1. Martínez-Vizcaíno V, Álvarez-Bueno C, Cavero-Redondo I. Diet in the management of weight loss. Nutrients. 2021; 13:1306. PMID:
33920924.

2. Diamantis DV, Karatzi K, Kantaras P, Liatis S, Iotova V, Bazdraska Y, Tankova T, Cardon G, Wikström K, Rurik I, et al. Prevalence and socioeconomic correlates of adult obesity in Europe: the Feel4Diabetes study. Int J Environ Res Public Health. 2022; 19:12572. PMID:
36231871.
3. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024; 403:1027–1050. PMID:
38432237.
4. Vandevijvere S, De Pauw R, Djojosoeparto S, Gorasso V, Guariguata L, Løvhaug AL, Mialon M, Van Dam I, von Philipsborn P. Upstream determinants of overweight and obesity in Europe. Curr Obes Rep. 2023; 12:417–428. PMID:
37594616.

5. Zhu J, Zhang Y, Wu Y, Xiang Y, Tong X, Yu Y, Qiu Y, Cui S, Zhao Q, Wang N, et al. Obesity and dyslipidemia in chinese adults: a cross-sectional study in Shanghai, China. Nutrients. 2022; 14:2321. PMID:
35684121.

6. Sun X, Yan AF, Shi Z, Zhao B, Yan N, Li K, Gao L, Xue H, Peng W, Cheskin LJ, et al. Health consequences of obesity and projected future obesity health burden in China. Obesity (Silver Spring). 2022; 30:1724–1751. PMID:
36000246.

7. Reid TJ, Korner J. Medical and surgical treatment of obesity. Med Clin North Am. 2022; 106:837–852. PMID:
36154703.

8. Müller TD, Blüher M, Tschöp MH, DiMarchi RD. Anti-obesity drug discovery: advances and challenges. Nat Rev Drug Discov. 2022; 21:201–223. PMID:
34815532.
9. Perdomo CM, Cohen RV, Sumithran P, Clément K, Frühbeck G. Contemporary medical, device, and surgical therapies for obesity in adults. Lancet. 2023; 401:1116–1130. PMID:
36774932.

10. Fink J, Seifert G, Blüher M, Fichtner-Feigl S, Marjanovic G. Obesity surgery. Dtsch Arztebl Int. 2022; 119:70–80. PMID:
34819222.
11. Zhu Q, An YA, Scherer PE. Mitochondrial regulation and white adipose tissue homeostasis. Trends Cell Biol. 2022; 32:351–364. PMID:
34810062.

12. Li Y, Fromme T. Uncoupling protein 1 does not produce heat without activation. Int J Mol Sci. 2022; 23:2406. PMID:
35269549.

