Abstract
Background: This study aims to analyze the risk factors for urinary tract infection (UTI) by cefotaxime-resistant Escherichia coli or Klebsiella pneumoniae, using data from the National Health Insurance Data Sharing Service. Methods: A retrospective case-control study was conducted to analyze the risk factors during 11 years (2010–2020). Study groups were selected based on the laboratory data of the hospital, which comprised 3,638 and 877 cases of cefotaxime-resistant E. coli and K. pneumoniae, respectively. Controls comprised 8,994 and 1,573 cases of cefotaxime-nonresistant (intermediate or susceptible) E. coli and K. pneumoniae, respectively. Clinical and socioeconomical features were obtained from the National Health Insurance service data. Results: In a multivariate analysis of risk factors for UTI by cefotaxime-resistant E. coli, the odds ratio (OR) of the male sex was 1.335 (95% confidence interval, 1.204–1.480), age 0–9 years was 1.794 (1.468–2.191), chronic renal disease was 1.227 (1.062–1.417), and hemodialysis was 1.685 (1.255–2.262). Moreover, the ORs of L-tube, central venous pressure catheter, and Foley catheter use were 1.204 (1.047–1.385), 1.332 (1.156–1.534), and 1.473 (1.316–1.649), respectively; the OR of previous antimicrobial use was 1.103 (1.009–1.206) and that of healthcare facility use was 1.782 (1.576–2.014). In a multivariate analysis of risk factors for UTI by cefotaxime-resistant K. pneumoniae, OR of the male sex was 1.460 (1.199–1.778), liver disease was 1.295 (1.037–1.617), and hemodialysis was 2.046 (1.263–3.315). The ORs of L-tube and Foley catheter use were 2.329 (1.861–2.915) and 1.793 (1.431–2.246), respectively, and the OR of the healthcare facility use was 1.545 (1.161–2.056). Conclusion: In this study, the risk factors for UTI caused by cefotaxime-resistant E. coli or K. pneumoniae were analyzed based on the data of a specific healthcare facility linked to the National Health Insurance system. We suggest that it is a simple and effective way to elucidate risk factors of infections caused by major antimicrobial-resistant pathogens.
Urinary tract infection (UTI) refers to bacterial infection in a part of the urinary system consisting of the kidneys, ureter, bladder, and urethra [1]. UTI is a very common type of bacterial infection, and many women experience recurrent UTIs [2]. Well-known etiologic agents of UTI are Escherichia coli (most common), and other enteric gram-negative bacteria (Klebsiella, Pseudomonas, Proteus, Enterobacter, and Citrobacter spp.) [3,4]. Extended-spectrum ß-lactamase (ESBL)-producing E. coli or K. pneumoniae (most of them show the resistance to third generation cephalosporin, such as cefotaxime) are common in Korea, and resistance rates to cefotaxime were 37.1% and 24.9% for E. coli and K. pneumoniae, respectively, in 2019 [5].
The purpose of this study is to analyze the risk factors for UTI by cefotaxime-resistant E. coli or K. pneumoniae, using data from the National Health Insurance Data Sharing Service. The data of a specific healthcare facility can be linked to the national health insurance data with this service, which can be a simple and effective way, including not only the use of medical, but also service socio-demographic characteristics. With this methodology, entire antibacterial prescriptions can be obtained with this service, including antimicrobial use in the community.
A total of 599,883 cases of urine culture over 11 years (2010-2020) were linked to the national health insurance service data in one general hospital (818 beds). Excluding repeated cases and missing data, 12,632 cases of E. coli and 2,450 cases of K. pneumoniae were included for a retrospective case-control study. Based on laboratory data of the hospital, study groups were selected. Cases comprised 3,638 cases of cefotaximeresistant E. coli and 877 cases of cefotaxime-resistant K. pneumoniae, which were isolated from urine cultures (UTI patients caused by ESBL-producers). Controls comprised 8,994 cases of cefotaxime-nonresistant (intermediate or susceptible) E. coli and 1,573 cases of cefotaxime-non-resistant K. pneumoniae, which were isolated from urine cultures (UTI patients caused by non-ESBL-producers).
