Abstract
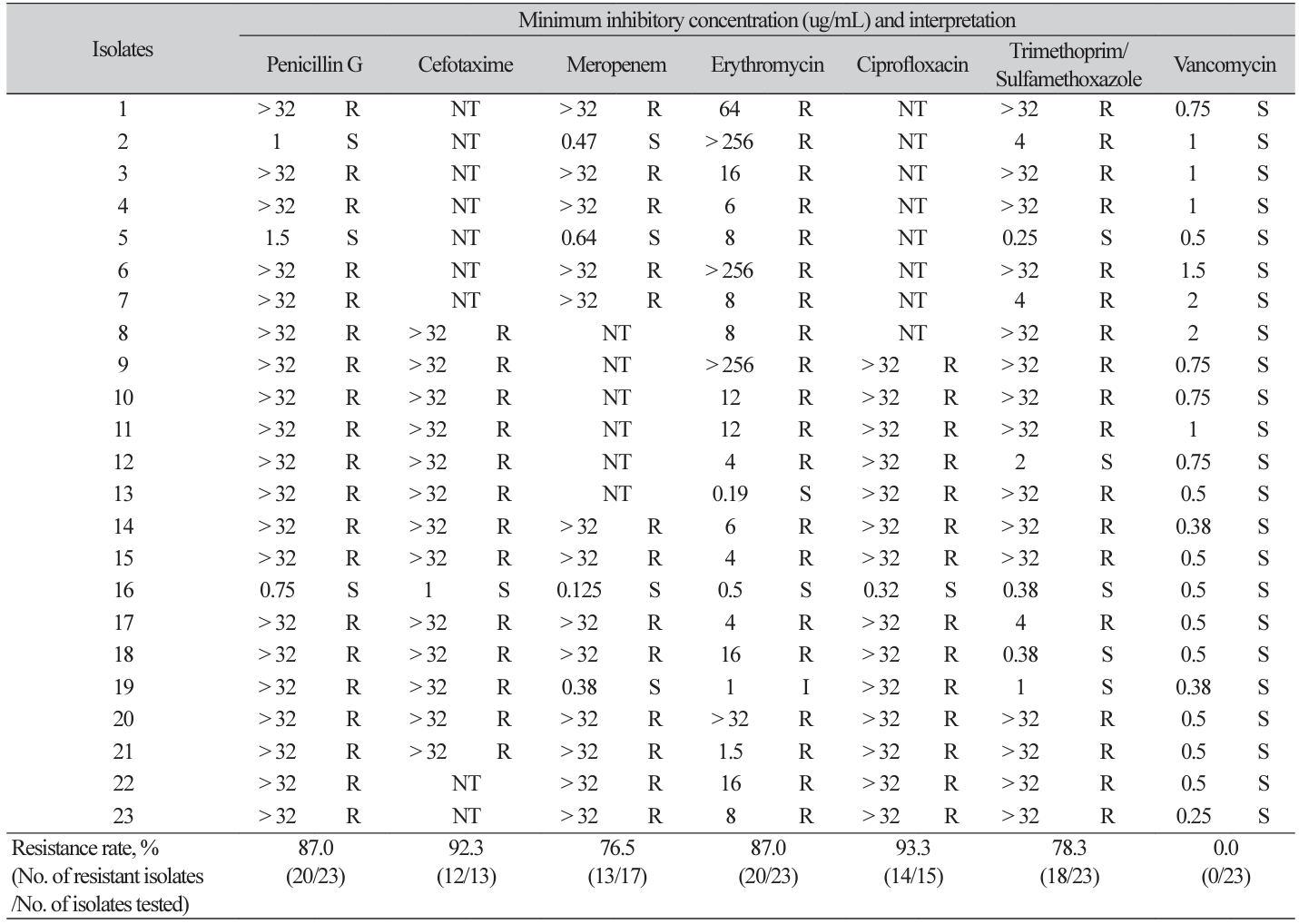
Background: Corynebacterium striatum is part of the normal flora of the skin, oral cavity, and intestine. However, it can be a pathogen causing endocarditis, pneumonia, arthritis, and meningitis occasionally. We evaluated the clinical features and antimicrobial susceptibility pattern of C. striatum cases. Methods: Patients infected with C. striatum, who consulted infectious disease physicians and were admitted to Hanyang University hospital between January 2018 and January 2021, were enrolled for an antimicrobial susceptibility test (AST). We reviewed medical records of selected patients for information on diagnosis, specimen types, and antibiotics used before and after AST. AST was performed using E-test and interpreted according to the Clinical and Laboratory Standards Institute M45 guidelines. Results: A total of 23 cases were evaluated, and average age of patients was 58.5 years. Ten cases were diagnosed sepsis. Eight cases were complicated with cancer, and five cases had wound infections. Four cases were treated with vancomycin prior to AST; in 13 cases, antibiotics were switched to vancomycin after AST. Resistance rates were highest for ciprofloxacin (93.3%), which was followed by cefotaxime (92.3%), penicillin G (87.0%), erythromycin (87.0%), trimethoprim/sulfamethoxazole (78.3%), and meropenem (76.5%). Conclusion: The patients infected by C. striatum were old and immunosuppressed, while many had cancer. Since C. striatum shows resistance to most drugs except vancomycin, we should consider conducting AST prior to antibiotic treatment.