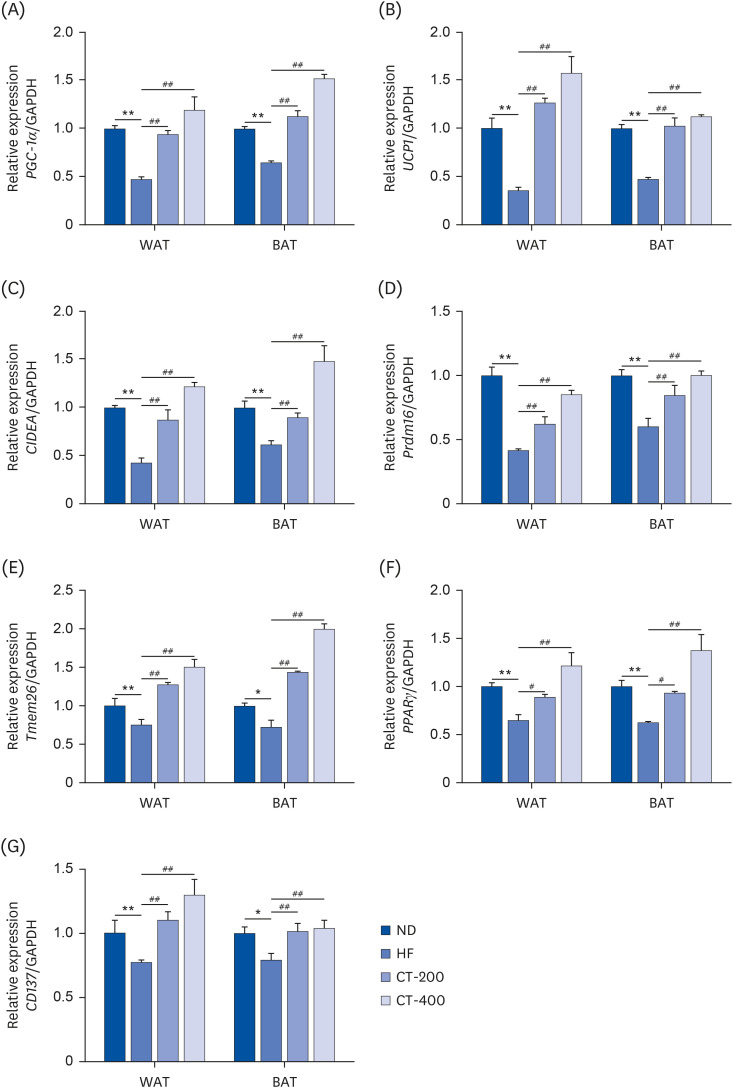
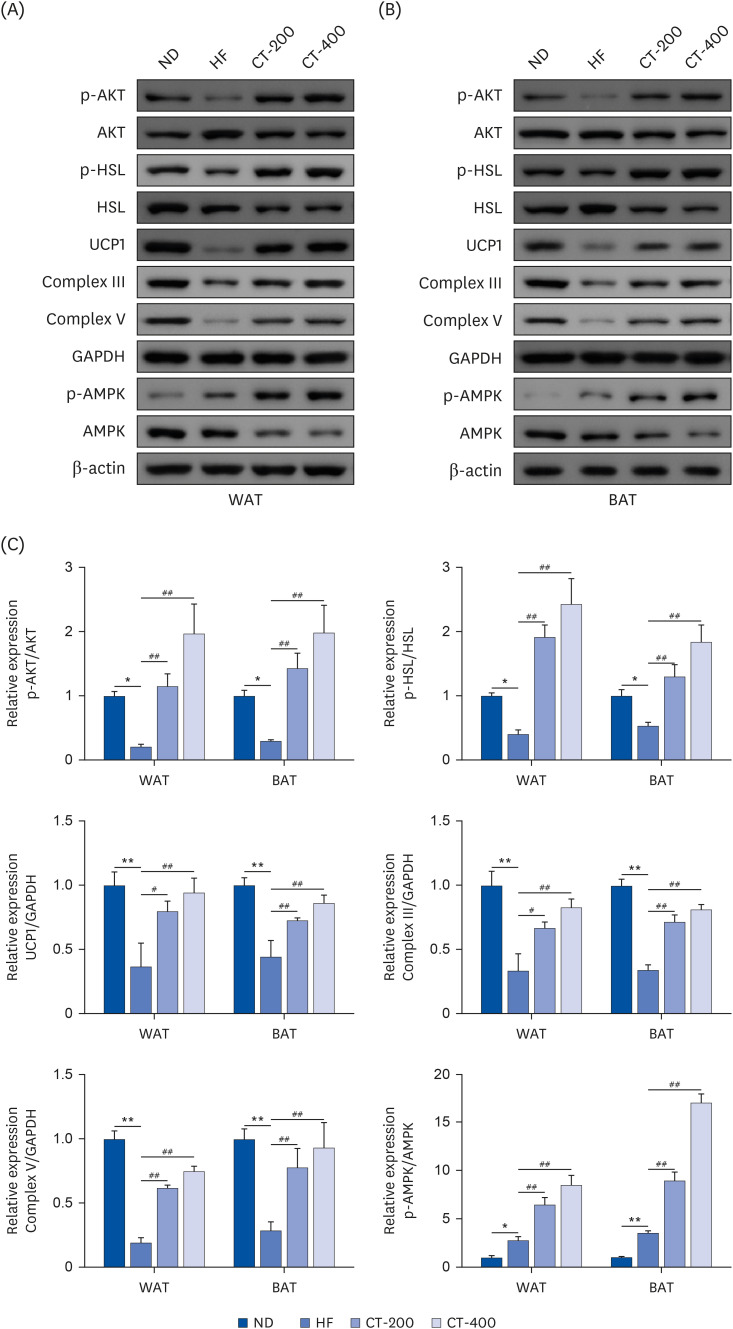
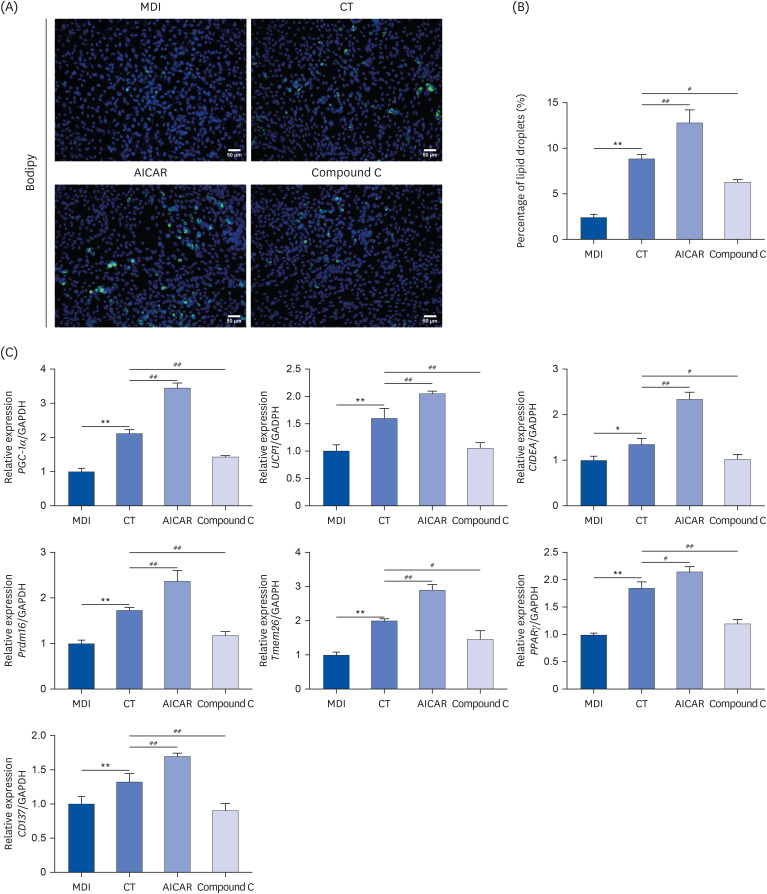
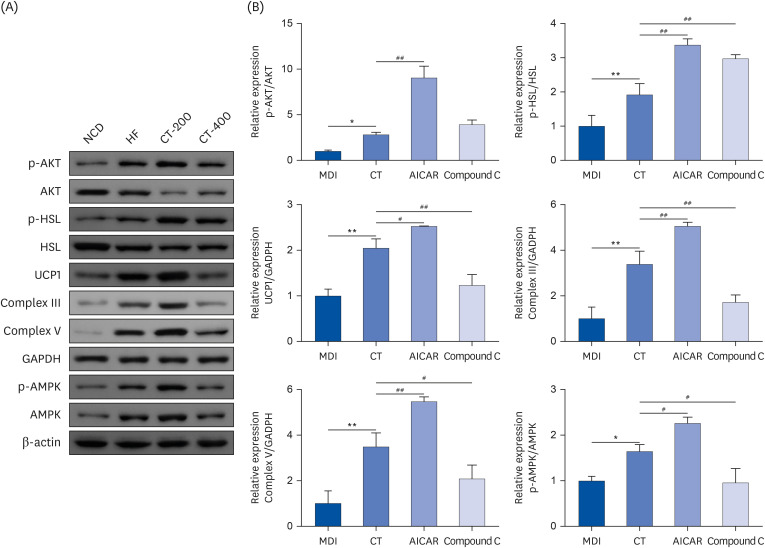
13. Crichton PG, Lee Y, Kunji ER. The molecular features of uncoupling protein 1 support a conventional mitochondrial carrier-like mechanism. Biochimie. 2017; 134:35–50. PMID:
28057583.
14. Scheele C, Wolfrum C. Brown adipose crosstalk in tissue plasticity and human metabolism. Endocr Rev. 2020; 41:53–65. PMID:
31638161.

