Abstract
Purpose
This study aimed to compare the results of patients who underwent anterior component separation techniques (ACST) and those who did not undergo component separation techniques (non-CST) in complicated ventral hernia repairs (VHRs) and to investigate the effect of these techniques on quality of life (QoL).
Methods
A total of 105 patients who were operated for large ventral hernias were retrospectively analyzed. The patients were divided into the ACST group (n = 48) and the non-CST group (n = 57). Demographic, intraoperative, and postoperative data were recorded. Postoperative follow-up was conducted at 2 and 4 weeks, and 6, 12, and 24 months. The primary and secondary outcomes and QoL were measured.
Results
The female ratio was higher in both groups (P = 0.512). There was no significant difference between age and body mass index between the groups (P = 0.705 and P = 0.803). The mean defect size and mesh size were similar between the groups (P = 0.775 and P = 0.245). The mean operation duration and amount of blood loss were similar between the groups (P = 0.801 and P = 0.142). There was no statistically significant difference in the median visual analog scale scores between the groups (P = 0.551). During follow-up, only 3 patients (6.3%) in the ACST group and 4 patients (7.0%) in the non-CST group had recurrence. There was no significant difference in the short- and long-term QoL between the groups.
In the United States, about 350,000 ventral hernia repairs (VHRs) are performed annually with the diagnosis of ventral hernia (VH) [1]. The definition of standard VHs and complicated ventral (abdominal wall) hernias are still lacking, although these terms are often used. In general, VHs can be classified according to the size and location of the hernia, contamination, soft tissue condition, patient history, and risk factors. Standard VHs can be defined as uncomplicated incisional or recurrent hernias smaller than <10 cm in size. Large or complicated hernias can be defined as >10 cm, >20% more fascial defect, and multiple simultaneous abdominal wall hernias [2]. In such cases, problems such as chronic low back pain, respiratory failure, and altered body image may occur. Surgical repair is indicated for patients with such defects or symptoms related to incisional hernia [3]. The ideal method to prevent recurrence in small and medium-sized VHs is repair with a mesh [45]. In large-sized and complicated VHs, the use of component separation techniques (CSTs) in closing the defect without tension helps considerably to ensure abdominal integrity [67]. Open CST in complex VHs has been a widely used technique since the 1990s [8]. This technique provides tension-free closure of myofascial advancement flaps by making a sharp division of both external oblique aponeuroses without interrupting the innervations and blood flow of the muscles. Wound complications of up to 60% may develop due to extensive dissection from medial to lateral in the subcutaneous region and deterioration of vascularization of perforating vessels [910].
Furthermore, complicated VH creates psychological problems in patients due to impaired physical appearance and pain, thereby impairing the quality of life (QoL) of patients. Therefore, the surgeon should attempt to ensure abdominal integrity using CST and improve the QoL of patients, particularly in complicated VH.
In the present study, we aimed to compare the short and long-term results of patients who underwent anterior CST (ACST) and those who did not undergo CST (non-CST) in complicated and large VHRs and to investigate the effect of these techniques on QoL.
This study protocol was approved by the Ethics Committee of University of Health Sciences, Erzurum Faculty of Medicine (No. 2023/03-32). The study was conducted in accordance with the principles of the Declaration of Helsinki. A written informed consent was obtained from each patient for all diagnostic and therapeutic procedures.
This multicenter, retrospective study was conducted at 3 centers between April 2017 and March 2023. Patients who underwent surgery with the diagnosis of large and complicated VHs were screened. Patients who received ACST and who did not receive ACST were identified. All operations were performed by 3 surgeons.
Defects that were not contaminated (the Centers for Disease Control and Prevention [CDC] class I) and larger than 100 cm2 were included in the study. Patients with missing follow-up data and those who underwent emergency surgery were excluded. All patients underwent abdominal CT before surgery. The defect diameter was decided by measuring intraoperatively. Demographic data, intraoperative, and postoperative data were recorded. Postoperative follow-up was conducted in the outpatient setting at 2 and 4 weeks, and 6, 12, and 24 months. Patients who did not attend the follow-up were reached by phone and their data were updated.
