Abstract
Purpose
This study evaluated the difference in the recurrence of inguinal hernia in young adult patients who underwent either high ligation alone or high ligation with posterior wall repair using nationwide data.
Methods
This retrospective study included young adult patients (aged 16–30 years) who underwent surgery for inguinal hernia between June 1, 2013 and December 31, 2020. Data from the National Health Information Database from the Korea Health Insurance Service were used for this study. Patients were divided into 2 groups (high ligation alone and posterior wall repair). The primary outcome was the difference in recurrent inguinal hernia surgeries between the 2 groups.
Results
Among the 10,803 patients included in the study, 947 underwent high ligation alone, and 9,856 underwent high ligation with posterior wall repair. Recurrence was observed in 18 patients (1.9%) in the high ligation only group and 84 (0.85%) in the high ligation with posterior wall repair group. Log-rank test findings revealed that recurrence was less frequent in the high ligation with posterior wall repair group than in the high ligation only group (P = 0.003). In the multivariate analysis of factors influencing recurrence, posterior wall repair (hazard ratio, 0.241; P = 0.001) was shown to significantly lower the recurrence.
Go to : 
Inguinal hernia occurs with a bimodal peak, appearing most frequently between the ages of 1–5 and 50–70 years [1]. The most common type of inguinal hernia is indirect hernia [2]. In 2018, international guidelines for groin hernia management recommended that posterior wall repair should accompany the treatment of adult inguinal hernia [3]. For pediatric inguinal hernias, high ligation is considered as the standard treatment [4].
There is a debate about the appropriate treatment for inguinal hernia in young adults, which has a relatively low incidence rate. In 2 retrospective cohort studies conducted in 2016 [5] and 2018 [6], high ligation alone did not show any difference between high ligation with posterior wall repair and recurrence rates. However, these were retrospective, single-center studies. Furthermore, the 2018 international guidelines for groin hernia management have not provided recommendations for appropriate treatment of young adults.
Therefore, we aimed to evaluate the difference in recurrence after surgery between high ligation alone and high ligation with posterior repair for inguinal hernias in young adults using nationwide data.
Go to : 
This study was exempted from approval by the Institutional Review Board as it utilized anonymized data from the National Health Information Database (NHID) hosted by the Korean Health Insurance Service (NHIS). The requirement for informed consent for participation was waived by the Institutional Review Board of the Catholic University of Korea (No. UC22ZISE0022).
Young adult patients (aged 16–30 years) who underwent surgery for inguinal hernia from June 1, 2013 to December 31, 2020 were included in this study using NHID from NHIS.
Based on the International Classification of Diseases (ICD-10) codes, inguinal hernia was defined as a condition, which was classified as K40, and treatment codes Q2755 (high ligation) and Q2756 (high ligation with posterior wall repair) were investigated as the surgical codes. Q2756 (high ligation with posterior wall repair) included both tissue and mesh repairs. To specifically select indirect hernia, bilateral inguinal hernia (K400, K402), direct inguinal hernia (K4090.001), oblique inguinal hernia (K4090.003), scrotal hernia (K4090.004), and bubonocele (K4090.005) were excluded from the analysis. Recurrence was investigated in patients with a treatment code for recurrent inguinal hernia surgery (QA753-756).
The selected patients were divided into 2 groups (high ligation only and high ligation with posterior wall repair), and data on the following variables were collected: sex, age, past medical history, height, weight, body mass index (BMI), social history (smoking or alcohol drinking), and recurrent inguinal hernia surgery (treatment code: QA753-756).
The primary outcome was the difference in recurrent inguinal hernia surgeries between the 2 groups.
The Student t-test was used to analyze continuous variables, and the chi-square test was used for categorical variables. To compare the recurrence of inguinal hernia between the 2 groups, a log-rank test, including the Kaplan-Meier curve, was used. Cox regression analysis was applied for the multivariate analysis of the factors affecting the recurrence.