Clinical and socioeconomical features were obtained from the national health insurance service data. The variables were defined as follows: underlying diseases were obtained in the inpatients during the admission period or outpatients within one month, using the major diagnostic code or four minor codes (total five codes), corresponding to malignancy (C00-D48), diabetes (E10-E14), ischemic heart disease (I20-I25), cardiovascular disease (I60-I69), chronic lower respiratory disease (J40-J47), liver disease (K70-K77), and chronic renal disease (N18).
Using health insurance claim codes, major surgery history (general anesthesia prescription), hemodialysis, anticancer treatment, and total parenteral nutrition history were confirmed. The use of a device, such as an L-tube, central venous pressure (CVP) catheter, and Foley catheter was evaluated within 90 days of pathogen isolation. Previous antimicrobial use was verified within 30 days of pathogen isolation, using J01 Anatomical Therapeutic Chemical codes, excluding local application or external preparation. The healthcare facility use comprised any healthcare facilities, including clinics before 30 days of pathogen isolation. The Charlson comorbidity index (CCI) was calculated according to the previous report [6].
Statistical analysis was performed with the Chi-square test and logistic regression. SAS program version 9.4 (SAS Institute, Cary, NC, USA) was used.
In a univariate analysis, male sex, childhood or older age, underlying disease (malignancy, diabetes, ischemic heart disease, cardiovascular disease, chronic lower respiratory disease, liver disease, and chronic renal disease), hemodialysis, anticancer treatment, device use (L-tube, CVP catheter, and Foley catheter), previous antimicrobial use, frequent healthcare facility use, and high CCI (more than 3) were statistically significant for cefotaxime-resistant E. coli UTI (Table 1).
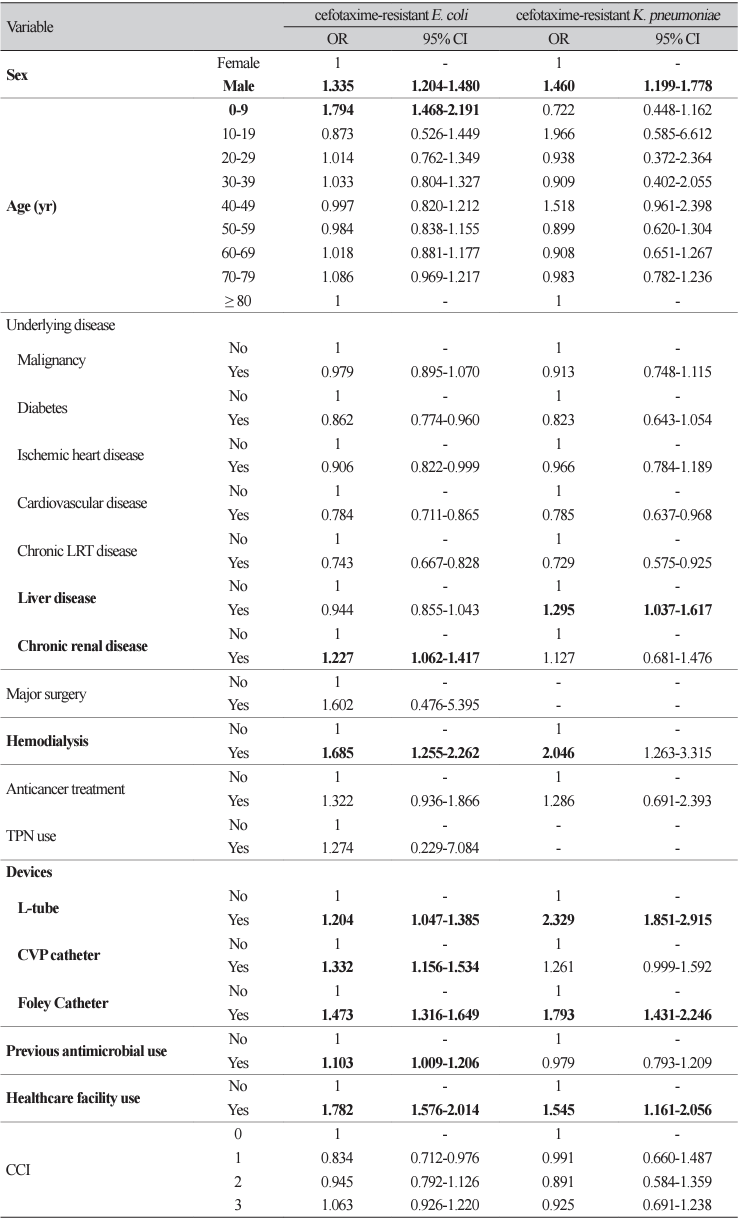
In a multivariate analysis, the odds ratio (OR) of male sex was 1.335 (95% confidential interval, 1.2041.480); OR of age 0-9 years was 1.794 (1.468-2.191); OR of chronic renal disease was 1.227 (1.062-1.417); OR of hemodialysis was 1.685 (1.255-2.262); ORs of L-tube, CVP catheter, and Foley catheter use were 1.204 (1.047-1.385), 1.332 (1.156-1.534), and 1.473 (1.316-1.649), respectively; OR of previous antimicrobial use was 1.103 (1.009-1.206); OR of healthcare facility use was 1.782 (1.576-2.014) (Table 2).