The primary outcome measure was hernia recurrence. The secondary outcome measures were duration of operation, amount of blood loss, mesh size, number of drains inserted, time to drain removal, pain scores, length of hospital stay (LOS), wound and mesh-related seroma, hematoma, infection, wound grade, mortality, and QoL. The pain was measured on the night of the operation and day 1 after surgery using the visual analog scale (VAS). The scores range from no pain “0” to worst pain “10.” The wound was graded by the CDC classification: I, normal wound; II, erythema and swelling; III, purulent effluent; and IV, open wound. Postoperative morbidity was classified according to the Clavien-Dindo (CD) classification [11].
The Carolinas Comfort Scale (CCS) is a scale system that evaluates the QoL of patients undergoing hernia repair with mesh [121314]. It measures QoL by questioning pain, mesh sensitivity, and movement limitation during 8 activities. These activities include lying down, bending over, sitting up, daily living, coughing/breathing, walking, walking upstairs, and exercising. Each question is scored on a 5-point Likert scale: 0, no symptoms to 5, disabling symptoms [15]. It has been shown that the CCS is more effective in determining QoL for hernia and is preferred by patients more often than the Short Form-36 [13].
All surgeries were performed under general anesthesia and in the supine position. The incision was made based on the presence of previous surgical scars, rather than the hernia. After the hernia sac was dissected, its contents were returned to the abdomen. The width of the defect was measured. Dissection was, then, continued about 2–5 cm lateral to the linea semilunaris on both sides, about 2–5 cm lateral to the costal margins above, and 2–5 cm lateral to the symphysis pubis below. The ACST was made with a 1-cm lateral vertical incision parallel to the linea semilunaris, with incisions extending from the costal margin to the inguinal region on one or both sides as needed (Fig. 1). Continuous closure of the linea alba was performed using 1/0 polypropylene to create a gap in the external oblique aponeurosis incision on one or both sides and provide tension-free midline closure. Next, a 2/0 polypropylene fixation suture was made by placing a wide polypropylene mesh only extending from the upper costal margins to the symphysis pubis below and extending at least approximately 5 cm beyond the lateral edge of the external oblique aponeurosis, covering the midline fascial closure. The skin was closed and the Jackson-Pratt drains were placed on both sides.
Descriptive statistics were reported as means with corresponding standard deviations for continuous variables and percentages for categorical variables. Categorical variables were evaluated using the Pearson chi-square and the Fisher exact tests where appropriate. Continuous and ordinal variables were evaluated using the Wilcoxon-Mann-Whitney and the Kruskal-Wallis tests. Statistical significance was set at P < 0.05, and all reported P-values were 2-tailed. All data were analyzed using SAS software ver. 9.4 (SAS Institute).
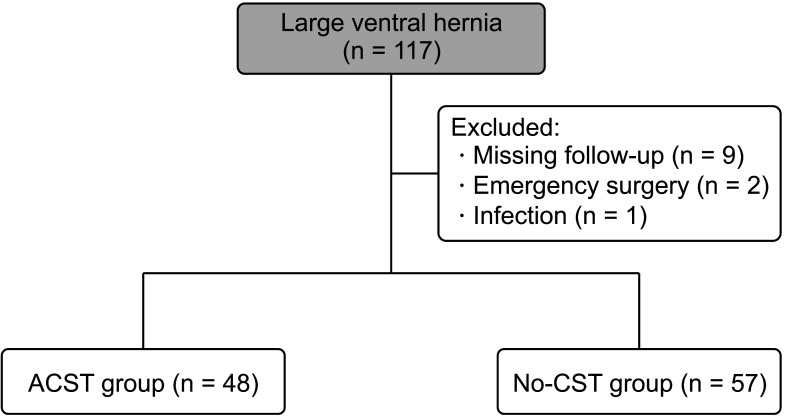
Of a total of 117 patients who were operated on for VH, 12 were excluded due to emergency surgery, infection, or missing follow-up data. The patients were divided into the ACST group (n = 48, 45.7%) and the non-CST group (n = 57, 54.3%). The study flowchart is shown in Fig. 2.