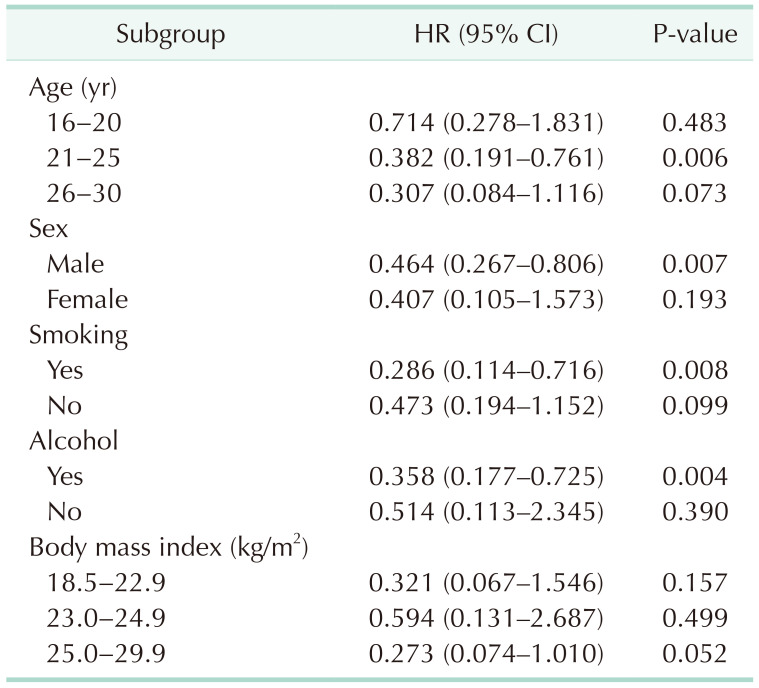
Subgroup analysis was performed to determine the hazard ratio (HR) for the recurrence of posterior repair in each categorized group for all the patients.
Statistical analyses were performed using SAS statistical software ver. 9.4 for Windows (SAS Institute Inc.). The P-values of <0.5 were considered statistically significant.
Go to : 
Among 19,002 patients under the age of 30 years who were diagnosed with inguinal hernia (K40) from June 2013 to December 2020, those with bilateral inguinal hernia (K400, K402), those with direct inguinal hernia (K4090.001), those with oblique inguinal hernia (K4090.003), those with scrotal hernia (K4090.004), those with bubonocele (K4090.005), those who underwent surgery (n = 917), those with no surgical code (n = 459), and those aged 0–15 years (n = 6,823) were excluded (Fig. 1).
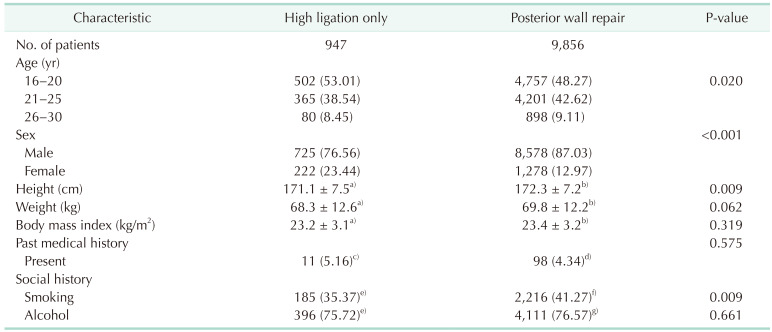
Among the 10,803 patients included, 947 underwent high ligation alone, and 9,856 underwent high ligation with posterior wall repair. The baseline characteristics of the patients are presented in Table 1. Patients in the high ligation only group were younger (P = 0.02), had a shorter height (P = 0.0092), and had a higher proportion of female sex (P < 0.0001).