Go to : 
[in Korean]
Ethics statement
This study was approved by the Institutional Review Board of Hanyang University Hospital (IRB No. 202112036).
REFERENCES
1. Bernard K. The genus Corynebacterium and other medically relevant coryneform-like bacteria. J Clin Microbiol 2012;50:3152-8.
.
2. Patricia MT. Bailey and Scott’s Diagnostic Microbiology. 14th ed. Elsevier, 2017:137-58.
.
3. Scholle D. A spontaneous joint infection with Corynebacterium striatum. J Clin Microbiol 2007;45:656-8.
.
4. Carroll KC, Pfaller MA, et al. Manual of Clinical Microbiology. 12th ed. American Society for Microbiology; 2019: 488-524.
.
5. Hong HL, Koh HI, Lee AJ. Native valve endocarditis due to Corynebacterium striatum confirmed by 16S ribosomal RNA sequencing: a case report and literature review. Infect Chemother 2016;48:239-45.
.
6. Renom F, Gomila F, Garau M, Gallegos MD, Guerrero D, Lalucat J, et al. Respiratory infection by Corynebacterium striatum: epidemiological and clinical determinants. New Microbes New Infect 2014;2:106-14
.
7. Cone LA, Curry N, Wuestoff MA, O’Connell SJ, Feller JF. Septic synovitis and arthritis due to Corynebacterium striatum following an accidental scalpel injury. Clin Infect Dis 1998;27:1532–3.
.
8. Weiss K, Labbé AC, Laverdière M. Corynebacterium striatum meningitis: case report and review of an increasingly important Corynebacterium species. Clin Infect Dis 1996;23:1246–8.
.
9. Song SA, Shin JH. Microbiological characteristics of Corynebacterium striatum, an emerging pathogen. Hanyang Med Rev 2018;38:93-8.
.
10. Clinical and Laboratory Standards Institute (CLSI). Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria; CLSI M45–ED3. Wayne; PA:2015.
.
11. Hahn WO, Werth BJ, Butler-Wu SM, Rakita RM. Multidrug-resistant Corynebacterium striatum associated with increased use of parenteral antimicrobial drugs. Emerg Infect Dis 2016;22:1908-14.
.
12. Otsuka Y, Ohkusu K, Kawamura Y, Baba S, Ezki T, Kimura S. Emergence of multidrugresistant Corynebacterium striatum as a nosocomial pathogen in long-term hospitalized patients with underlying diseases. Diagn Microbiol Infect Dis 2006;54:109-14.
.
