis. Angiology. 2021; 72:971–978. PMID:
33957806.
21. Tanaka A, Latib A, Jabbour RJ, et al. Impact of angiographic result after predilatation on outcome after drug-coated balloon treatment of in-stent coronary restenosis. Am J Cardiol. 2016; 118:1460–1465. PMID:
27634028.
22. Her AY, Yuan SL, Jun EJ, et al. Drug-coated balloon treatment for nonsmall de-novo coronary artery disease: angiographic and clinical outcomes. Coron Artery Dis. 2021; 32:534–540. PMID:
33471480.
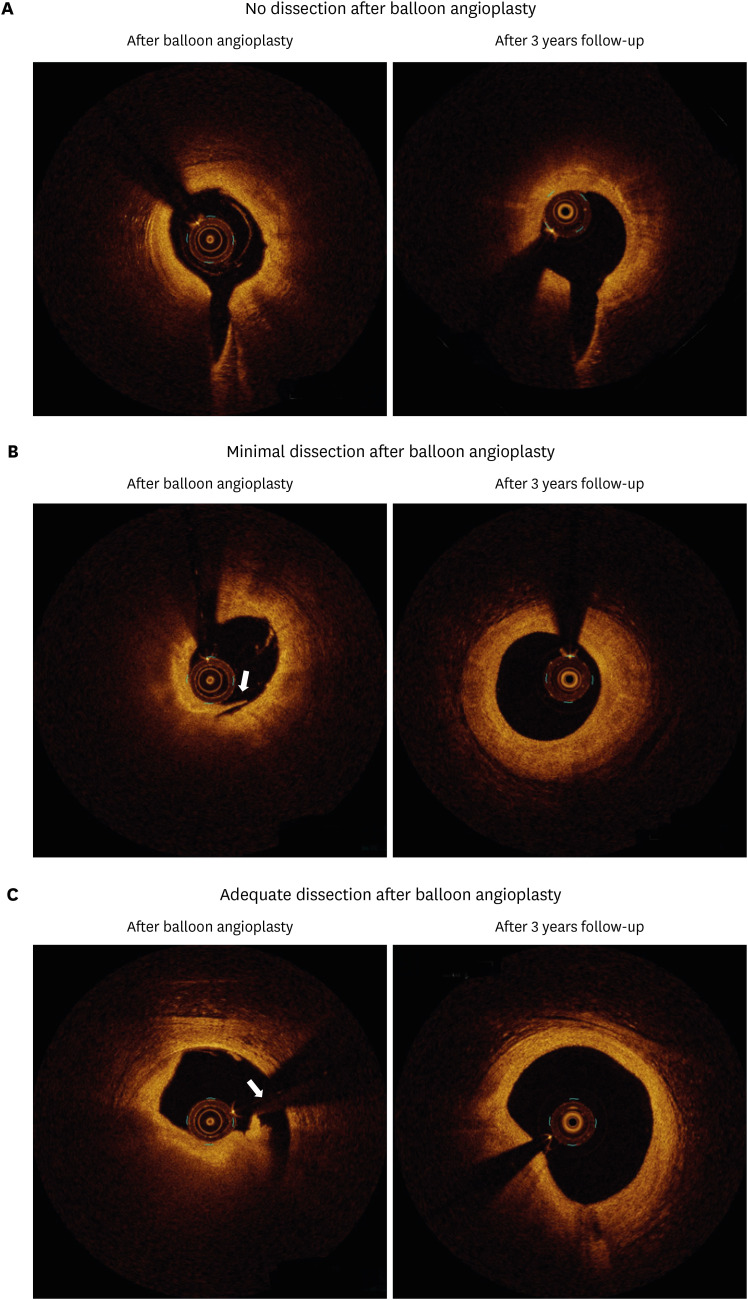
23. Hui L, Shin ES, Jun EJ, et al. Impact of dissection after drug-coated balloon treatment of de novo coronary lesions: angiographic and clinical outcomes. Yonsei Med J. 2020; 61:1004–1012. PMID:
33251774.
24. Shin ES, Jun EJ, Kim B. Vascular remodeling after drug-coated balloon treatment: insight from optical coherence tomography. Korean Circ J. 2023; 53:191–193. PMID:
36914609.
25. Ann SH, Balbir Singh G, Lim KH, Koo BK, Shin ES. Anatomical and physiological changes after paclitaxel-coated balloon for atherosclerotic de novo coronary lesions: serial IVUS-VH and FFR study. PLoS One. 2016; 11:e0147057. PMID:
26824602.