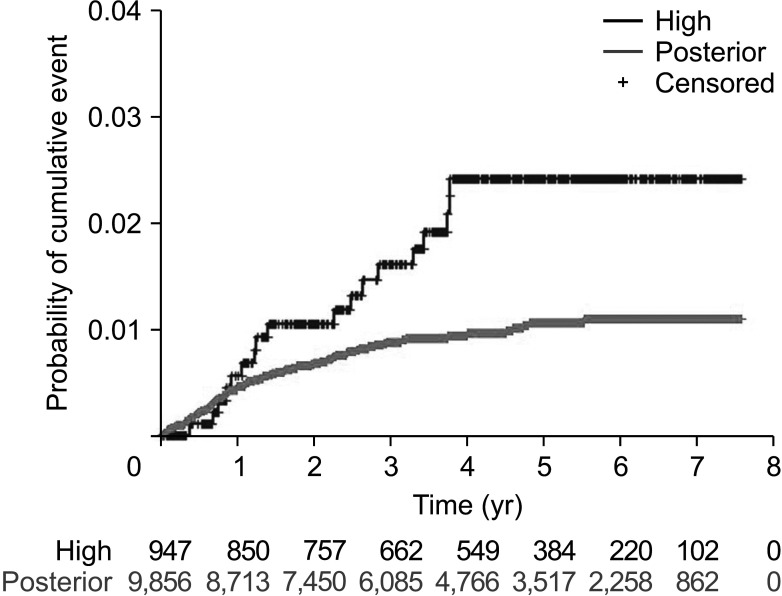
During the average follow-up period of 1,436 days (1,543.9±781.4 and 1,425.7±801.5 days for the high ligation only and high ligation with posterior wall repair groups, respectively), recurrence occurred in 18 (1.9%) and 84 (0.85%) patients in the high ligation only and high ligation with posterior wall repair groups, respectively.
Recurrence occurred less frequently in the high ligation with posterior wall repair group than in the high ligation only group (P = 0.003) (Fig. 2).
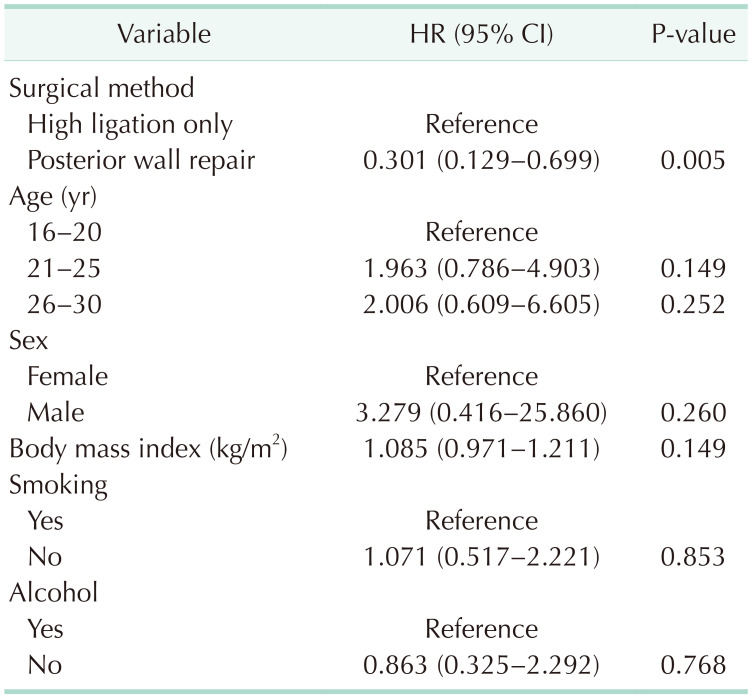
In the multivariate analysis of factors influencing the recurrence, posterior wall repair (HR, 0.301; P = 0.005) was observed to significantly lower the recurrence (Table 2).
