INTRODUCTION
Neuroendocrine tumors (NETs) are commonly found in the gastrointestinal tract, with the small intestine traditionally being the most frequent site [
1]. However, recent years have seen a significant increase in the detection of rectal NETs (RNETs), now comparable in incidence to small intestine NETs. This surge is primarily attributed to advancements in endoscopic imaging and examination techniques, leading to the widespread use of colonoscopy for cancer screening [
2]. At diagnosis, approximately 90% of RNETs have a diameter of less than 10 mm and typically present as well-differentiated epithelial lesions confined to the submucosa without invasion into the muscularis propria. These small RNETs have a low risk of lymphovascular invasion (approximately 0.7%) and distant metastasis (less than 2%) [
34].
Consequently, the latest consensus recommends complete resection via advanced endoscopic methods as the optimal standard for managing RNETs smaller than 10 mm. Current guidelines support endoscopic resection as a safe and effective treatment for small RNETs; however, there remains debate over the optimal technique among various advanced endoscopic methods [
356]. Additionally, achieving complete R0 resection through additional treatment is advised when inadequate resections occur, as this is crucial for guiding further surveillance and treatment decisions. Nevertheless, the appropriate method for such salvage therapy has not yet been determined [
67].
Originally, the choice of endoscopic treatment depended on the tumor’s characteristics, such as size and morphology within the mucosal and submucosal layers. Standard polypectomy is not recommended due to a high risk of incomplete resection, which complicates the management of residual disease [
356789]. In cases where the mucosal and submucosal layers are damaged from previous procedures, the lifting process in EMR and ESD, which are common methods, can lead to complications or unsuccessful procedures. Despite these challenges, we devised a wide hot snare polypectomy (WHSP) as an effective and simple method for managing small residual RNETs. This technique is designed to achieve complete resection without additional devices or complex procedures. It involves securing an adequate margin around the lesion, including areas difficult to lift, and tightening towards the center. In this study, we confirmed that WHSP is a simple, safe, and effective salvage treatment method.
Go to :

METHODS
The study was reviewed and approved by the Institutional Review Board of Korea University Guro Hospital (No. 2023GR0268). This study was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
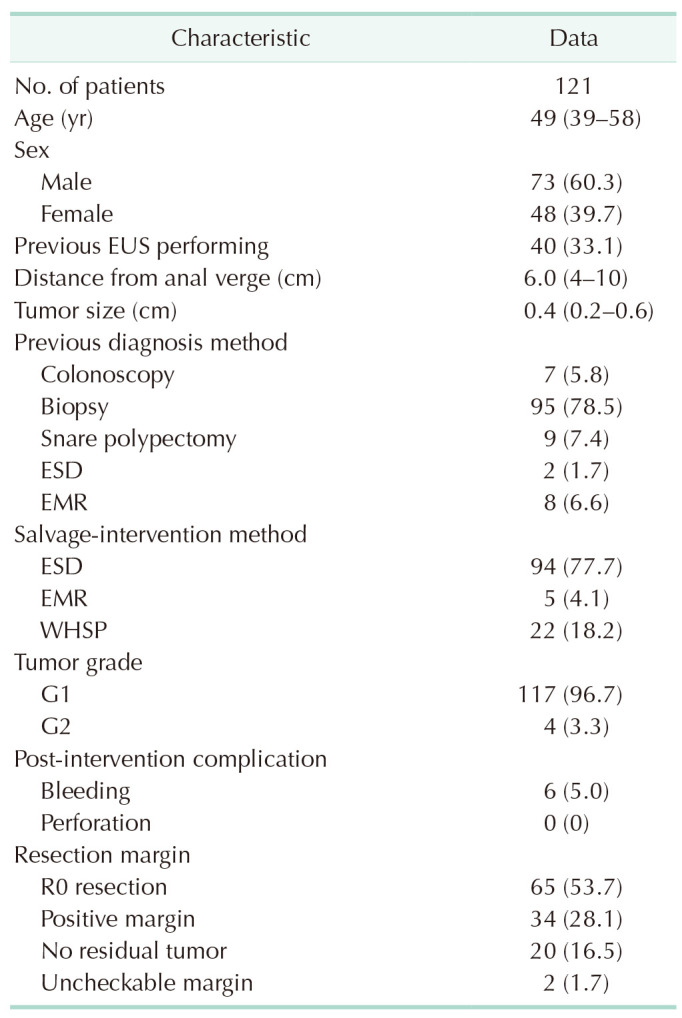
Study design and patients
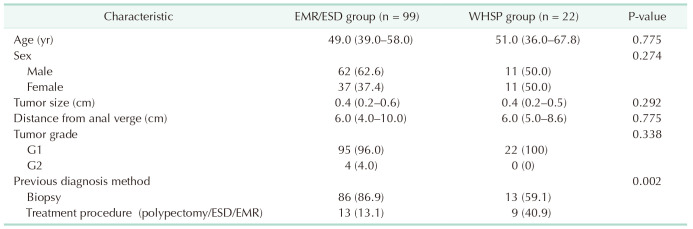
This retrospective cohort study was conducted at Korea University Guro Hospital between January 2018 and December 2022. It focused on patients diagnosed with RNETs who underwent salvage resection for tumors ≤10 mm in diameter. A total of 135 patients underwent salvage resections and, excluding the 14 who received transanal resection, 121 were included in the study. The study involved a comparative analysis of 2 groups based on the resection techniques used: endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) vs. WHSP. These patients were divided into 2 groups: the ESD/EMR group treated by several gastroenterologists specializing in endoscopy, and the WHSP group handled by a colorectal surgeon with endoscopic expertise.
