Abstract
Purpose
Whether a dilated intrahepatic bile duct (IHBD) has any effect on the prognosis of choledochal cyst (CC) remains controversial. We aimed to summarize the clinical characteristics and prognosis of CC with IHBD dilatation.
Methods
One hundred ninety-two children diagnosed with CC were identified, including 127 without IHBD dilatation (group A) and 65 with IHBD dilatation (group B). A retrospective analysis was performed to explore the clinical characteristics and prognosis of CC with IHBD dilatation based on clinical indices, symptoms, and complications.
Results
Compared with group A, incidences of jaundice and fever were higher in group B (P = 0.010 and P = 0.033). Preoperative total bilirubin, direct bilirubin, and indirect bilirubin were increased in group B compared to group A (P = 0.005, P < 0.001, and P = 0.014), as were preoperative ALT, AST, γ-GT, and total bile acid (P = 0.006, P = 0.025, P < 0.001, and P = 0.024). The risk of liver fibrosis or cirrhosis was significantly increased for group B compared with group A (P = 0.012) and also occurred earlier in group B (P = 0.006). In the dilated IHBDs, 95.4% (62 of 65) recovered to normal, and more than half of dilated IHBDs (37 of 65) recovered to normal in 1 week.
Choledochal cysts (CCs) are cystic or fusiform dilations of the common bile duct. As advanced imaging techniques facilitate improved CC diagnostics, its incidence has increased, particularly in neonates due to a distinct increase in prenatally diagnosed CC [1]. The clinical features of CC differ according to age. Neonates and young infants usually present with an abdominal mass, jaundice, or acholic stools, depending on the degree of obstruction. To date, CC is primarily grouped according to the Todani classification that was proposed in 1977, in which Todani type IV-a cysts are accompanied by intrahepatic bile duct (IHBD) dilation. The incidence of IHBD dilatation accounts for 30%–40% of all CC cases [2]. After properly dealing with the extrahepatic bile ducts (EHBDs), spontaneous extinction of the IHBD dilatation occurs early in some cases; however, some IHBD dilatation is persistent, and whether this residual dilatation has any effect on the long-term prognosis of children with CC is unclear.
In this study, we reviewed our institution’s records from October 2016 to December 2019 for cases of CCs, which revealed that CC with IHBD dilatation had conspicuous pre- and postoperative clinical characteristics compared with CC cases without IHBD dilatation. Thus, we summarized the clinical characteristics and outcomes of CC with IHBD dilatation based on the clinical symptoms, laboratory indices, and liver biopsies to establish guidelines for the future clinical management of this disease.
This study was carried out in accordance with the Declaration of Helsinki and the recommendations of the Ethics Committee of The Children’s Hospital, Zhejiang University School of Medicine. The protocol was approved by the Ethics Committee of The Children’s Hospital, Zhejiang University School of Medicine (No. 2020-IRB-055), and informed consent was obtained from all of their parents.
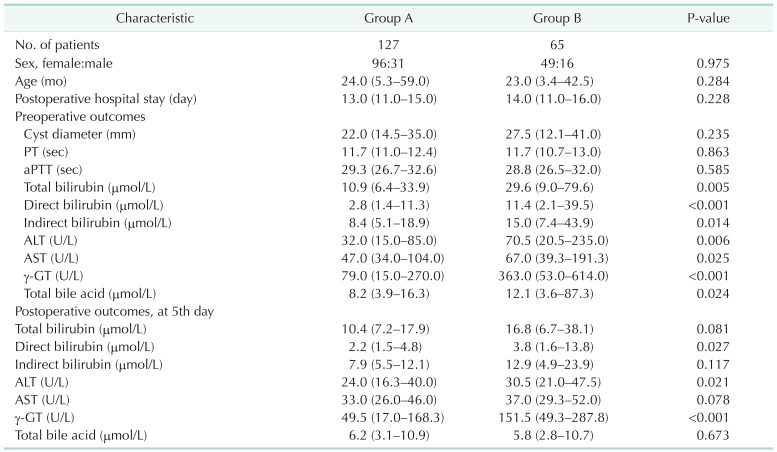
In total, data from 192 CC patients (47 males and 145 females) who were treated at the Department of General Surgery, Children’s Hospital of Zhejiang University School of Medicine between October 2016 and December 2019 were collected. Group A included 127 CC patients (31 males and 96 females) without IHBD dilatation. Group B included 65 CC patients (16 males and 49 females) with IHBD dilatation. All operations were performed by the same experienced surgeon and dilatation EHBDs were verified by this surgeon. Variables including clinical symptoms (fever, abdominal pain, jaundice, and vomiting) and preoperative and postoperative clinical indices were recorded and provided in Table 1.