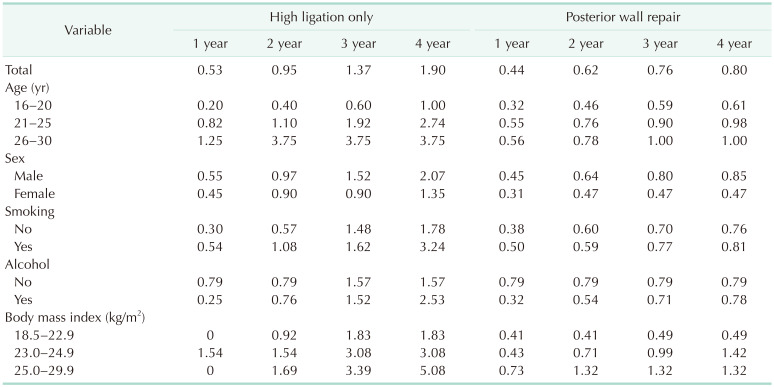
A subgroup analysis was performed to identify the cohort of patients that would benefit from posterior wall repair. The cumulative recurrence rates are presented according to the subgroup in Table 3. Accordingly, patients aged 21–25 years (HR, 0.382; 95% confidence interval [CI], 0.191–0.761; P = 0.0111), male individuals (HR, 0.464; 95% CI, 0.267–0.806; P = 0.0065), smokers (HR, 0.285; 95% CI, 0.114–0.716; P = 0.0075), and alcohol drinkers (HR, 0.358; 95% CI, 0.177–0.725; P = 0.0019) were shown to significantly benefit from the procedure (Table 4).
Go to : 
Our study demonstrated that performing additional posterior wall repair can reduce the recurrence compared with high ligation alone in young adults undergoing inguinal hernia repair. Furthermore, we demonstrated that high ligation alone might be sufficient for female patients and those aged 16–20 years.
To the best of our knowledge, this is the first nationwide cohort study to demonstrate the importance of posterior wall repair for inguinal hernia in young adults. In a single-center, retrospective study conducted by van Kerckhoven et al. [5] in 2016 on 148 young adults aged 18–30 years, the overall recurrence rate was 2.7%, and high ligation alone showed no recurrence compared with mesh repair. Criss et al. [6] in 2018 reported that there was no statistically significant difference in recurrence between mesh repair and high ligation (5.8% vs. 6.3%, P = 0.570), although their study compared young adults (average age of 21.9 years) and adolescents (average age of 15.5 years). These 2 studies have the disadvantage of having a retrospective design; therefore, there is insufficient evidence to determine the effect of posterior wall repair in young adults. However, our large cohort study demonstrates that posterior wall repair can reduce the recurrence.
One of the causes of inguinal hernia is patent processus vaginalis [2]. We have shown through subgroup analyses that high ligation alone may be sufficient for the treatment of inguinal hernia in young women. This reinforces that the most common cause of inguinal hernia in young women is likely to be patent processus vaginalis. However, direct- or femoral hernia can occur with age, although the lifetime occurrence of groin hernia in women is only 3%–6%; among them, the frequency of femoral hernia is only 3% [7].
We attempted to identify the patient groups that would benefit from posterior wall repair through a subgroup analysis. Accordingly, this study demonstrated that posterior wall repair was effective in patients who were aged 21–25 years, male, alcohol drinkers, and smokers. Because the proportion of patients aged 26–30 years included in our study was only approximately 9% of the total cohorts, there was no significance in recurrence, although the patients who underwent posterior wall repair had a lower recurrence rate than those who underwent high ligation only. Furthermore, since adolescents were included in the patient group below 20 years of age in our study, we suggest that high ligation alone would be sufficient, as reported in previous studies [56]. Factors, such as smoking [8] and a high BMI [9], are known to affect the recurrence of inguinal hernia. Although neither smoking nor a high BMI was a statistically independent factor for recurrence in our study, patients who are smokers and have a high BMI should be concerned about the possibility of recurrence. Therefore, posterior wall repair is strongly recommended to prevent recurrence. In contrast, in young adults aged 16–20 years, high ligation alone can be a surgical option.
In our study, the average follow-up period was 1,436 days. According to a multicenter retrospective study conducted in Korea [10], hernia recurrence rate was highest up to 2 years postoperatively (17.3% within 1 year and 7.5% in 1–2 years), and it was <7% after 4 years. Since it has been reported that there is a decreasing trend, 4 years is considered to be an appropriate period. In particular, since the present study is to confirm whether high ligation is a technically appropriate procedure in young adults, early recurrence (within 2 years) seems important.