15. Zhang F, Ma T, Tong X, Liu Y, Cui P, Xu X, Shi J, Hu W, Lu W, Pei Z, et al. Electroacupuncture improves metabolic and ovarian function in a rat model of polycystic ovary syndrome by decreasing white adipose tissue, increasing brown adipose tissue, and modulating the gut microbiota. Acupunct Med. 2022; 40:347–359. PMID:
34892981.

16. Cheng L, Wang J, Dai H, Duan Y, An Y, Shi L, Lv Y, Li H, Wang C, Ma Q, et al. Brown and beige adipose tissue: a novel therapeutic strategy for obesity and type 2 diabetes mellitus. Adipocyte. 2021; 10:48–65. PMID:
33403891.

17. Saikia R, Joseph J. AMPK: a key regulator of energy stress and calcium-induced autophagy. J Mol Med (Berl). 2021; 99:1539–1551. PMID:
34398293.

18. Steinberg GR, Hardie DG. New insights into activation and function of the AMPK. Nat Rev Mol Cell Biol. 2023; 24:255–272. PMID:
36316383.
19. Desjardins EM, Steinberg GR. Emerging role of AMPK in brown and beige adipose tissue (BAT): implications for obesity, insulin resistance, and type 2 diabetes. Curr Diab Rep. 2018; 18:80. PMID:
30120579.

20. Szewczuk M, Boguszewska K, Kaźmierczak-Barańska J, Karwowski BT. The role of AMPK in metabolism and its influence on DNA damage repair. Mol Biol Rep. 2020; 47:9075–9086. PMID:
33070285.

21. Wu YH, Wu YR, Li B, Yan ZY. Cryptotanshinone: a review of its pharmacology activities and molecular mechanisms. Fitoterapia. 2020; 145:104633. PMID:
32445662.

22. Wang L, Wang R, Wei GY, Zhang RP, Zhu Y, Wang Z, Wang SM, Du GH. Cryptotanshinone alleviates chemotherapy-induced colitis in mice with colon cancer via regulating fecal-bacteria-related lipid metabolism. Pharmacol Res. 2021; 163:105232. PMID:
33027716.

23. Terado T, Kim CJ, Ushio A, Minami K, Tambe Y, Kageyama S, Kawauchi A, Tsunoda T, Shirasawa S, Tanaka H, et al. Cryptotanshinone suppresses tumorigenesis by inhibiting lipogenesis and promoting reactive oxygen species production in KRAS-activated pancreatic cancer cells. Int J Oncol. 2022; 61:108. PMID:
35894141.
24. Imran KM, Rahman N, Yoon D, Jeon M, Lee BT, Kim YS. Cryptotanshinone promotes commitment to the brown adipocyte lineage and mitochondrial biogenesis in C3H10T1/2 mesenchymal stem cells via AMPK and p38-MAPK signaling. Biochim Biophys Acta BBAMol Cell Biol Lipids. 2017; 1862:1110–1120.

25. Yang W, Han J, Gong S, Zhao J, Yu T, Ma J. Cryptotanshinone suppressed postmenopausal osteoporosis by preventing RANKL-mediated osteoclastogenesis against kidney injury. Evid Based Complement Alternat Med. 2022; 2022:2821984. PMID:
35132325.

26. Wang N. Effect of cryptotanshinone on glucose and lipid metabolism and sex hormone levels of rats with polycystic ovary syndrome. Matern Child Health Care China. 2015; 30:3490–3493.
27. Ling J, Hua L, Qin Y, Gu T, Jiang S, Zhao J. Perfluorooctane sulfonate promotes hepatic lipid accumulation and steatosis in high-fat diet mice through AMP-activated protein kinase/acetyl-CoA carboxylase (AMPK/ACC) pathway. J Appl Toxicol. 2023; 43:312–322. PMID:
35999056.

28. Villarroya F, Cereijo R, Gavaldà-Navarro A, Villarroya J, Giralt M. Inflammation of brown/beige adipose tissues in obesity and metabolic disease. J Intern Med. 2018; 284:492–504. PMID:
29923291.
29. Carpi S, Quarta S, Doccini S, Saviano A, Marigliano N, Polini B, Massaro M, Carluccio MA, Calabriso N, Wabitsch M, et al. Tanshinone IIA and Cryptotanshinone counteract inflammation by regulating gene and miRNA expression in human SGBS adipocytes. Biomolecules. 2023; 13:1029. PMID:
37509065.

30. Song M, Chen L, Zhang L, Li C, Coffie JW, Fang Z, Zhang L, Wang S, Gao X, Wang H. Cryptotanshinone enhances wound healing in type 2 diabetes with modulatory effects on inflammation, angiogenesis and extracellular matrix remodelling. Pharm Biol. 2020; 58:845–853. PMID:
32870741.

