Abstract
Purpose
Bilateral axillo-breast approach robotic parathyroidectomy (BABA-RP) aims to remove overactive or enlarged parathyroid glands with no visible neck collar incision. In this study, we compared the safety and surgical outcomes of BABA-RP vs. those of an open surgery group to ascertain whether BABA-RP is a safe and feasible surgical approach for patients with primary hyperparathyroidism (pHPT).
Methods
This single-institution retrospective cohort study included 74 patients with primary HPT who underwent open parathyroidectomy (n = 37) or BABA-RP (n = 37) at our institution between November 2014 and March 2023. Patient demographics, biochemical cure rates, operative time, blood loss rates, and complication rates were examined and compared.
Results
The patients in the BABA-RP group were younger and had a longer mean operative time. Regarding complication events, 2 patients in the open surgery group and 1 patient in the BABA-RP group had transient hypoparathyroidism. All 74 patients achieved biochemical cure at <6 months, regardless of the approach used. Two patients in the BABA-RP group and 1 patient in the open surgery group had carcinoma on surgical pathology. All 3 patients with parathyroid carcinoma remained recurrence-free at 1-year follow-up.
Primary hyperparathyroidism (pHPT) is a common endocrine disorder characterized by abnormal calcium metabolism, with an estimated incidence of 66 per 100,000 person-years for women and 25 per 100,000 person-years for men in the United States [1]. Parathyroidectomy is the definitive treatment for those with symptomatic kidney stones or fractures, calcium >1.0 mg/dL over the upper limit of normal, T-score <−2.5 on dual-energy X-ray absorptiometry, creatinine clearance <60 mL/min, 24-hour urinary calcium >400 mg/dL, urinary tract stones or vertebral fractures on imaging, and age <50 years [23].
Parathyroid surgery has evolved since it was first successfully performed by Mandl in 1925 [4]. Over the decades, the standard surgical approach was neck “collar” incision and bilateral neck exploration. However, after advances in parathyroid localization imaging and the high prevalence of single parathyroid adenoma (80%–90%), focused parathyroidectomy has become the standard procedure for pHPT, with results equivalent to those of bilateral cervical exploration [567].
More recently, a robotic scarless approach has been proposed and has become more popular in thyroid and parathyroid surgery because of its high-definition 3-dimensional (3D) videoscope, precise endowrist function instruments, and patient satisfaction regarding cosmetics. There are several approaches (transaxillary, bilateral axillo-breast, transoral, and retroauricular) to the thyroid and parathyroid glands in robotic surgery [8910111213].
Our institution is a considerably large-volume center for robotic thyroidectomy and uses the bilateral axillo-breast approach (BABA) [14]. The safety and feasibility of BABA robotic thyroidectomy have been well established since its first use by Youn et al. in 2008 [131516]. Considering the similarity in the surgical field between the thyroid and parathyroid glands, we did not encounter serious obstacles in starting robotic parathyroidectomy in 2014, and 37 patients with pHPT had undergone BABA robotic parathyroidectomy (BABA-RP) by April 2023.
This study aimed to compare the surgical outcomes of BABA-RP with those of focused open parathyroidectomy and to assess the safety and benefits of BABA-RP to determine whether BABA-RP is a safe and feasible surgical approach for pHPT.
The protocol of this study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (No. B-2312-872-102). This study was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
This was a retrospective comparative study. Patients were recruited between November 2014 and April 2023 from the Division of Endocrine Surgery, Department of Surgery, Seoul National University Bundang Hospital in South Korea. This institution performs approximately 40 parathyroidectomies annually. Thirty-seven consecutive open parathyroidectomies and 37 consecutive BABA-RPs were compared. All patients underwent surgery performed by 2 experienced surgeons, with a follow-up period of up to 6 months. The selection criteria were the same for both groups, as described below.
Seventy-four patients aged >18 years were recruited for this study. The patient demographics, body mass index (BMI), and operative indications are summarized in Table 1.
The inclusion criterion was single or multiple parathyroid tumors detected on imaging studies with a biochemical diagnosis of pHPT. The imaging modalities included neck sonography, parathyroid 4-dimensional CT, parathyroid technetium-99m sestamibi, and single photon emission CT (Fig. 1). All patients required surgical intervention because of age, hypercalcemia, hypercalciuria, osteoporosis, and history of urinary tract stones (Table 2).
