1. Miller CE, Vasan RS. The southern rural health and mortality penalty: a review of regional health inequities in the United States. Soc Sci Med. 2021; 268:113443. PMID:
33137680.

2. Cosby AG, McDoom-Echebiri MM, James W, Khandekar H, Brown W, Hanna HL. Growth and persistence of place-based mortality in the United States: the rural mortality penalty. Am J Public Health. 2019; 109:155–162. PMID:
30496008.

3. Ebeling M, Rau R, Sander N, Kibele E, Klüsener S. Urban-rural disparities in old-age mortality vary systematically with age: evidence from Germany and England & Wales. Public Health. 2022; 205:102–109. PMID:
35276525.
4. Kim YE, Jung YS, Ock M, Park H, Kim KB, Go DS, Yoon SJ. The gaps in health-adjusted life years (HALE) by income and region in Korea: a national representative bigdata analysis. Int J Environ Res Public Health. 2021; 18:3473. PMID:
33801588.

5. Kim I. Contributions of the life expectancy gap reduction between urban and rural areas to the increase in overall life expectancy in South Korea from 2000 to 2019. Int J Equity Health. 2023; 22:141. PMID:
37507677.

6. Choi MH, Moon MH, Yoon TH. Avoidable mortality between metropolitan and non-metropolitan areas in Korea from 1995 to 2019: a descriptive study of implications for the national healthcare policy. Int J Environ Res Public Health. 2022; 19:3475. PMID:
35329162.

7. Chung SJ, Han YS, Lee SI, Kang SH. Urban and rural differences in the prevalence of gender and age specific obesity and related health behaviors in Korea. J Korean Med Sci. 2005; 20:713–720. PMID:
16224141.

8. Ha K, Song Y, Kim HK. Regional disparities in the associations of cardiometabolic risk factors and healthy dietary factors in Korean adults. Nutr Res Pract. 2020; 14:519–531. PMID:
33029291.
9. Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, Cunningham TJ, Khan LK, Caraballo RS, Holt JB, et al. Health-related behaviors by urban-rural county classification—United States, 2013. MMWR Surveill Summ. 2017; 66:1–8.

10. Cohen SA, Greaney ML, Sabik NJ. Assessment of dietary patterns, physical activity and obesity from a national survey: rural-urban health disparities in older adults. PLoS One. 2018; 13:e0208268. PMID:
30517166.

11. Foster HME, Polz P, Gill JMR, Celis-Morales C, Mair FS, O’Donnell CA. The influence of socioeconomic status on the association between unhealthy lifestyle factors and adverse health outcomes: a systematic review. Wellcome Open Res. 2023; 8:55. PMID:
38533439.

12. Soares RR. On the determinants of mortality reductions in the developing world. Popul Dev Rev. 2007; 33:247–287.

13. Chang I, Kim BH. Regional disparity of medical resources and its effect on age-standardized mortality rates in Korea. Ann Reg Sci. 2019; 62:305–325.
14. Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med. 2012; 55:163–170. PMID:
22735042.

15. Zhang YB, Pan XF, Chen J, Cao A, Xia L, Zhang Y, Wang J, Li H, Liu G, Pan A. Combined lifestyle factors, all-cause mortality and cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. J Epidemiol Community Health. 2021; 75:92–99. PMID:
32892156.

16. Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, Song M, Liu G, Shin HJ, Sun Q, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ. 2020; 368:l6669. PMID:
31915124.

17. Sabia S, Singh-Manoux A, Hagger-Johnson G, Cambois E, Brunner EJ, Kivimaki M. Influence of individual and combined healthy behaviours on successful aging. CMAJ. 2012; 184:1985–1992. PMID:
23091184.

18. Said MA, Verweij N, van der Harst P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank Study. JAMA Cardiol. 2018; 3:693–702. PMID:
29955826.
19. Meader N, King K, Moe-Byrne T, Wright K, Graham H, Petticrew M, Power C, White M, Sowden AJ. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health. 2016; 16:657. PMID:
27473458.

20. Noble N, Paul C, Turon H, Oldmeadow C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev Med. 2015; 81:16–41. PMID:
26190368.

21. Kim HR. Quality of diet and nutritional intake and mortality risk among South Korean adults based on 12-year follow-up data. Korean J Community Nutr. 2016; 21:354–365.

22. Lim J, Lee Y, Shin S, Lee HW, Kim CE, Lee JK, Lee SA, Kang D. An association between diet quality index for Koreans (DQI-K) and total mortality in Health Examinees Gem (HEXA-G) study. Nutr Res Pract. 2018; 12:258–264. PMID:
29854332.

23. Jo G, Park D, Lee J, Kim R, Subramanian SV, Oh H, Shin MJ. Trends in diet quality and cardiometabolic risk factors among Korean adults, 2007-2018. JAMA Netw Open. 2022; 5:e2218297. PMID:
35731513.
24. Yun JE, Won S, Kimm H, Jee SH. Effects of a combined lifestyle score on 10-year mortality in Korean men and women: a prospective cohort study. BMC Public Health. 2012; 12:673. PMID:
22900981.