31. Tang H, Zeng Q, Tang T, Wei Y, Pu P. Kaempferide improves glycolipid metabolism disorder by activating PPARγ in high-fat-diet-fed mice. Life Sci. 2021; 270:119133. PMID:
33508298.

32. Zhang S, Li J, Shi X, Tan X, Si Q. Naringenin activates beige adipocyte browning in high fat diet-fed C57BL/6 mice by shaping the gut microbiota. Food Funct. 2022; 13:9918–9930. PMID:
36053256.

33. Wang X, Morris-Natschke SL, Lee KH. New developments in the chemistry and biology of the bioactive constituents of Tanshen. Med Res Rev. 2007; 27:133–148. PMID:
16888751.
34. Deng X, Huang SL, Ren J, Pan ZH, Shen Y, Zhou HF, Zuo ZL, Leng Y, Zhao QS. Development and structure-activity relationships of tanshinones as selective 11β-hydroxysteroid dehydrogenase 1 inhibitors. Nat Prod Bioprospect. 2022; 12:36. PMID:
36131216.

35. Wang Q, Li H, Tajima K, Verkerke AR, Taxin ZH, Hou Z, Cole JB, Li F, Wong J, Abe I, et al. Post-translational control of beige fat biogenesis by PRDM16 stabilization. Nature. 2022; 609:151–158. PMID:
35978186.

36. Chouchani ET, Kazak L, Spiegelman BM. New advances in adaptive thermogenesis: UCP1 and beyond. Cell Metab. 2019; 29:27–37. PMID:
30503034.

37. van der Vaart JI, Boon MR, Houtkooper RH. The role of AMPK signaling in brown adipose tissue activation. Cells. 2021; 10:1122. PMID:
34066631.

38. Ding X, Jian T, Li J, Lv H, Tong B, Li J, Meng X, Ren B, Chen J. Chicoric acid ameliorates nonalcoholic fatty liver disease via the AMPK/Nrf2/NF
κB signaling pathway and restores gut microbiota in high-fat-diet-fed mice. Oxid Med Cell Longev. 2020; 2020:9734560. PMID:
33204402.
39. Hu M, Zhang D, Xu H, Zhang Y, Shi H, Huang X, Wang X, Wu Y, Qi Z. Salidroside activates the AMP-activated protein kinase pathway to suppress nonalcoholic steatohepatitis in mice. Hepatology. 2021; 74:3056–3073. PMID:
34292604.

40. Entezari M, Hashemi D, Taheriazam A, Zabolian A, Mohammadi S, Fakhri F, Hashemi M, Hushmandi K, Ashrafizadeh M, Zarrabi A, et al. AMPK signaling in diabetes mellitus, insulin resistance and diabetic complications: a pre-clinical and clinical investigation. Biomed Pharmacother. 2022; 146:112563. PMID:
35062059.

41. Zhang E, Jin L, Wang Y, Tu J, Zheng R, Ding L, Fang Z, Fan M, Al-Abdullah I, Natarajan R, et al. Intestinal AMPK modulation of microbiota mediates crosstalk with brown fat to control thermogenesis. Nat Commun. 2022; 13:1135. PMID:
35241650.

42. Diniz TA, de Lima Junior EA, Teixeira AA, Biondo LA, da Rocha LA, Valadão IC, Silveira LS, Cabral-Santos C, de Souza CO, Rosa Neto JC. Aerobic training improves NAFLD markers and insulin resistance through AMPK-PPAR-α signaling in obese mice. Life Sci. 2021; 266:118868. PMID:
33310034.

43. Nagappan A, Kim JH, Jung DY, Jung MH. Cryptotanshinone from the
Salvia miltiorrhiza bunge attenuates ethanol-induced liver injury by activation of AMPK/SIRT1 and Nrf2 signaling pathways. Int J Mol Sci. 2019; 21:265. PMID:
31906014.
44. Chen J, Yang Y, Li S, Yang Y, Dai Z, Wang F, Wu Z, Tso P, Wu G. E2F1 regulates adipocyte differentiation and adipogenesis by activating ICAT. Cells. 2020; 9:1024. PMID:
32326181.

45. Wang YL, Lin SP, Hsieh PC, Hung SC. Concomitant beige adipocyte differentiation upon induction of mesenchymal stem cells into brown adipocytes. Biochem Biophys Res Commun. 2016; 478:689–695. PMID:
27498007.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download