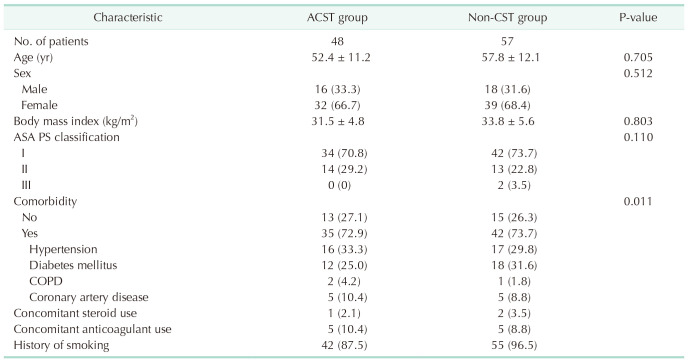
The female ratio was higher in both groups (66.7% vs. 68.4%, P = 0.512). There was no significant difference between age and body mass index between the groups (P = 0.705 and P = 0.803, respectively). In addition, the American Society of Anesthesiologists physical status classification and comorbidities were similar. The demographic and baseline characteristics of the patients are summarized in Table 1.
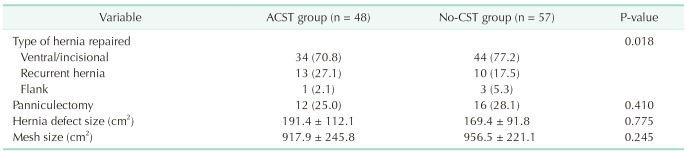
The proportion of ventral/incisional hernia was higher in both groups (70.8% vs. 77.2%, P = 0.018). The mean defect size and mesh size were similar between the groups (P = 0.775 and P = 0.245, respectively). VH and hernia-related characteristics are shown in Table 2.
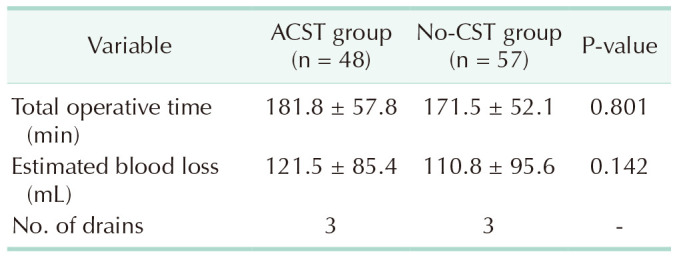
The mean operation duration was 181.8 ± 57.8 minutes in the ACST group and 171.5 ± 52.1 minutes in the non-CST group (P = 0.801). The mean amount of blood loss was 121.5 ± 85.4 mL in the ACST group and 110.8 ± 95.6 mL in the non-CST group indicating no statistically significant difference (P = 0.142). Operative data are summarized in Table 3.