26. Ann SH, Her AY, Singh GB, Okamura T, Koo BK, Shin ES. Serial morphological and functional assessment of the paclitaxel-coated balloon for de novo lesions. Rev Esp Cardiol (Engl Ed). 2016; 69:1026–1032. PMID:
27321644.
27. Lee HS, Kang J, Park KW, et al. Procedural optimization of drug-coated balloons in the treatment of coronary artery disease. Catheter Cardiovasc Interv. 2021; 98:E43–E52. PMID:
33491857.
28. Claessen BE, Smits PC, Kereiakes DJ, et al. Impact of lesion length and vessel size on clinical outcomes after percutaneous coronary intervention with everolimus- versus paclitaxel-eluting stents pooled analysis from the SPIRIT (Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System) and COMPARE (Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice) randomized trials. JACC Cardiovasc Interv. 2011; 4:1209–1215. PMID:
22115661.
29. van der Heijden LC, Kok MM, Danse PW, et al. Small-vessel treatment with contemporary newer-generation drug-eluting coronary stents in all-comers: insights from 2-year DUTCH PEERS (TWENTE II) randomized trial. Am Heart J. 2016; 176:28–35. PMID:
27264217.
30. Cortese B, Di Palma G, Guimaraes MG, et al. Drug-coated balloon versus drug-eluting stent for small coronary vessel disease: PICCOLETO II randomized clinical trial. JACC Cardiovasc Interv. 2020; 13:2840–2849. PMID:
33248978.
31. Kiyohara Y, Aikawa T, Kayanuma K, et al. Comparison of clinical outcomes among various percutaneous coronary intervention strategies for small coronary artery disease. Am J Cardiol. 2024; 211:334–342. PMID:
37984638.
32. Venetsanos D, Lawesson SS, Panayi G, et al. Long-term efficacy of drug coated balloons compared with new generation drug-eluting stents for the treatment of de novo coronary artery lesions. Catheter Cardiovasc Interv. 2018; 92:E317–E326. PMID:
29481718.
33. Toelg R, Merkely B, Erglis A, et al. Coronary artery treatment with paclitaxel-coated balloon using a BTHC excipient: clinical results of the international real-world DELUX registry. EuroIntervention. 2014; 10:591–599. PMID:
24345357.
34. Uskela S, Kärkkäinen JM, Eränen J, et al. Percutaneous coronary intervention with drug-coated balloon-only strategy in stable coronary artery disease and in acute coronary syndromes: an all-comers registry study. Catheter Cardiovasc Interv. 2019; 93:893–900. PMID:
30380186.
35. Her AY, Shin ES, Lee JM, et al. Paclitaxel-coated balloon treatment for functionally nonsignificant residual coronary lesions after balloon angioplasty. Int J Cardiovasc Imaging. 2018; 34:1339–1347. PMID:
29696453.
36. Her AY, Shin ES, Chung JH, et al. Plaque modification and stabilization after paclitaxel-coated balloon treatment for de novo coronary lesions. Heart Vessels. 2019; 34:1113–1121. PMID:
30701291.
37. Poerner TC, Duderstadt C, Goebel B, Kretzschmar D, Figulla HR, Otto S. Fractional flow reserve-guided coronary angioplasty using paclitaxel-coated balloons without stent implantation: feasibility, safety and 6-month results by angiography and optical coherence tomography. Clin Res Cardiol. 2017; 106:18–27. PMID:
27379610.
38. Hu FW, Chang S, Li Q, et al. Long-term clinical outcomes after percutaneous coronary intervention with drug-coated balloon-only strategy in de novo lesions of large coronary arteries. Front Cardiovasc Med. 2022; 9:882303. PMID:
35911516.
39. Gitto M, Sticchi A, Chiarito M, et al. Drug-coated balloon angioplasty for de novo lesions on the left anterior descending artery. Circ Cardiovasc Interv. 2023; 16:e013232. PMID:
37874646.
40. Lin Y, Sun X, Liu H, Pang X, Dong S. Drug-coated balloon versus drug-eluting stent for treating de novo coronary lesions in large vessels: a meta-analysis of clinical trials. Herz. 2021; 46:269–276. PMID:
32468141.
41. Park TK, Park YH, Song YB, et al. Long-term clinical outcomes of true and non-true bifurcation lesions according to medina classification- results from the COBIS (COronary BIfurcation Stent) II registry. Circ J. 2015; 79:1954–1962. PMID:
26134457.