The inclusion criteria for group B included: (1) a preoperative abdominal scan (B ultrasound, CT, or magnetic resonance cholangiopancreatography [MRCP]) showed moderately-to-severely dilatated IHBD [3]; (2) dilatated EHBDs were identified during surgery; (3) postoperative pathological confirmation of CC; and (4) well-documented clinical data were available. The remaining CC patients were included in group A.
Group A included 31 patients who were diagnosed by B ultrasound, 90 patients diagnosed by MRCP, and 6 patients diagnosed by CT, among which, 28 patients were diagnosed during prenatal screening. Group B included 16 patients who were diagnosed by B ultrasound, 46 patients diagnosed by MRCP, and 3 patients diagnosed by CT, among which, 15 patients were diagnosed during prenatal screening. All the diagnoses of liver fibrosis or cirrhosis were confirmed by pathology. During follow-up, liver cirrhosis was examined mainly by liver grayscale stereo imaging, which can provide an accurate number to evaluate the degree of cirrhosis.
All patients received excision of dilated EHBDs and hepaticojejunostomy, which were performed by one experienced surgeon. Patients received postoperative imipenem-cilastatin sodium as an antimicrobial treatment for 3–5 days, at which time the antibiotic was changed to cephalosporin if the WBC count and CRP levels decreased and the patient had recovered well. The gastrointestinal decompression tube could be removed 5 days postoperatively if the patients felt well (without nausea, vomiting, or abdominal distension), then liquid and semiliquid diets could be gradually introduced. The abdominal drainage tube could be removed when the postoperative daily drainage volume was less than 15–20 mL and the ascites were less than 2 cm.
Data are presented as the median with interquartile range (IQR). All statistical analyses were performed with PASW Statistics ver. 18.0 (IBM Corp.) and GraphPad Prism 6 (GraphPad Software, Inc.) software packages. The independent samples t-test was used to compare samples. Comparisons of liver fibrosis and cirrhosis were conducted by the chi-square test. Survival curves were drawn using Kaplan-Meier univariate estimates. A P-value of <0.05 was considered statistically significant.
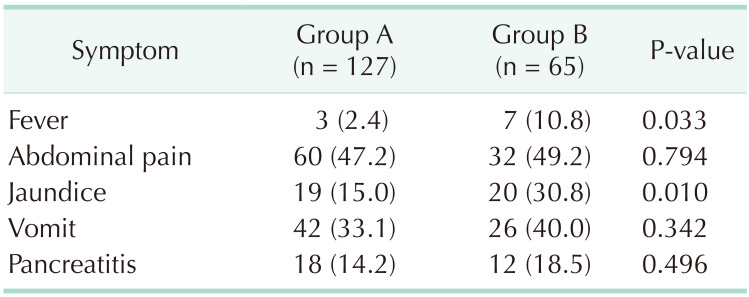
In total, 192 CC patients (47 males and 145 females) were included in this study, among whom 127 (31 males and 96 females) were without IHBD dilatation (group A), and 65 (16 males and 49 females) had IHBD dilatation (group B). The proportions of symptomatic patients were 63.0% in group A and 75.4% in group B. In both groups, abdominal pain was the most common symptom (47.2% in group A and 49.2% in group B), followed by vomiting, jaundice, and fever. The incidence of jaundice and fever in group B was significantly higher than in group A (P = 0.010 and P = 0.033, respectively) (Table 2).