Go to : 
Table 1
Clinical features and outcome of C. striatum cases between 2018 and 2021
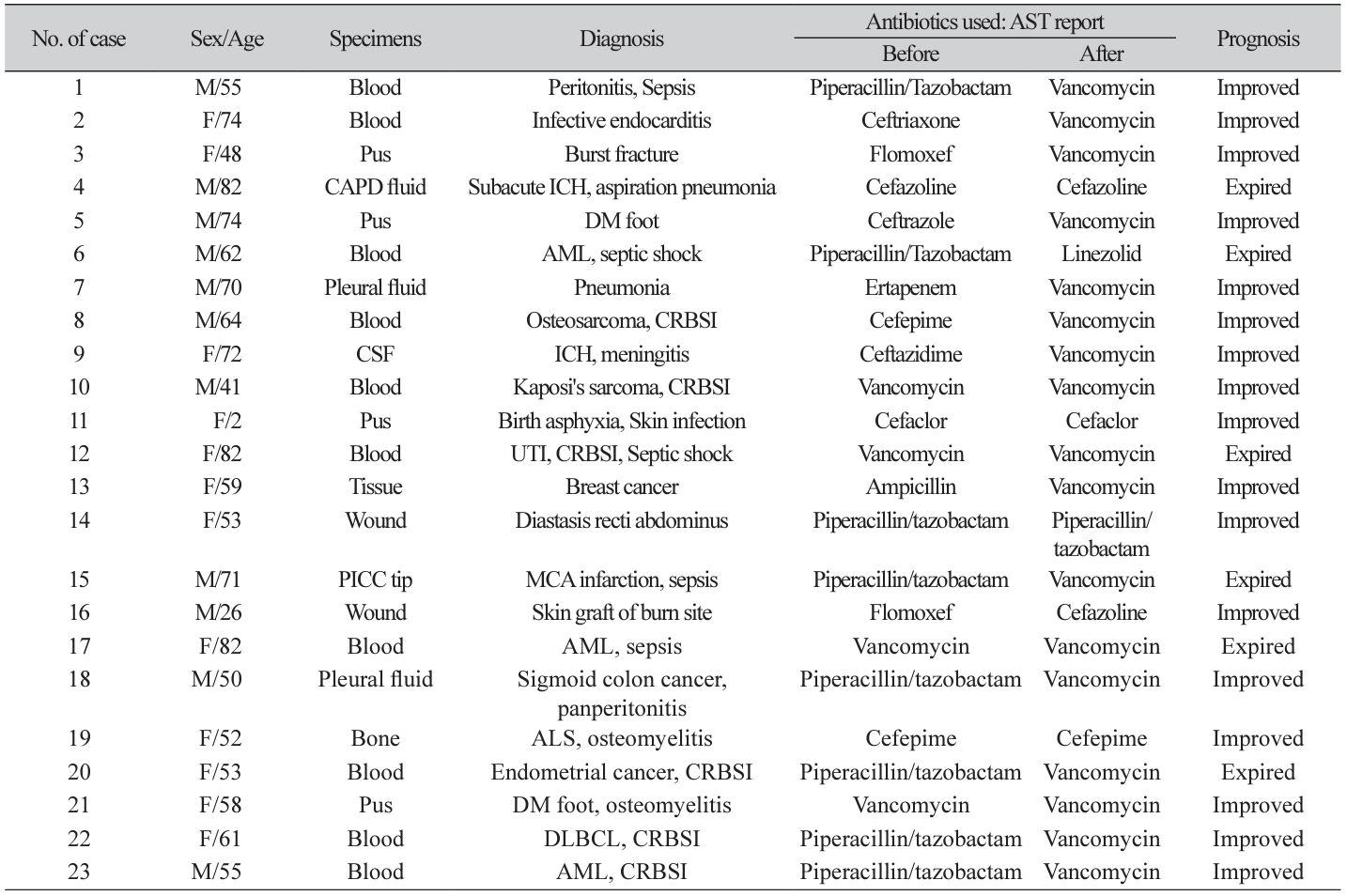
Abbreviations: M, male; F, female; AST, antimicrobial susceptibility test; CAPD, continuous ambulatory peritoneal dialysis; CSF, cerebrospinal fluid; PICC, percutaneous inserted central catheter; ICH, intracranial hemorrhage; AML, acute myeloid leukemia; CRBSI, catheter-related bloodstream infection; UTI, urinary tract infection; MCA, middle cerebral artery; ALS, amyotrophic lateral sclerosis; DLBCL, diffuse large B-cell lymphoma; DM, diabetes mellitus.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download