Data extraction
Data on demographics, tumor characteristics, procedural details, and clinical outcomes were extracted retrospectively from electronic medical records. The inclusion criteria were patients treated or diagnosed for NETs ≤10 mm in size, confirmed pathologically. The exclusion criteria included patients with other malignant tumors, potential lymph node or distant metastasis, and those who underwent transanal resection to maintain consistency in comparing endoscopic outcomes.
Interventions
Endoscopic mucosal resection procedure
The procedure begins with the injection of a saline and indigocarmine dye solution into the submucosa directly beneath the lesion. This injection serves to elevate the lesion above the underlying muscle layer, creating a ‘safety cushion’ that helps prevent perforation during resection. After elevation, a circumferential incision is made around the lesion using a snare, which is then tightened to excise the lesion while cauterizing the blood vessels to minimize bleeding.
Endoscopic submucosal dissection procedure
Like EMR, ESD starts with the injection of a lifting solution to separate the lesion from the muscle layer. However, ESD involves a more intricate procedure where a specialized ESD knife (e.g., DualKnife or ITknife, Olympus Corp.) is used to make a precise circumferential cut around the lesion. Following this marking, meticulous dissection is performed layer by layer in the submucosal space to ensure complete en bloc resection of the lesion.
Both EMR and ESD were adapted by several gastroenterologists to match their personal preferences and the specific needs of the patients. Customizations included the use of various additional tools, such as caps or specialized knives, which facilitated the procedures by providing enhanced control and precision.
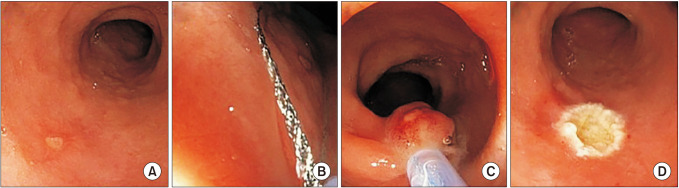
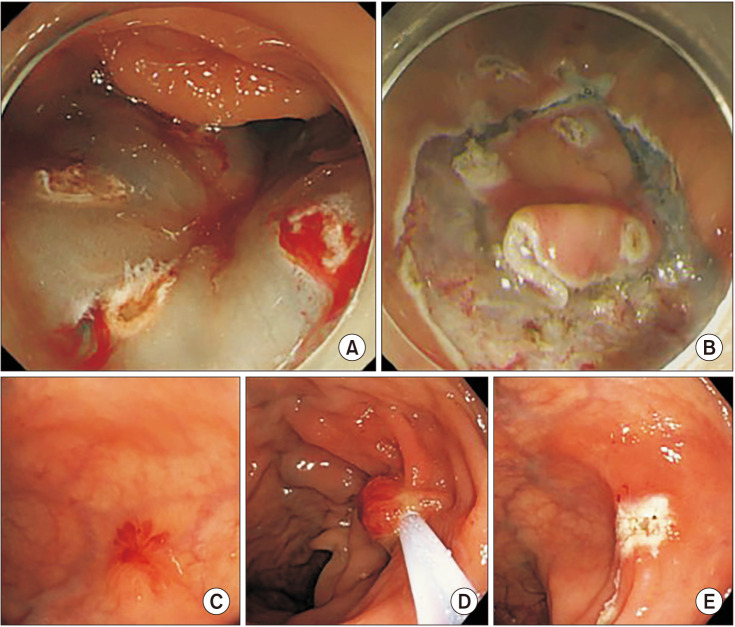
Wide hot snare polypectomy
In the WHSP procedure, we used the cBM1523024-R(42) snare from BMA, which features a 15 mm diameter when fully expanded. To ensure an R0 resection—defined as the absence of tumor cells within at least 1 mm of the margins—we meticulously placed the snare to achieve a visual margin of 2–5 mm, and up to 10 mm at maximum, around the lesion's perimeter. This careful placement is crucial to encompass all microscopic extensions and guarantee complete tumor removal.