The diameters of the cysts were measured by B ultrasound, CT, or MRCP and were not significantly different between the 2 groups (22.0 mm [IQR, 14.5–35.0 mm] vs. 27.5 mm [IQR, 12.1–41.0 mm]). Preoperative PT and aPTT were also not significantly different between the 2 groups (PT, 11.7 seconds [IQR, 11.0–12.4 seconds] vs. 11.7 seconds [IQR, 10.7–13.0 seconds]; aPTT: 29.3 seconds [IQR, 26.7–32.6 seconds] vs. 28.8 seconds [IQR, 26.5–32.0 seconds]). The incidence of jaundice in group B was significantly higher than in group A (P = 0.010), and preoperative total bilirubin (TB), direct bilirubin (DB), and indirect bilirubin (IDB) levels were also higher in group B (P = 0.005, P < 0.001, and P = 0.014, respectively). Compared with group A, preoperative ALT and AST were significantly increased in group B (P = 0.025 and P = 0.006, respectively). Finally, preoperative γ-GT levels were also significantly higher in group B compared with group A (363.0 U/L [IQR, 53.0–614.0 U/L] vs. 79.0 U/L [IQR, 15.0–270.0 U/L], P = 0.024) (Table 1).
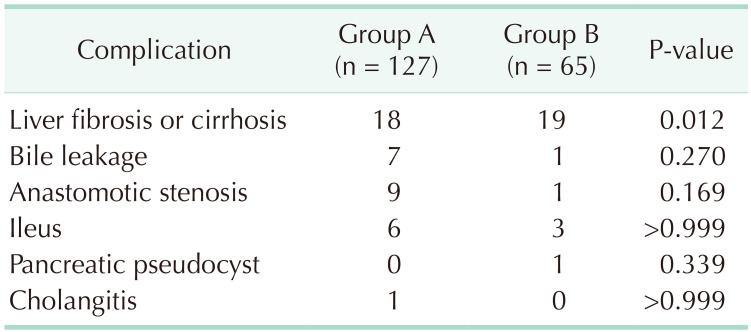
Following surgery, the average levels of TB, DB, IDB, ALT, AST, and γ-GT recovered to normal at day 5 in group A; these same indices also recovered to normal at day 5 in group B, except γ-GT, which remained significantly increased (151.5 U/L [IQR, 49.3–287.8 U/L] vs. 49.5 U/L [IQR, 17.0–168.3 U/L], P < 0.001] (Table 1). Further analysis of liver biopsies from the 2 groups showed that the proportion of liver fibrosis and cirrhosis was significantly increased in group B compared with group A (P = 0.012) (Table 3). Also, the postoperative complications of bile leakage, anastomotic stenosis, ileus, pancreatic pseudocyst, and cholangitis did not show significant differences between the 2 groups (P = 0.270, P = 0.169, P > 0.999, P = 0.339, and P > 0.999, respectively) (Table 3). Finally, Kaplan-Meier analysis indicated that liver fibrosis and cirrhosis occurred earlier in group B than in group A (P = 0.006) (Fig. 1). Among group B, 95.4% of dilated IHBDs (62 of 65) recovered to normal, and more than half of the patients (37 of 65) with dilated IHBDs recovered to normal in 1 week.