Patients with concomitant thyroid cancer, a history of neck surgery, or an intraoperative parathyroid hormone (PTH) test during parathyroidectomy were excluded from this study. Those with familial hypocalciuric hypercalcemia were excluded based on 24-hour urine calcium levels.
The selection of the robotic vs. the conventional approach was based on patient preference. Both approaches were offered to all the patients. All parathyroidectomies were performed by 2 surgeons who had performed more than 200 parathyroidectomies.
The surgical approach has been described in detail in a previous publication [13]. It uses the Davinci Xi robotic system (Intuitive Surgical) via BABA to meticulously handle tissues and magnify the operational view. The BABA surgical procedure involved making 1 cm incisions on both axillae and both areolas of the breast and inserting all 8-mm ports. The grasper and bipolar dissector were inserted through the axillary ports, and a videoscope and harmonic scalpel (or electrocautery hook) were inserted through the breast ports (Fig. 2). After flap dissection around both sternocleidomastoid muscles and the anterior neck, surgeons meticulously dissected the lateral side of the thyroid gland and located the pathological parathyroid gland. Parathyroidectomy was performed under full visualization of the vessels around the parathyroid gland and recurrent laryngeal nerve (Fig. 3).
The techniques described by Udelsman and Donovan [5] or Agarwal et al. [7] were used. An abbreviated low collar incision was usually employed for a length of 3–4 cm for most cases. After limited subplatysmal flaps were developed, the strap muscles could be mobilized and retracted laterally to expose the thyroid glands. Previously localized parathyroid adenoma and recurrent laryngeal nerve were identified via dissecting between the lateral surface of the thyroid gland and strap muscles.
The success of parathyroidectomy was determined by biochemical normalization of serum calcium and PTH levels after surgery and by histopathological confirmation of proliferative parathyroid tissue in the excised lesion. Surgical outcomes were evaluated based on the surgical extent, operative time, blood loss, and hospital stay. Surgical complications, including postoperative hypoparathyroidism, hematoma, surgical site infection, and recurrent laryngeal nerve injury, were also evaluated. The follow-up period was up to 6 months after surgery.
The 2 groups were compared in terms of patient characteristics, surgical indications, operative findings, and surgical outcomes using the chi-square test (categorical variables) or Student t-test (continuous variables). Comparisons were performed using IBM SPSS Statistics ver. 21.0 (IBM Corp.). Statistical significance was set at P < 0.05.
Concerning patient characteristics, age was higher in the open surgery group (60.7 ± 12.14 years vs. 49.9 ± 13.48 years, P = 0.001). Sex (12 of 37 male vs. 11 of 37 male, P = 0.802) and BMI (24.14 ± 5.05 kg/m2
vs. 24.03 ± 3.22 kg/m2, P = 0.914) were not different between the 2 groups. In surgical indications, only osteoporosis (P = 0.03) and age (P = 0.04) were significantly more advanced in the open surgery group (Table 1).
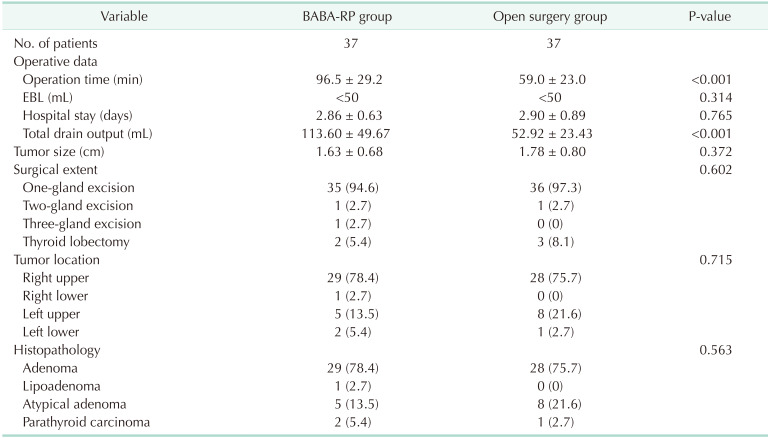
The mean operative time for the BABA-RP approach was 96.5± 29.2 minutes, whereas for the open approach, it was 59 ± 23 minutes (P < 0.001). The estimated blood loss was less than 50 mL in both groups (P = 0.314), and hospital stay was 2.86 ± 0.63 days for the BABA-RP group and 2.9 ± 0.89 days for the open surgery group (P = 0.765). Only the total drain output during hospital stay was different between the BABA-RP and open surgery groups (113.6 ± 49.67 mL vs. 59.9 ± 23.43 mL, P < 0.001) (Table 2).