The WHSP procedures were performed by a single endoscopic specialist, who is also a colorectal surgeon, ensuring uniform application of the technique. Once the snare was positioned, it was tightened to compress the surrounding tissue, which not only facilitated a lifting effect due to the margins being pushed upwards but also enhanced the precision of the resection. Before applying the electric current, the entire tissue was lifted with the snare to assess the depth, ensuring a safe and effective procedure. Subsequently, an electric current was applied through the snare wire to simultaneously cut and coagulate the tissue, minimizing bleeding and ensuring thorough tumor excision. This technique not only provided a clear path for resection but also maintained the integrity of the margins both visually and pathologically, confirming the achievement of an R0 resection status. No additional instruments such as caps or knives were used, to simplify the procedure (
Fig. 1).
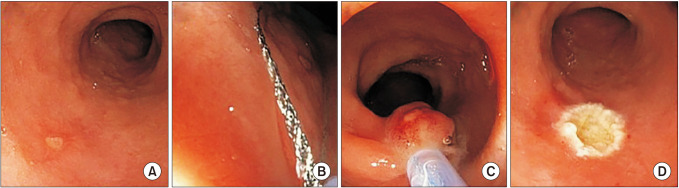 | Fig. 1Wide hot snare polypectomy for the post-endoscopic mucosal resection (EMR) state of the rectal neuroendocrine tumor with improper margin. (A) The previous EMR scar is at the distal rectum. (B) Applying the snare with a sufficiently visible margin. (C) The compressed and lifted tissue was cut with electrocautery. (D) The absence of complications and sufficient margins were confirmed.
|
Outcomes
Efficacy of the procedure was primarily evaluated by the rate of complete resection and the time taken to perform the procedure, while safety was assessed through the incidence of post-procedure complications. Complete resection was defined as the absence of tumor cells at both lateral and vertical margins, confirmed pathologically. Procedure time included the durations from lesion identification to the initiation of the procedure, and from the completion of resection to the final assessment by the surgical team. All resected specimens were rigorously examined by pathologists to ensure comprehensive evaluation.
Statistical analysis
Continuous variables, such as procedure time and patient age, were analyzed using the Student t-test and expressed as means ± standard deviations or medians with interquartile ranges (IQRs), depending on the data distribution. Categorical variables, including resection status (complete or incomplete) and incidence of complications, were assessed with the chi-square test or Fisher exact test, presented as frequencies and percentages. All statistical tests were 2-sided, and a P-value of less than 0.05 was considered to indicate statistical significance. Analyses were performed using IBM SPSS Statistics ver. 20.0.0 (IBM Corp.).
Go to :

DISCUSSION
Although RNETs are relatively uncommon, their incidence has increased due to the widespread use of screening colonoscopy and advancements in endoscopic technology [
1]. Most RNETs are detected at stage 1 or 2, with excellent long-term prognosis and 5-year survival rates between 74% and 88% [
11011]. Typically, 80% to 90% of these tumors are less than 1 cm in size, low grade, rarely metastasize (<3%), and are diagnosed early in a well-differentiated state confined to the submucosa [
412]. Current guidelines from the European Neuroendocrine Tumor Society recommend endoscopic resection for well-differentiated tumors smaller than 10 mm due to their minimal risk of lymphatic and vascular invasion [
61314].
Various treatment strategies for the endoscopic resection of RNETs include standard snare polypectomy, EMR, EMR band ligation, EMR cap placement, underwater EMR, EMR ligation, ESD, ESD muscle ligation, and endoscopic full-thickness resection. Although complete resection rates for these techniques are reported to be between 88% and 100%, the optimal treatment method is still a subject of debate [
678151617].
Endoscopic resection of RNETs aims for
en bloc and complete resection. If an R1 lesion is identified after endoscopic resection and confirmed to be G1 with no risk factors, lymphatic, or vascular invasion, a second endoscopic resection can be conducted without additional imaging tests. Achieving an R0 resection status in this subsequent procedure may eliminate the need for further follow-up. Therefore, salvage procedures are crucial to ensure complete lesion removal and achieve optimal patient outcomes [
67].
When RNET was considered a polyp before the endoscopic procedure, the complete resection rate was 68.2%. However, when RNET was diagnosed or suspected, it increased to 94.5% [
51819]. If an initial endoscopic procedure results in incomplete resection, subsequent observations often reveal scarring, ulceration, and deformation of the dissection surface at the lesion site during the second endoscopy. These conditions complicate the lifting and dissection processes, thereby hindering the salvage resection of the residual tumor.