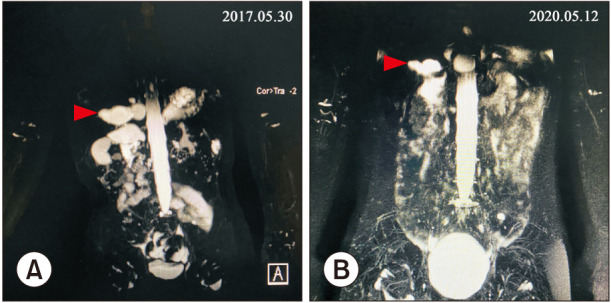
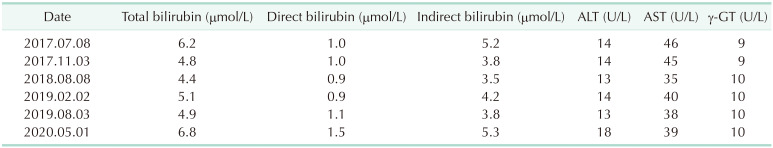
The average follow-up time was 13.2 months (IQR, 2.5–32.3 months) and 12.4 months (IQR, 1.6–29.0 months) months in group A and group B, respectively. In the dilated IHBDs, 95.4% (62 of 65) recovered to normal, and more than half of the patients (37 of 65) with dilated IHBDs recovered to normal in 1 week in group B. The follow-up time of 1 patient who experienced persistent, remarkable gourd-shaped IHBD dilatation was 34 months.
Type IV-a CC has been reported more and more in recent years, and accounts for up to 29% of some series [4]. In our series, type IV-a CC accounts for 33.9% of all patients. Here, we have found that CC patients with IHBD dilatation had conspicuous clinical symptoms. Patients with initial manifestation of CC usually have nonspecific symptoms, and the classic triad (abdominal pain, jaundice, and abdominal mass) has proven to be rare [2]. In this study, the predominant symptoms were abdominal pain and vomiting, followed by jaundice and fever. The incidence of the latter 2 symptoms was much higher in patients with IHBD dilatation. It is probable that the increased pressure in the biliary tract results from biliary obstruction, and poor bile drainage is more prone to cause recurrent fever and jaundice [56]. The significantly elevated pre- and postoperative γ-GT levels in group B, which was related to the biliary obstruction [78], further verified the increased biliary pressure. Notably, previous studies also confirmed a significant stepwise increased pressure between 2 common types (type 1 < type 4) [910].
It has been shown that early excision of the extrahepatic portion of the cyst for type IV-a CC without removing the cystic dilation of IHBD provides a satisfactory prognosis [1112]. Previous studies had also reported that the intrahepatic portion of the cyst diminished or disappeared after surgery, and that preoperative IHBD dilatation was not significantly associated with prognosis [1213]. In our study, type IV-a CC patients with early surgeries experienced satisfactory outcomes, and most of the dilated IHBDs recovered to normal in a short time. Only 1 patient experienced persistent, remarkable gourd-shaped IHBD dilatation (Fig. 2, Table 4), and this patient also experienced a satisfactory recovery of liver function. However, those patients with persistent IHBD dilatation need longer-term follow-up to confirm whether the remaining intrahepatic cysts will influence their symptom-free survival. Some studies reported that the incidence of malignancy was higher in patients who underwent Roux-en-Y hepaticojejunostomy without radical resection of cysts compared with patients who did not undergo any surgery [14], and the dilated bile ducts might be vulnerable to bile infection, resulting stone formation [15]. As previously reported, the incidence of a combined malignancy on the biliary tracts after the resection of CCs should draw attention [16]. Also, such cases in which intrahepatic cholangiocarcinoma arises many years after excision of a type IV-a congenital CC have occasionally been reported [1718]. According to previous research, the incidence of malignancy before the age of 18 years was 0.42% vs. 11.4% in adults [19]. Although postoperative hepatic biochemical indices were restored to normal early in our cohort, the incidences of liver fibrosis or cirrhosis were significantly increased in group B. It is gratifying that only 2 patients with IHBDs had liver cirrhosis at 8.2 and 9.8 months postoperatively. However, it is noteworthy that our Kaplan-Meier analysis used liver fibrosis as a preliminary biomarker for patient assessments [20] and indicated that liver fibrosis or cirrhosis appeared significantly earlier in type IV-a CC.