There was no significant difference in the extent of surgery between the BABA-RP and open surgery groups (P = 0.602). Thirty-five patients had 1 gland excised, 1 underwent the excision of 2 glands, and another underwent the excision of 3 glands in the BABA-RP group. In the open surgery group, 36 patients had 1 gland excised and 1 patient had 2 glands excised. Two patients in the BABA-RP group and 3 patients in the open surgery group underwent concomitant ipsilateral thyroid lobectomy because of suspected parathyroid carcinoma or an intrathyroidal parathyroid gland (Table 2).
Tumor size (P = 0.372) and location (P = 0.715) were not significantly different between the BABA-RP and open surgery groups. The lower parathyroid glands were the dominant tumor location. Pathological parathyroid in the lower position was present in 29 of 37 patients (78.4%) in both groups. The mean tumor size was 1.63 ± 0.68 cm in the BABA-RP group and 1.78 ± 0.8 cm in the open surgery group.
Regarding the histopathological data, parathyroid adenoma was the most common disease in both groups (29 of 37 patients in the BABA-RP group vs. 28 of 37 patients in the open surgery group). The second most common pathology in each group was atypical adenoma (5 of 37 in the BABA-RP group vs. 8 of 37 in the open surgery group), and 1 patient in the BABA-RP group had lipoadenoma. Two patients in the BABA-RP group and 1 in the open surgery group had parathyroid carcinoma. All 3 patients with parathyroid carcinoma remained recurrence-free at the 1-year follow-up. The overall pathological difference between the 2 groups was negligible (P = 0.563) (Table 2).
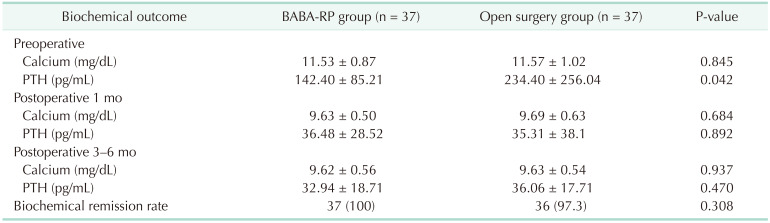
The mean postoperative biochemical data and remission rates are shown in Table 3. Immediate postoperative PTH and calcium levels normalized to 100% in the BABA-RP group (37 of 37) and 97% in the open surgery group (36 of 37). One patient in the open surgery group did not achieve biochemical remission and underwent a second operation 2 days after the first surgery. The preoperative PTH level was higher in the open surgery group because 1 patient with parathyroid carcinoma had a very high PTH level (1,444 pg/mL). Overall, the biochemical remission rate did not differ between the 2 groups (P = 0.308). The time trends of the mean serum calcium and PTH levels are shown in Fig. 4. The mean serum calcium and PTH levels were normal during the 1-month follow-up period. The final biochemical follow-up period was at 6 months.
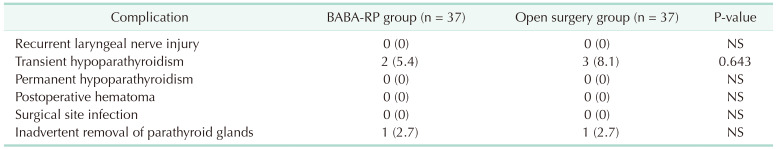
The most common complication was transient hypoparathyroidism, defined as hypocalcemic symptoms with postoperative day 1 PTH levels of <10.0 pg/mL. Two patients in the BABA-RP group (5.4%) and 3 patients in the open surgery group (8.1%) had transient hypoparathyroidism. Inadvertent removal of a normal parathyroid gland was also observed. Both groups had 1 patient (2.7%) with normal parathyroid gland removal due to preoperative imaging and operation-finding mismatch. No recurrent laryngeal nerve injuries, permanent hypoparathyroidism, postoperative hematomas, or surgical site infections were observed in either group (Table 4).