Moreover, the choice of optimal treatment, even for salvage procedures, remains a subject of clinical debate [
513]. Traditional endoscopic polypectomy is not typically recommended for RNET resections because it usually does not achieve adequate and complete lesion removal and may necessitate additional interventions [
61320]. Anatomical alterations caused by previous interventions can complicate the use of lifting techniques or other adjunctive methods and potentially lead to additional complications.
These challenges have led to a paradigm shift and the development of a simplified, single-step WHSP technique. By enhancing the existing polypectomy methods, we anticipate that the procedure can be performed more efficiently and safely, without the need for complex additional steps that increase the risk of complications. This innovative approach integrates the damaged layers into a single, streamlined procedure, which is expected to enhance both efficiency and safety while reducing the likelihood of complications. Therefore, we applied the WHSP technique to salvage procedures for small, early-stage RNETs.
The WHSP procedure involves placing a guidewire widely around the lesion to secure sufficient margins and then tightening it while pushing toward the lesion. This allows for resection with a similar effect to the lifting process without the invasive lifting procedure. The principle of lifting is similar to that of underwater EMR, but it offers the advantage of achieving similar effects without the cumbersome process of water infusion [
9].
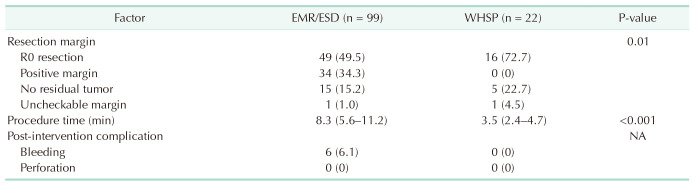
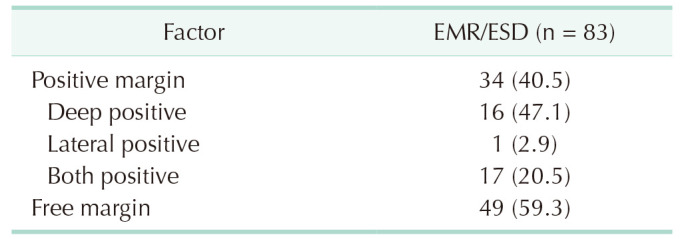
The R0 resection rate was 72.7%, which was significantly higher than the 49.5% in the EMR/ESD group. In reality, excluding no residual tumor and uncheckable margin, the positive margin was 0%. Additionally, the average procedure time was 3.5 minutes, which was significantly shorter than 8.3 minutes, and no complications were observed after the procedure. This result proved that sufficient treatment can be achieved with WHSP. This is a procedure that can be performed by any endoscopist skilled in polypectomy and does not require special skills or special equipment.
Our study has several limitations. Firstly, the small number of patients in this study is attributed to the rarity of RNETs. Additionally, being a retrospective study conducted at a single institution, there is a possibility of selection bias. Secondly, the outcomes for the EMR/ESD group were lower compared to other studies. The EMR/ESD procedures require a lifting process through injection, which can be problematic in salvage operations where the submucosal layers have already been compromised by the initial procedures, increasing the likelihood of difficulties or failures in progressing through each step. Moreover, the inconsistent results can be attributed to the variety of techniques and the different endoscopists performing the EMR/ESD procedures. Despite these limitations, the significance of our study lies not in demonstrating the inadequacy of EMR/ESD, but in showing that a polypectomy-based technique, which is generally not recommended for RNET resection, can still yield good outcomes. This finding highlights the potential of the refined polypectomy technique, WHSP, to achieve effective results even in challenging cases.
Based on the results of this study, WHSP is not limited to RNETs and can potentially be extended to other small tumors. For general small rectal polyps, using WHSP instead of simple polypectomy may reduce the need for repeated salvage procedures following subsequent histopathological evaluations. Small lesions, particularly those less than 10 mm in size, are suitable candidates for WHSP. Additionally, WHSP can be considered in anatomically challenging cases where endoscopic access is difficult and performing complex procedures is challenging. Overall, WHSP holds promise for a variety of applications, including removing residual tumors following initial endoscopic resection. This technique is expected to extend its applicability beyond RNETs and be useful in the treatment of various lesions.
In conclusion, our study demonstrates that WHSP as part of salvage treatment is a swift, uncomplicated, secure, and efficient choice for rectal NETs <10 mm in the absence of risk factors. The procedure’s simplicity, requiring no additional steps or instruments, is a significant advantage, making WHSP a potential therapeutic alternative for other small tumors as well.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download