In conclusion, CC patients with IHBD dilatation had relatively conspicuous preoperative symptoms, highly elevated bilirubin, and abnormal liver function, and they were more prone to develop liver fibrosis or cirrhosis in the early stages. Although patients with IHBD dilatation experience satisfactory outcomes and most of the IHBD dilatation diminishes spontaneously in a short time, proactive treatment is recommended once surgical contraindications are excluded for CC patients with IHBD dilatation, and meticulous follow-up is needed.
Notes
References
1. Matsumoto M, Urushihara N, Fukumoto K, Yamoto M, Miyake H, Nakajima H. Laparoscopic management for prenatally diagnosed choledochal cysts. Surg Today. 2016; 46:1410–1414. PMID: 26935547.
2. Koshinaga T, Inoue M, Ohashi K, Sugito K, Ikeda T, Hagiwara N, et al. Persistent biliary dilatation and stenosis in postoperative congenital choledochal cyst. J Hepatobiliary Pancreat Sci. 2011; 18:47–52. PMID: 20521068.
3. Congo K, Lopes MF, Oliveira PH, Matos H, Basso S, Reis A. Outcomes of choledochal cysts with or without intrahepatic involvement in children after extrahepatic cyst excision and Roux-en-Y hepaticojejunostomy. Ann Hepatol. 2012; 11:536–543. PMID: 22700636.
4. Saluja SS, Nayeem M, Sharma BC, Bora G, Mishra PK. Management of choledochal cysts and their complications. Am Surg. 2012; 78:284–290. PMID: 22524764.
5. Fujishiro J, Masumoto K, Urita Y, Shinkai T, Gotoh C. Pancreatic complications in pediatric choledochal cysts. J Pediatr Surg. 2013; 48:1897–1902. PMID: 24074664.
6. Kaneko K, Ono Y, Tainaka T, Sumida W, Ando H. Fatty acid calcium stones in patients with pancreaticobiliary maljunction/choledochal cyst as another cause of obstructive symptoms besides protein plugs. J Pediatr Surg. 2008; 43:564–567. PMID: 18358304.
7. Lieberman MW, Barrios R, Carter BZ, Habib GM, Lebovitz RM, Rajagopalan S, et al. gamma-Glutamyl transpeptidase. What does the organization and expression of a multipromoter gene tell us about its functions? Am J Pathol. 1995; 147:1175–1185. PMID: 7485380.
8. Cabrera-Abreu JC, Green A. Gamma-glutamyltransferase: value of its measurement in paediatrics. Ann Clin Biochem. 2002; 39:22–25. PMID: 11853185.
9. Hill R, Parsons C, Farrant P, Sellars M, Davenport M. Intrahepatic duct dilatation in type 4 choledochal malformation: pressure-related, postoperative resolution. J Pediatr Surg. 2011; 46:299–303. PMID: 21292077.
10. Kronfli R, Davenport M. Insights into the pathophysiology and classification of type 4 choledochal malformation. J Pediatr Surg. 2020; 55:2642–2646. PMID: 32561173.
11. Zheng X, Gu W, Xia H, Huang X, Liang B, Yang T, et al. Surgical treatment of type IV-A choledochal cyst in a single institution: children vs. adults. J Pediatr Surg. 2013; 48:2061–2066. PMID: 24094958.
12. Ono S, Fumino S, Shimadera S, Iwai N. Long-term outcomes after hepaticojejunostomy for choledochal cyst: a 10- to 27-year follow-up. J Pediatr Surg. 2010; 45:376–378. PMID: 20152355.
13. Ohi R, Koike N, Matsumoto Y, Ohkohchi N, Kasai M. Changes of intrahepatic bile duct dilatation after surgery for congenital dilatation of the bile duct. J Pediatr Surg. 1985; 20:138–142. PMID: 3891953.