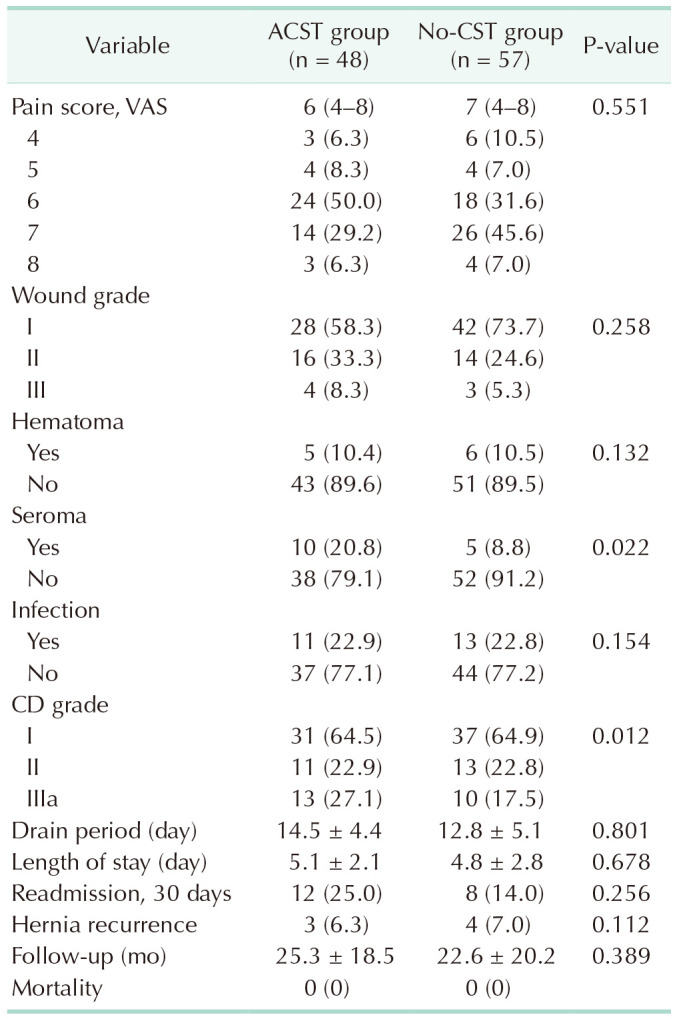
There was no statistically significant difference in the median VAS scores between the groups (P = 0.551). Although the wound grade II–II was more common in the ACST group, it did not reach statistical significance (P = 0.258). The mean time to drain removal was also comparable between the groups (P = 0.801). Five patients (10.4%) had hematoma, 10 patients (20.8%) had seroma, and 11 patients (22.9%) had surgical site infection in the ACST group. No additional intervention was performed in patients who developed a hematoma, and these patients were closely followed. No erythrocyte suspension transfusion was administered to any of the patients, as there was no massive bleeding. Bedside drainage was attempted for 10 patients who developed seroma after drain removal. Wound debridement was applied to three of 11 patients (22.9%) who developed surgical site infection and all patients were initiated on systemic antibiotherapy. Six patients (10.5%) developed hematoma, 5 patients (8.8%) developed seroma, and 13 patients (22.8%) developed surgical site infections in the non-CST group. The patients who developed hematoma were closely followed. Similarly, bedside drainage was attempted for the patients who developed seroma after drain removal. Five patients who had surgical site infection underwent wound debridement and all these patients were initiated systemic antibiotherapy.
A total of 31 patients (64.6%) in the ACST group and 37 patients (64.9%) in the non-CST group had CD grade I complications. None of these patients received additional surgical or medical treatment. The patients who had Grade II complications were initiated extended systemic antibiotherapy. The patients who had CD grade III complications underwent surgical intervention under local anesthesia (P = 0.012).
There was no significant difference in the LOS between the groups. No mortality was observed in any of the patients. The mean follow-up was 25.3 ± 18.5 months in the ACST group and 22.6 ± 20.2 months in the non-CST group (P = 0.389). During follow-up, only 3 patients (6.3%) in the ACST group and 4 patients (7.0%) in the non-CST group had recurrence. Recurrence occurred in the 6, 10, and 16 months in the ACST group and the 12, 15, 16, and 20 months in the non-CST group. Postoperative data, surgical morbidities, and follow-up data are summarized in Table 4.
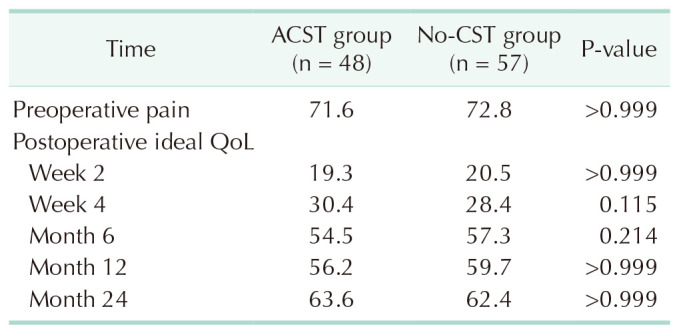
The QoL of the patients was assessed using the CCS. Accordingly, pain was the most common complaint in both groups in the preoperative period. The QoL was assessed at 2 and 4 weeks and 6, 12, 24 months postoperatively. There was no significant difference in the short- and long-term QoL between the groups (P > 0.999). At 24 months, 63.6% of the patients in the ACST group and 62.4% of the patients in the non-CST group had improved QoL close to normal (Table 5).