25. Kim JY, Ko YJ, Rhee CW, Park BJ, Kim DH, Bae JM, Shin MH, Lee MS, Li ZM, Ahn YO. Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: the Seoul male cohort study. J Prev Med Public Health. 2013; 46:319–328. PMID:
24349653.

26. Lee DH, Nam JY, Kwon S, Keum N, Lee JT, Shin MJ, Oh H. Lifestyle risk score and mortality in Korean adults: a population-based cohort study. Sci Rep. 2020; 10:10260. PMID:
32581249.

28. Jeon BY, Choi SM, Kim CY. Socioeconomic equity in regional distribution of health care resources in Korea. Health Policy Manag. 2012; 22:85–108.

29. Kim H, Ahn S, Ulfarsson GF. Impacts of transportation and industrial complexes on establishment-level productivity growth in Korea. Transp Policy. 2021; 100:89–97.
30. Song YJ. The South Korean health care system. Japan Med Assoc J. 2009; 52:206–209.
31. Lee SE, Yeon M, Kim CW, Yoon TH. The association among individual and contextual factors and unmet healthcare needs in South Korea: a multilevel study using national data. J Prev Med Public Health. 2016; 49:308–322. PMID:
27744672.

32. Lim JH. Regional disparity and factors influencing unmet medical needs: a study based on the Sixth Korea National Health and Nutrition Examination Survey (2015). Osong Public Health Res Perspect. 2017; 8:295–301. PMID:
29164040.

33. Oh Y. The National Health Plan 2030: its purpose and directions of development. J Prev Med Public Health. 2021; 54:173–181. PMID:
34092063.

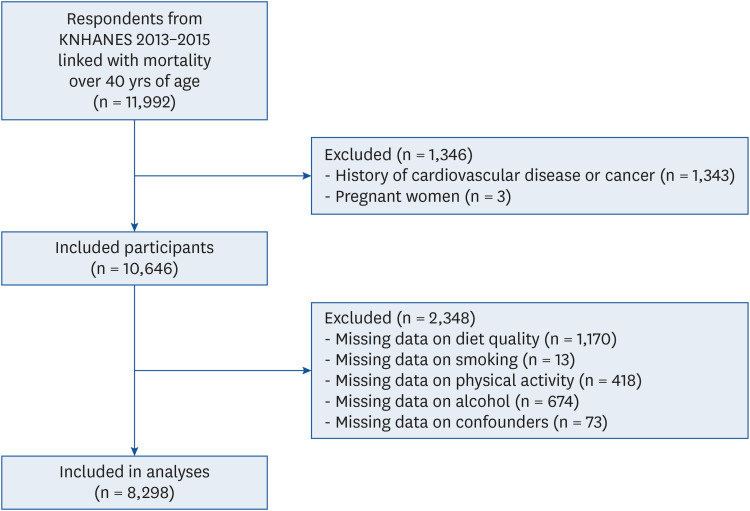
34. Yun S, Oh K. The Korea National Health and Nutrition Examination Survey data linked cause of death data. Epidemiol Health. 2022; 44:e2022021. PMID:
35167742.
35. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77. PMID:
24585853.

37. Norheim OF, Jha P, Admasu K, Godal T, Hum RJ, Kruk ME, Gómez-Dantés O, Mathers CD, Pan H, Sepúlveda J, et al. Avoiding 40% of the premature deaths in each country, 2010-30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet. 2015; 385:239–252. PMID:
25242039.

38. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020; 396:1223–1249. PMID:
33069327.
39. Rural Development Administration, National Institute of Agricultural Sciences. Korean Food Composition Table. 8th rev. Wanju: National Institute of Agricultural Sciences;2013.
40. Ministry of Health and Welfare. The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2015. Sejong: Ministry of Health and Welfare;2015.
41. Yun S, Park S, Yook SM, Kim K, Shim JE, Hwang JY, Oh K. Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2022; 16:233–247. PMID:
35392533.

42. Yook SM, Park S, Moon HK, Kim K, Shim JE, Hwang JY. Development of Korean Healthy Eating Index for adults using the Korea National Health and Nutrition Examination Survey data. J Nutr Health. 2015; 48:419–428.

43. English LK, Ard JD, Bailey RL, Bates M, Bazzano LA, Boushey CJ, Brown C, Butera G, Callahan EH, de Jesus J, et al. Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open. 2021; 4:e2122277. PMID:
34463743.
44. Kim S, Lee GW, Park CY. Older Korean men with inadequate vitamin D status have lower odds of radiologic osteoarthritis. Sci Rep. 2022; 12:11372. PMID:
35790839.

45. Kim H. Interlinking open government data in Korea using administrative district knowledge graph. J Inf Sci Theory Pract. 2018; 6:18–30.
46. Local Autonomy Act of 2023. c. 3. Sejong: Ministry of Security and Public Administration;2023.
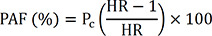
47. Miettinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol. 1974; 99:325–332. PMID:
4825599.