42. Pan M, Lassen JF, Burzotta F, et al. The 17th expert consensus document of the European Bifurcation Club – techniques to preserve access to the side branch during stepwise provisional stenting. EuroIntervention. 2023; 19:26–36. PMID:
37170568.
43. Kleber FX, Rittger H, Ludwig J, et al. Drug eluting balloons as stand alone procedure for coronary bifurcational lesions: results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 2016; 105:613–621. PMID:
26768146.
44. Corballis NH, Paddock S, Gunawardena T, Merinopoulos I, Vassiliou VS, Eccleshall SC. Drug coated balloons for coronary artery bifurcation lesions: a systematic review and focused meta-analysis. PLoS One. 2021; 16:e0251986. PMID:
34242214.
45. Her AY, Ann SH, Singh GB, et al. Serial morphological changes of side-branch ostium after paclitaxel-coated balloon treatment of de novo coronary lesions of main vessels. Yonsei Med J. 2016; 57:606–613. PMID:
26996558.
46. Pan L, Lu W, Han Z, et al. Drug-coated balloon in the treatment of coronary left main true bifurcation lesion: a patient-level propensity-matched analysis. Front Cardiovasc Med. 2022; 9:1028007. PMID:
36407423.
47. Okutsu M, Mitomo S, Ouchi T, et al. Impact of directional coronary atherectomy followed by drug-coated balloon strategy to avoid the complex stenting for bifurcation lesions. Heart Vessels. 2022; 37:919–930. PMID:
34981167.
48. Kitani S, Igarashi Y, Tsuchikane E, et al. Efficacy of drug-coated balloon angioplasty after directional coronary atherectomy for coronary bifurcation lesions (DCA/DCB registry). Catheter Cardiovasc Interv. 2021; 97:E614–E623. PMID:
32776689.
49. Costopoulos C, Latib A, Naganuma T, et al. The role of drug-eluting balloons alone or in combination with drug-eluting stents in the treatment of de novo diffuse coronary disease. JACC Cardiovasc Interv. 2013; 6:1153–1159. PMID:
24262615.
50. Yang X, Lu W, Pan L, et al. Long-term outcomes of drug-coated balloons in patients with diffuse coronary lesions. Front Cardiovasc Med. 2022; 9:935263. PMID:
36211569.
51. Shin ES, Jun EJ, Kim S, et al. Clinical impact of drug-coated balloon-based percutaneous coronary intervention in patients with multivessel coronary artery disease. JACC Cardiovasc Interv. 2023; 16:292–299. PMID:
36609038.
52. Lee CW, Park DW, Lee BK, et al. Predictors of restenosis after placement of drug-eluting stents in one or more coronary arteries. Am J Cardiol. 2006; 97:506–511. PMID:
16461047.
53. Mieres J, Fernandez-Pereira C, Risau G, et al. One-year outcome of patients with diabetes mellitus after percutaneous coronary intervention with three different revascularization strategies: results from the Diabetic Argentina Registry (DEAR). Cardiovasc Revasc Med. 2012; 13:265–271. PMID:
22796496.
54. Wöhrle J, Scheller B, Seeger J, et al. Impact of diabetes on outcome with drug-coated balloons versus drug-eluting stents: the BASKET-SMALL 2 trial. JACC Cardiovasc Interv. 2021; 14:1789–1798. PMID:
34412797.
55. Her AY, Shin ES, Kim S, et al. Drug-coated balloon-based versus drug-eluting stent-only revascularization in patients with diabetes and multivessel coronary artery disease. Cardiovasc Diabetol. 2023; 22:120. PMID:
37210516.
56. Sharp AS, Latib A, Ielasi A, et al. Long-term follow-up on a large cohort of “full-metal jacket” percutaneous coronary intervention procedures. Circ Cardiovasc Interv. 2009; 2:416–422. PMID:
20031751.
57. Lee PH, Lee SW, Yun SC, et al. Full metal jacket with drug-eluting stents for coronary chronic total occlusion. JACC Cardiovasc Interv. 2017; 10:1405–1412. PMID:
28668311.
58. Wöhrle J, Werner GS. Paclitaxel-coated balloon with bare-metal stenting in patients with chronic total occlusions in native coronary arteries. Catheter Cardiovasc Interv. 2013; 81:793–799. PMID:
22511572.
59. Jun EJ, Shin ES, Teoh EV, et al. Clinical outcomes of drug-coated balloon treatment after successful revascularization of de novo chronic total occlusions. Front Cardiovasc Med. 2022; 9:821380. PMID:
35498010.