The limitations of this study are as follows. First, since our study analyzed recurrence only in cases where surgery was performed for recurrence, the actual recurrence rate (recurrence in patients who did not undergo surgery) may be higher than what the results of our study estimate. Second, due to the limitation of the NHIS-NHID, it is not possible to check the surgical records of each patient; therefore, it is difficult to determine the specific characteristics of the hernia, surgical method, and level of skill of the surgeon in hernia surgery. Furthermore, we cannot rule out the possibility that primary inguinal hernia repair is identified as recurrent inguinal hernia repair in the entered data. Moreover, when billing medical expenses to the National Health Insurance Service, there may have been cases where posterior wall repair was also claimed for patients who underwent high ligation only. Third, we tried to exclude direct inguinal hernia; however, sometimes, the type of hernia could not be clearly identified in cases where direct and indirect hernias were not clearly distinguished when inputting the ICD codes in the clinical field. Finally, differences in baseline characteristics between the 2 groups may have influenced the results. Therefore, propensity score matching was attempted, although due to the large amount of missing data on BMI, social history, among others, 208 people were assigned to each group. Therefore, propensity score matching was not performed in this study because selection bias was expected to increase. Alternatively, multivariate analysis was performed to compensate for these differences, and a positive effect of posterior wall repair was observed.
In conclusion, posterior wall repair should be performed for inguinal hernias in young adults. High ligation alone can be a surgical option for female and 16–20-year-old adults. However, because of the limitations of our study, the effect of posterior repair must be demonstrated in a multicenter randomized study.
Go to : 
ACKNOWLEDGEMENTS
This study used the NHIS-NHID (National Health Insurance Service-National Health Information Database; NHIS-2022-1-763) created by the National Health Insurance Service. The authors wish to acknowledge the financial support provided by Clinical Research Laboratory Foundation of The Catholic University of Korea, Uijeongbu St. Mary’s Hospital, in the program year of 2022.
Go to : 
References
1. Han SR, Kim HJ, Kim NH, Shin S, Yoo RN, Kim G, et al. Inguinal hernia surgery in Korea: nationwide data from 2007-2015. Ann Surg Treat Res. 2019; 97:41–47. PMID: 31297352.
2. Hammoud M, Gerken J. Inguinal hernia. StatPearls [Internet]. StatPearls Publishing;2024. 01. Updated 2023 Aug 8. cited 2023 Nov 30. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513332/
.
3. HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018; 22:1–165.
4. Gauderer MW, Cina RA. Chapter 36: Hernias of the inguinal region. Ziegler MM, Azizkhan RG, Allmen Dv, Weber TR, editors. Operative pediatric surgery. 2nd ed. McGraw-Hill Education;2014. p. 489–509.
5. van Kerckhoven G, Toonen L, Draaisma WA, de Vries LS, Verheijen PM. Herniotomy in young adults as an alternative to mesh repair: a retrospective cohort study. Hernia. 2016; 20:675–679. PMID: 27522362.
6. Criss CN, Gish N, Gish J, Carr B, McLeod JS, Church JT, et al. Outcomes of adolescent and young adults receiving high ligation and mesh repairs: a 16-year experience. J Laparoendosc Adv Surg Tech A. 2018; 28:223–228. PMID: 29261090.
7. oethals A, Azmat CE, Adams CT. Femoral hernia. StatPearls [Internet]. StatPearls Publishing;2024. 01. updated 2023 Jul 31. cited 2023 Nov 30. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK535449/
.
8. DeLancey JO, Blay E, Hewitt DB, Engelhardt K, Bilimoria KY, Holl JL, et al. The effect of smoking on 30-day outcomes in elective hernia repair. Am J Surg. 2018; 216:471–474. PMID: 29559083.
9. Schjøth-Iversen L, Refsum A, Brudvik KW. Factors associated with hernia recurrence after laparoscopic total extraperitoneal repair for inguinal hernia: a 2-year prospective cohort study. Hernia. 2017; 21:729–735. PMID: 28752424.
10. Lee CS, Kim JH, Choi BJ, Lee JI, Lee SC, Lee YS, et al. Retrospective study on prevalence of recurrent inguinal hernia: a large-scale multi-institutional study. Ann Surg Treat Res. 2020; 98:51–55. PMID: 31909050.
Go to : 




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download