48. Khosravi A, Nazemipour M, Shinozaki T, Mansournia MA. Population attributable fraction in textbooks: time to revise. Glob Epidemiol. 2021; 3:100062. PMID:
37635714.

49. Natarajan S, Lipsitz SR, Rimm E. A simple method of determining confidence intervals for population attributable risk from complex surveys. Stat Med. 2007; 26:3229–3239. PMID:
17309113.
50. Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012; 41:514–520. PMID:
22253321.

51. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007; 147:W163–W194. PMID:
17938389.
52. Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005; 20:575–579. PMID:
16119429.

53. Korea National Health and Nutrition Examination Survey Analytic Guidelines Using SAS Program. Cheongju: Korea Centers for Disease Control and Prevention;2019.
54. Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004; 292:1433–1439. PMID:
15383513.

55. Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC, et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation. 2018; 138:345–355. PMID:
29712712.
56. Zhang QL, Zhao LG, Zhang W, Li HL, Gao J, Han LH, Zheng W, Shu XO, Xiang YB. Combined impact of known lifestyle factors on total and cause-specific mortality among Chinese men: a prospective cohort study. Sci Rep. 2017; 7:5293. PMID:
28706246.

57. Ford ES, Zhao G, Tsai J, Li C. Low-risk lifestyle behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health. 2011; 101:1922–1929. PMID:
21852630.

58. Imamura F, Micha R, Khatibzadeh S, Fahimi S, Shi P, Powles J, Mozaffarian D. Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE). Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob Health. 2015; 3:e132–e142. PMID:
25701991.

59. Wang DD, Li Y, Afshin A, Springmann M, Mozaffarian D, Stampfer MJ, Hu FB, Murray CJ, Willett WC. Global improvement in dietary quality could lead to substantial reduction in premature death. J Nutr. 2019; 149:1065–1074. PMID:
31049577.

60. Stephenson BJ, Willett WC. Racial and ethnic heterogeneity in diets of low-income adult females in the United States: results from National Health and Nutrition Examination Surveys from 2011 to 2018. Am J Clin Nutr. 2023; 117:625–634. PMID:
36872021.
61. Kim HJ, Kim K. Effect of geographic area on dietary quality across different age groups in Korea. Korean J Community Nutr. 2019; 24:453–464.

62. Park S, Kim HJ, Kim K. Do where the elderly live matter? Factors associated with diet quality among Korean elderly population living in urban versus rural areas. Nutrients. 2020; 12:1314. PMID:
32380737.

63. Seidelmann SB, Claggett B, Cheng S, Henglin M, Shah A, Steffen LM, Folsom AR, Rimm EB, Willett WC, Solomon SD. Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health. 2018; 3:e419–e428. PMID:
30122560.

64. Sun Y, Rong S, Liu B, Du Y, Wu Y, Chen L, Xiao Q, Snetselaar L, Wallace R, Bao W. Meal skipping and shorter meal intervals are associated with increased risk of all-cause and cardiovascular disease mortality among US adults. J Acad Nutr Diet. 2023; 123:417–426.e3. PMID:
35964910.
65. Ko H. The effect of outdoor smoking ban: evidence from Korea. Health Econ. 2020; 29:278–293. PMID:
31860782.
66. National Health Promotion Act of 2021. c. 9. Sejong: Ministry of Health and Welfare;2021.
67. Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol. 2011; 40:1382–1400. PMID:
22039197.

68. Kim J. Association between meeting physical activity guidelines and mortality in Korean adults: an 8-year prospective study. J Exerc Nutrition Biochem. 2017; 21:23–29.

69. Soedamah-Muthu SS, De Neve M, Shelton NJ, Tielemans SM, Stamatakis E. Joint associations of alcohol consumption and physical activity with all-cause and cardiovascular mortality. Am J Cardiol. 2013; 112:380–386. PMID:
23647792.

70. O’Donovan G, Hamer M, Stamatakis E. Relationships between exercise, smoking habit and mortality in more than 100,000 adults. Int J Cancer. 2017; 140:1819–1827. PMID:
28108995.

71. Hershey MS, Martínez-González MÁ, Álvarez-Álvarez I, Martínez Hernández JA, Ruiz-Canela M. The Mediterranean diet and physical activity: better together than apart for the prevention of premature mortality. Br J Nutr. 2022; 128:1413–1424. PMID:
34462020.
72. Pardavila-Belio MI, de la O V, Hershey MS, Barbería-Latasa M, Toledo E, Martin-Moreno JM, Martínez-González MÁ, Ruiz-Canela M. Joint association of the Mediterranean diet and smoking with all-cause mortality in the Seguimiento Universidad de Navarra (SUN) cohort. Nutrition. 2022; 103-104:111761. PMID:
35843044.

73. Stringhini S, Sabia S, Shipley M, Brunner E, Nabi H, Kivimaki M, Singh-Manoux A. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010; 303:1159–1166. PMID:
20332401.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download