Abdominal wall hernia is one of the common surgical diseases that require repair [1]. Complicated and large VHs can cause serious problems in patients with chronic back and abdominal pain, respiratory failure, and altered body image. Complicated VHs are prone to expansion [16]. Therefore, as the hernia grows, complaints increase, repairs become more difficult, and postoperative morbidity and mortality risks increase. The main goal in such large hernias is to close the abdominal wall fascia without tension and prevent the intraabdominal pressure from increasing [17]. Repair of the abdominal wall with mesh under tension increases recurrence and wound complications [18]. The CST is a technique that performs tension-free repair with myofascial mobilization for midline closure of large and complicated hernias and was first described by Ramirez et al. [8]. In our study, the results of repairing large and complicated VHs with ACST and non-CST and standard mesh were compared. In the ACST group, 20 patients had VHs that developed after obstetric surgery, 15 after laparotomy for colon cancer, and 13 after recurrent incisional hernia. In the non-CST group, 28 obstetric patients, 19 post-colon cancer surgery patients, and 10 patients with recurrence underwent incisional hernia repair. Demographic characteristics, hernia characteristics, and surgery data were comparable between the groups. Patients with large hernias often had associated comorbidities such as obesity, diabetes mellitus, and cardiorespiratory problems.
Several studies have shown that the size of the hernia defect is of utmost importance in predicting the risks of postoperative complications [19]. In our study, defects larger than 100 cm2 in diameter were repaired. Although the surgery time was longer and blood loss was higher in the ACST group, there was no statistically significant difference between the groups. Due to extensive dissection, 2 Jackson-Pratt drains (10 mm each) were placed subcutaneously in both groups to prevent postoperative hematoma and seroma. No significant difference was observed between the groups in the postoperative VAS scores. Wound complications are the most common complication of hernia repair in ACST, ranging from 0% to 50%. Higher infection rates are observed in obese patients [20]. Wound complications and seromas are more common in ACST patients compared to non-CST due to extensive subcutaneous dissection. Maloney et al. [10] reported a wound complication rate of 42.9% after ACST in their study. In our study, wound complications developed in 11 patients (22.9%) in the ACST group and 13 patients (22.8%) in the non-CST group. There are studies reporting bedside aspiration or drain placement due to seroma with a rate of 14% to 21% [2122]. In our study, although postoperative hematoma development (10.4% vs. 10.5%) was similar between the groups, seroma development (20.8% vs. 8.8%) was more common in the ACST group, consistent with the literature. Therefore, according to the CD classification, the ACST group statistically significantly needed more invasive procedures. However, there was no statistically significant difference in the wound grade between the groups.
Several studies have demonstrated that the laparoscopic CST technique is safer in preventing such complications. However, it has been abandoned by many surgeons recently due to its technical difficulty, limited myofascial release, and frequent seroma development in the lateral region [23]. In addition, posterior CST may be one of the preferred options in complicated VHR due to lower complication and recurrence rates. Posterior CST is associated with other challenges, including technical difficulty in performing the procedure, the risk of damaging the posterior sheath and allowing the bowel to contact mesh, and the risk of denervating the rectus complex) [24].