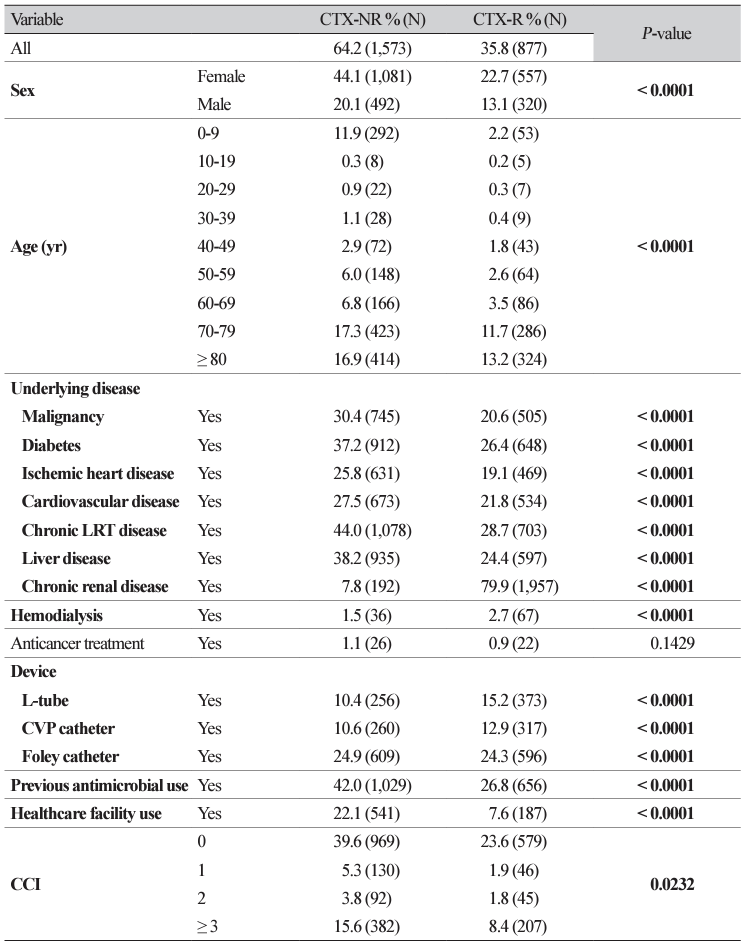
In a univariate analysis, male sex, older age, underlying disease (malignancy, diabetes, ischemic heart disease, cardiovascular disease, chronic lower respiratory disease, liver disease, and chronic renal disease), hemodialysis, device use (L-tube, CVP catheter, and Foley catheter), and previous antimicrobial use, and frequent healthcare facility use were statistically significant for cefotaxime-resistant E. coli UTI (Table 3).
In a multivariate analysis, OR of male sex was 1.460 (1.199-1.778); OR of liver disease was 1.295 (1.0371.617); OR of hemodialysis was 2.046 (1.263-3.315); OR of L-tube and Foley catheter use were 2.329 (1.861-2.915) and 1.793 (1.431-2.246), respectively; and OR of healthcare facility use was 1.545 (1.1612.056) (Table 2).
Antimicrobial resistance and emerging ESBL infections are rising concerns in public health [7]. The production of β-lactamase enzymes is the primary mechanism by which Gram-negative bacteria resist the action of all β-lactam antibiotics, except carbapenems and cephamycins [8]. Additionally, ESBL-producing isolates have demonstrated rising rates of resistance to other classes of antibiotics, such as sulfonamides, aminoglycosides, and fluoroquinolones [8]. These multidrug-resistant organisms significantly limit the treatment options, and initial empirical therapy is often ineffective and associated with poor outcomes [9].