60. Sung JG, Lo ST, Lam H. Contemporary interventional approach to calcified coronary artery disease. Korean Circ J. 2023; 53:55–68. PMID:
36792557.
61. Stone SG, Serrao GW, Mehran R, et al. Incidence, predictors, and implications of reinfarction after primary percutaneous coronary intervention in ST-segment-elevation myocardial infarction: the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial. Circ Cardiovasc Interv. 2014; 7:543–551. PMID:
24939928.
62. Vos NS, Fagel ND, Amoroso G, et al. Paclitaxel-coated balloon angioplasty versus drug-eluting stent in acute myocardial infarction: the REVELATION randomized trial. JACC Cardiovasc Interv. 2019; 12:1691–1699. PMID:
31126887.
63. Scheller B, Ohlow MA, Ewen S, et al. Bare metal or drug-eluting stent versus drug-coated balloon in non-ST-elevation myocardial infarction: the randomised PEPCAD NSTEMI trial. EuroIntervention. 2020; 15:1527–1533. PMID:
31659986.
64. Kondo Y, Ishikawa T, Shimura M, et al. Cardiovascular outcomes after paclitaxel-coated balloon angioplasty versus drug-eluting stent placement for acute coronary syndrome: a systematic review and meta-analysis. J Clin Med. 2024; 13:1481. PMID:
38592314.
65. Palmerini T, Della Riva D, Benedetto U, et al. Three, six, or twelve months of dual antiplatelet therapy after DES implantation in patients with or without acute coronary syndromes: an individual patient data pairwise and network meta-analysis of six randomized trials and 11 473 patients. Eur Heart J. 2017; 38:1034–1043. PMID:
28110296.
66. Shin ES, Lee JM, Her AY, et al. Prospective randomized trial of paclitaxel-coated balloon versus bare-metal stent in high bleeding risk patients with de novo coronary artery lesions. Coron Artery Dis. 2019; 30:425–431. PMID:
31009399.
67. Rowinsky EK, Donehower RC. Paclitaxel (taxol). N Engl J Med. 1995; 332:1004–1014. PMID:
7885406.
68. Clever YP, Cremers B, Krauss B, et al. Paclitaxel and sirolimus differentially affect growth and motility of endothelial progenitor cells and coronary artery smooth muscle cells. EuroIntervention. 2011; 7(Suppl K):K32–K42. PMID:
22027725.
69. Verheye S, Vrolix M, Kumsars I, et al. The SABRE Trial (Sirolimus Angioplasty Balloon for Coronary In-Stent Restenosis): angiographic results and 1-year clinical outcomes. JACC Cardiovasc Interv. 2017; 10:2029–2037. PMID:
28964764.
70. Scheller B, Mangner N, Abdul Kader MA, et al. Combined analysis of two parallel randomized trials of sirolimus-coated and paclitaxel-coated balloons in coronary in-stent restenosis lesions. Circ Cardiovasc Interv. 2022; 15:e012305. PMID:
36126132.
71. Cortese B, Testa L, Heang TM, et al. Sirolimus-coated balloon in an all-comer population of coronary artery disease patients: the EASTBOURNE prospective registry. JACC Cardiovasc Interv. 2023; 16:1794–1803. PMID:
37495352.
72. Stettler C, Wandel S, Allemann S, et al. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007; 370:937–948. PMID:
17869634.
73. Ahmad WA, Nuruddin AA, Abdul Kader MA, et al. Treatment of coronary de novo lesions by a sirolimus- or paclitaxel-coated balloon. JACC Cardiovasc Interv. 2022; 15:770–779. PMID:
35305906.
74. Ninomiya K, Serruys PW, Colombo A, et al. A prospective randomized trial comparing sirolimus-coated balloon with paclitaxel-coated balloon in de novo small vessels. JACC Cardiovasc Interv. 2023; 16:2884–2896. PMID:
37877914.
75. Gao XF, Ge Z, Kan J, et al. Rationale and design for comparison of non-compliant balloon with drug-coating balloon angioplasty for side branch after provisional stenting for patients with true coronary bifurcation lesions: a prospective, multicentre and randomised DCB-BIF trial. BMJ Open. 2022; 12:e052788.
76. Greco A, Sciahbasi A, Abizaid A, et al. Sirolimus-coated balloon versus everolimus-eluting stent in de novo coronary artery disease: rationale and design of the TRANSFORM II randomized clinical trial. Catheter Cardiovasc Interv. 2022; 100:544–552. PMID:
36054266.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download