Although the main goal of hernia repair is to prevent recurrence, surgical results affect the lifelong QoL of patients. Depending on the surgical technique, abdominal pain, discomfort, and cosmetic results are the factors that indicate the success of the surgery. Therefore, we can evaluate the ideal QoL using CCS for short and long-term surgery results. Using the CCS, it is possible to compare and evaluate the pre- and postoperative results of hernia repairs performed using different techniques. In CCS, particularly pain, movement limitation, and mesh sensitivity play a key role in determining QoL [1417252627]. To the best of our knowledge, there are few studies in the literature evaluating QoL after CST. Klima et al. [27] evaluated QoL in the short and long-term follow-up after CST and standard VHR using CCS and obtained similar results between the groups. Maloney et al. [10] compared patients with and without CST for VHR and reported that QoL improved in patients who underwent CST. Similar results were obtained in our study and QoL improved in patients who underwent ACST. However, no statistically significant difference was observed between the groups with and without ACST after short and long-term follow-up. The recurrence rates after ACST range from 7% to 32% in previous studies [23242528]. Sailes et al. [29] reported a relapse rate of 18.5% over a 10-year period. In our study, recurrence rates were found to be consistent with the literature and no statistically significant difference was found between the groups. No mortality was observed in any of the patients.
Nonetheless, there are some limitations to this study. First, the main limitations include its retrospective design with a relatively small sample size. Second, there were no laparoscopic ACST cases in this study. Further large-scale, long-term, prospective studies using different surgical techniques are needed to gain a better understanding of the effect of CST on VHRs.
In conclusion, although ACST increases postoperative wound complications, it is a safe, simple, and rapid option for patients with large and complicated VHs. We believe that it can maintain intraabdominal pressure, particularly by helping to close the abdomen without tension. With increasing experience, complication rates can be minimized. In addition, by improving QoL, the recurrence rate is similar to patients undergoing standard VHR.
References
1. Poulose BK, Shelton J, Phillips S, Moore D, Nealon W, Penson D, et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia. 2012; 16:179–183. PMID: 21904861.
2. Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M, et al. Criteria for definition of a complex abdominal wall hernia. Hernia. 2014; 18:7–17. PMID: 24150721.
3. Topcu R. Component separation technique in incisional hernias. Kafadar MT, Gok MA, editors. Hernia surgery. Akademisyen Kitabevi;2020. p. 159–179.
4. Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004; 240:578–585. PMID: 15383785.
5. den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias. Cochrane Database Syst Rev. 2008; 2008:CD006438. PMID: 18646155.
6. Booth JH, Garvey PB, Baumann DP, Selber JC, Nguyen AT, Clemens MW, et al. Primary fascial closure with mesh reinforcement is superior to bridged mesh repair for abdominal wall reconstruction. J Am Coll Surg. 2013; 217:999–1009. PMID: 24083910.
7. Holihan JL, Askenasy EP, Greenberg JA, Keith JN, Martindale RG, Roth JS, et al. Component separation vs. bridged repair for large ventral hernias: a multi-institutional risk-adjusted comparison, systematic review, and meta-analysis. Surg Infect (Larchmt). 2016; 17:17–26. PMID: 26375422.
8. Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990; 86:519–526. PMID: 2143588.
9. Cobb WS, Warren JA, Ewing JA, Burnikel A, Merchant M, Carbonell AM. Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. J Am Coll Surg. 2015; 220:606–613. PMID: 25797746.
10. Maloney SR, Schlosser KA, Prasad T, Kasten KR, Gersin KS, Colavita PD, et al. Twelve years of component separation technique in abdominal wall reconstruction. Surgery. 2019; 166:435–444. PMID: 31358348.
11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.
12. Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, et al. Carolinas Comfort Scale as a measure of hernia repair quality of life: a reappraisal utilizing 3788 international patients. Ann Surg. 2018; 267:171–176. PMID: 27655239.
13. Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW. Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg. 2008; 206:638–644. PMID: 18387468.
14. Cox TC, Huntington CR, Blair LJ, Prasad T, Lincourt AE, Heniford BT, et al. Predictive modeling for chronic pain after ventral hernia repair. Am J Surg. 2016; 212:501–510. PMID: 27443426.
15. Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF, et al. Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg. 2012; 256:714–723. PMID: 23095614.
16. Jensen KK, Arnesen RB, Christensen JK, Bisgaard T, Jørgensen LN. Large incisional hernias increase in size. J Surg Res. 2019; 244:160–165. PMID: 31295649.