Defining risk factors for UTI by ESBL-producing E. coli or K. pneumoniae is very important to manage antimicrobial resistance in Korea because UTIs by these organisms are very common even in the community and they frequently progress to bloodstream infections, showing a serious prognosis [10]. The well-known risk factors for community-acquired UTI by ESBL-producing E. coli were prior use of antibiotics (OR from 2.2 to 21.4), previous hospitalization (OR from 1.7 to 3.9), and UTI history (OR from 1.3 to 3.8) after reviewing 16 previous observational studies [11]. In a multicenter study, a total of 983 patient-specific isolates were reviewed (890 were E. coli, 68 were Klebsiella species, and 25 were Proteus mirabilis) and significant risk factors for ESBL-producing Enterobacteriaceae-mediated infections were recent antibiotic use, residence in a long-term care facility, recent hospitalization, age 65 years, and male sex [12]. In this study, we found similar risk factors for UTI by cefotaxime-resistant E. coli or K. pneumoniae (ESBL-producers), such as male sex, underlying disease, hemodialysis, use of a device, previous antimicrobial use, and healthcare facility.
The National Health Insurance Data Sharing Service was used in this study, which can link the data of a specific healthcare facility to the national health insurance data. The strength of this study was that whole antibacterial prescriptions can be obtained with this service, including antimicrobial use in the community and healthcare facility use can also be identified. The risk factors for UTI caused by cefotaxime-resistant E. coli or K. pneumoniae were analyzed after the data of a specific healthcare facility were linked to the national health insurance data. Therefore, we suggest that it is a simple and effective way to elucidate risk factors of infections by major antimicrobial-resistant pathogens.
Ethics statement
The Institutional Review Board of the National Health Insurance Service Ilsan Hospital approved this study (NHIMC 2022-05-019) and waiver of informed consent was obtained.
Acknowledgements
This study used the National Health Insurance Data Sharing Service with permission (NHIS-2022-1-394).
Funding
This study was funded by a grant from the National Health Insurance Service Ilsan Hospital (2021-20-001).
REFERENCES
1. Gupta K, Grigoryan L, Trautner B. Urinary tract infection. Ann Intern Med 2017;167:ITC49-64.
.
2. Jung C, Brubaker L. The etiology and management of recurrent urinary tract infections in postmenopausal women. Climacteric 2019;22:242-9.
.
3. Millner R, Becknell B. Urinary tract infections. Pediatr Clin North Am 2019;66:1-13.
.
4. Lee H, Yoon EJ, Kim D, Jeong SH, Won EJ, Shin JH, et al. Antimicrobial resistance of major clinical pathogens in South Korea, May 2016 to April 2017: first one-year report from KorGLASS. Euro Surveill 2018;23:1800047.
.
5. Kim D, Yoon EJ, Hong JS, Choi MH, Kim HS, Kim YR, et al. Major bloodstream infectioncausing bacterial pathogens and their antimicrobial resistance in South Korea, 2017-2019: Phase I report from Kor-GLASS. Front Microbiol 2022;12:799084.
.
6. Kim KH. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients. J Prev Med Public Health 2010;43:42-9.
.
7. van Driel AA, Notermans DW, Meima A, Mulder M, Donker GA, Stobberingh EE, at al. Antibiotic resistance of Escherichia coli isolated from uncomplicated UTI in general practice patients over a 10-year period. Eur J Clin Microbiol Infect Dis 2019;38:2151–8.
.
8. Rawat D, Nair D. Extended-spectrum β-lactamases in gram negative bacteria. J Glob Infect Dis 2010;2:263–74.
.
9. Al-Tamimi M, Abu-Raideh J, Albalawi H, Shalabi M, Saleh S. Effective oral combination treatment for extended-spectrum beta-lactamase-producing Escherichia coli. Microb Drug Resist 2019;25:1132–41.
.
10. Holmes CL, Anderson MT, Mobley HLT, Bachman MA. Pathogenesis of Gram-negative bacteremia. Clin Microbiol Rev 2021;34:e00234-20.
.