14. Ziegler KM, Zyromski NJ. Choledochoceles: are they choledochal cysts? Adv Surg. 2011; 45:211–224. PMID: 21954689.
15. Uno K, Tsuchida Y, Kawarasaki H, Ohmiya H, Honna T. Development of intrahepatic cholelithiasis long after primary excision of choledochal cysts. J Am Coll Surg. 1996; 183:583–588. PMID: 8957460.
16. Han WS, Kim H, Sohn HJ, Lee M, Kang YH, Kim HS, et al. Clinical characteristics of patients with malignancy and long-term outcomes of surgical treatment of patients with choledochal cyst. Ann Surg Treat Res. 2021; 101:332–339. PMID: 34934760.
17. Mizuguchi Y, Nakamura Y, Uchida E. Subsequent biliary cancer originating from remnant intrapancreatic bile ducts after cyst excision: a literature review. Surg Today. 2017; 47:660–667. PMID: 27324392.
18. Shimamura K, Kurosaki I, Sato D, Takano K, Yokoyama N, Sato Y, et al. Intrahepatic cholangiocarcinoma arising 34 years after excision of a type IV-A congenital choledochal cyst: report of a case. Surg Today. 2009; 39:247–251. PMID: 19280286.
19. Sastry AV, Abbadessa B, Wayne MG, Steele JG, Cooperman AM. What is the incidence of biliary carcinoma in choledochal cysts, when do they develop, and how should it affect management? World J Surg. 2015; 39:487–492. PMID: 25322698.
20. Dong JH, Yang SZ, Xia HT, Duan WD, Ji WB, Gu WQ, et al. Aggressive hepatectomy for the curative treatment of bilobar involvement of type IV-A bile duct cyst. Ann Surg. 2013; 258:122–128. PMID: 23478522.
Fig. 1
Prognostic analyses of choledochal cyst patients with or without intrahepatic bile duct dilatation. Kaplan-Meier analysis of liver fibrosis- or cirrhosis-free survival for group A (high) and group B (low) was analyzed. Log-rank test was used.
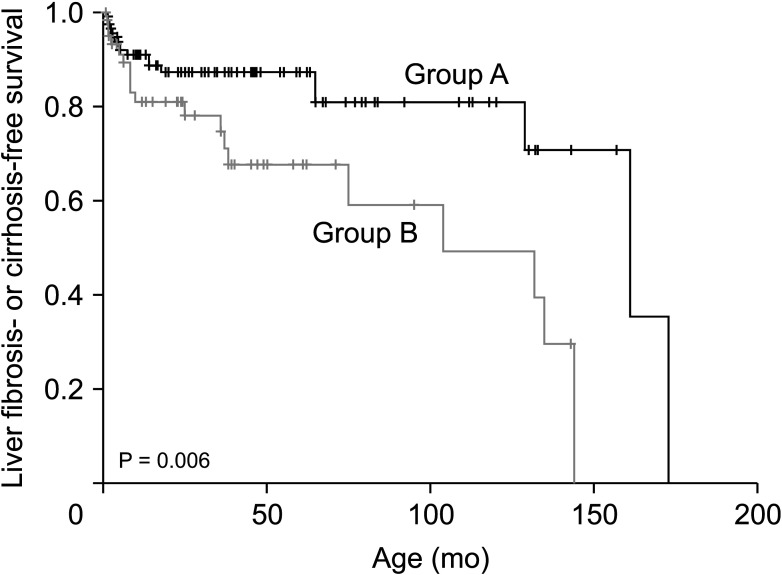
Fig. 2
Preoperative (A) and postoperative (B) magnetic resonance cholangiopancreatography images of a patient with intrahepatic bile duct (IHBD) dilatation. The images were gained on May 30, 2017 and May 12, 2020, respectively. The red arrowheads point to the IHBD.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download