17. Shestak KC, Edington HJ, Johnson RR. The separation of anatomic components technique for the reconstruction of massive midline abdominal wall defects: anatomy, surgical technique, applications, and limitations revisited. Plast Reconstr Surg. 2000; 105:731–738. PMID: 10697187.
18. Petersen S, Henke G, Zimmermann L, Aumann G, Hellmich G, Ludwig K. Ventral rectus fascia closure on top of mesh hernia repair in the sublay technique. Plast Reconstr Surg. 2004; 114:1754–1760. PMID: 15577345.
19. Clarke JM. Incisional hernia repair by fascial component separation: results in 128 cases and evolution of technique. Am J Surg. 2010; 200:2–8. PMID: 20637331.
20. Cornette B, De Bacquer D, Berrevoet F. Component separation technique for giant incisional hernia: a systematic review. Am J Surg. 2018; 215:719–726. PMID: 28811004.
21. Mazzocchi M, Dessy LA, Ranno R, Carlesimo B, Rubino C. “Component separation” technique and panniculectomy for repair of incisional hernia. Am J Surg. 2011; 201:776–783. PMID: 20850707.
22. Klima DA, Brintzenhoff RA, Tsirline VB, Belyansky I, Lincourt AE, Getz S, et al. Application of subcutaneous talc in hernia repair and wide subcutaneous dissection dramatically reduces seroma formation and postoperative wound complications. Am Surg. 2011; 77:888–894. PMID: 21944353.
23. Giurgius M, Bendure L, Davenport DL, Roth JS. The endoscopic component separation technique for hernia repair results in reduced morbidity compared to the open component separation technique. Hernia. 2012; 16:47–51. PMID: 21833851.
24. Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ. Posterior and open anterior components separations: a comparative analysis. Am J Surg. 2012; 203:318–322. PMID: 22244073.
25. Archer S, Pinto A, Vuik S, Bicknell C, Faiz O, Byrne B, et al. Surgery, complications, and quality of life: a longitudinal cohort study exploring the role of psychosocial factors. Ann Surg. 2019; 270:95–101. PMID: 29677027.
26. Blair LJ, Cox TC, Huntington CR, Groene SA, Prasad T, Lincourt AE, et al. The effect of component separation technique on quality of life (QOL) and surgical outcomes in complex open ventral hernia repair (OVHR). Surg Endosc. 2017; 31:3539–3546. PMID: 28039655.
27. Klima DA, Tsirline VB, Belyansky I, Dacey KT, Lincourt AE, Kercher KW, et al. Quality of life following component separation versus standard open ventral hernia repair for large hernias. Surg Innov. 2014; 21:147–154. PMID: 23843156.
28. Köckerling F. Recurrent incisional hernia repair: an overview. Front Surg. 2019; 6:26. PMID: 31139632.
29. Sailes FC, Walls J, Guelig D, Mirzabeigi M, Long WD, Crawford A, et al. Synthetic and biological mesh in component separation: a 10-year single institution review. Ann Plast Surg. 2010; 64:696–698. PMID: 20395790.
Fig. 1
(A) Anatomical location of vertical incision in anterior component separation technique. (B) Detachment of skin and subcutaneous tissues from underlying fascia. (C) The incision extending from the costal margin caudally to the pubis and laterally to the anterior axillary line and the iliac crest.
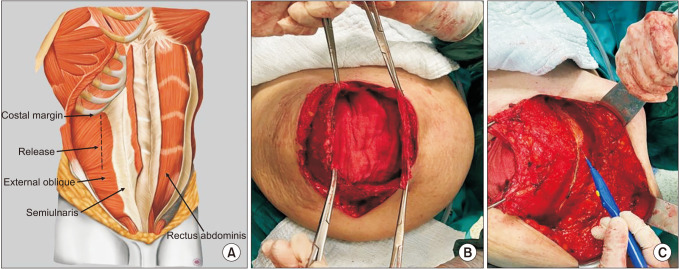
Fig. 2
Study flowchart. ACST, anterior component separation technique; CST, component separation technique.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download