11. Larramendy S, Deglaire V, Dusollier P, Fournier JP, Caillon J, Beaudeau F, et al. Risk factors of extended-spectrum beta-lactamases-producing Escherichia coli community acquired urinary tract infections: a systematic review. Infect Drug Resist 2020;13:3945-55.
.
12. Ben-Ami R, Rodríguez-Baño J, Arslan H, Pitout JD, Quentin C, Calbo ES, et al. A multinational survey of risk factors for infection with extended-spectrum ß-lactamaseproducing Enterobacteriaceae in nonhospitalized patients. Clin Infect Dis 2009;49:682-90.
.
Table 1
Risk factors for cefotaxime-resistant Escherichia coli urinary tract infections: A univariate analysis.
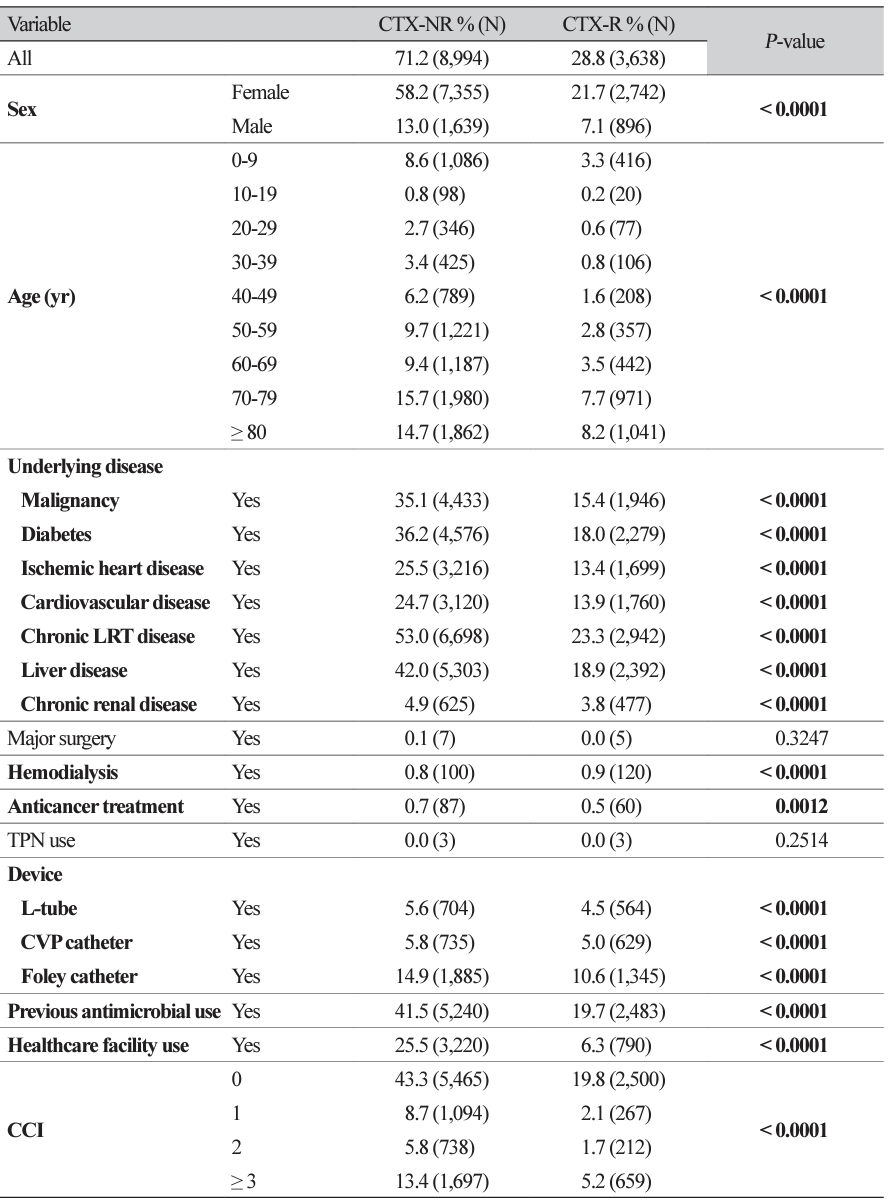
Table 2
Risk factors of cefotaxime-resistant Escherichia coli or Klebsiella pneumoniae urinary tract infections: A multivariate analysis.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download