The Davinci robotic system has several advantages, such as multi-articulated movement, high-definition 3D views of small structures, and the ability to filter out vibrations caused by hand tremors. In addition to these benefits, the BABA robotic approach is even more optimized for parathyroid surgery by providing a symmetric surgical view of important neck structures such as the thyroidal vessels, parathyroid glands, and recurrent laryngeal nerves (Fig. 3). Thus, it is easier to perform bilateral neck exploration and parathyroidectomy using the BABA approach than the transaxillary approach [1213].
Demographic data analysis revealed that the BABA-RP group was younger than the open surgery group. This trend has a correlation with the difference in surgical indication data between 2 groups that more patients underwent open surgery because of age and osteoporotic factors (Table 1). This indicates that young patients are more concerned about the cosmetic results of surgery and are more likely to choose scarless surgery. The prospect of minimal scarring might be a decisive factor for younger patients when they are deciding surgical procedure.
Robotic parathyroidectomy usually takes longer than conventional open surgery because of the flap dissection and robotic arm docking, even when the learning curve is considered. The learning curve for robotic surgery has been well-described in other surgical fields [1718]. The BABA-RP group had a longer operative time and larger drain output (Table 2). This may imply that the wider flap dissection to create a working space in the BABA-RP group prolonged the operation time and increased drain output [15]. However, 12 patients in the open surgery group and 6 in the BABA-RP group had no drain insertion postoperatively. This might hinder a more accurate evaluation of drain output difference between the 2 groups.
In the biochemical remission data, 1 case of open parathyroidectomy failed to achieve immediate biochemical remission; the pathologic findings showed that the excised left lower gland was normal. After reoperation, the actual pathological gland was the left upper parathyroid gland. The risk of treatment failure or persistent hyperparathyroidism can be reduced by an intraoperative PTH assay, which is not routinely used for robotic patients at our institution [19]. We excluded patients who underwent intraoperative PTH assay during parathyroidectomy in the open surgery group because it could influence the comparison of surgical success between the BABA-RP and open surgery groups.
In the postoperative complication data, transient hypoparathyroidism was the only complication in each group. In this study, we defined transient hypoparathyroidism as hypocalcemic symptoms with a postoperative day 1 PTH levels of <10.0 pg/mL. Many studies have reported that postoperative PTH level is a better predictor of hypocalcemia than isolated calcium level, and a PTH level of <10 pg/mL is usually predictive for hypocalcemia and calcium medication [1920]. In our institution, calcium carbonate and alfacalcidol constitute a postoperative medication regimen, and we withdrew medication within 3 months if patients had no symptoms and had normal serum calcium and PTH results. If postoperative PTH is ≥10 pg/mL, we prescribe CaCO3 500 mg, 2 tablets 2 times per day and alfacalcidol 0.5 µg, 2 tablets per day. If PTH was <10 pg/mL, we prescribe CaCO3 500 mg, 2 tablets 4 times per day and alfacalcidol 0.5 µg, 2 tablets per day. Postoperative outpatient laboratory tests consisted of serum calcium, ionized calcium, phosphorus, and PTH levels.
Of the 37 BABA-RP patients in this study, 2 had multi-gland disease, and 2 had concomitant ipsilateral thyroid lobectomy due to suspected parathyroid carcinoma or intrathyroidal parathyroid gland. Considering the advantages of BABA, even if we encounter persistent hyperparathyroidism due to multi-gland disease during surgery or suspected parathyroid carcinoma, we may steadily proceed to additional neck exploration or thyroidectomy without converting to open maneuvers or adding incisions to the neck.
To the best of our knowledge, this is the first comparative study of BABA-RP with focused open parathyroidectomy and the first study of a relatively large number of robotic parathyroidectomies, which included more than 30 patients. The significant number of cases analyzed allows more accurate comparison and evaluation of the 2 procedures, which could lead to BABA-RP as a safe and feasible option for primary hyperparathyroidism patients.
However, this study has certain limitations. This was a retrospective, short-term follow-up study. In contrast to its known incidence, 3 parathyroid carcinomas were diagnosed in 74 patients with pHPT in this study. As parathyroid carcinoma is very rare and has a relatively high recurrence rate, a longer follow-up period is necessary to evaluate long-term surgical outcomes [2122]. Fortunately, inspection of electronic medical records revealed that all 3 patients were recurrence-free for at least 2 years after surgery.
The lack of patient-reported questionnaires for the BABA-RP due to the retrospective nature of the study is also a limitation. Nonetheless, in a study by Choe et al. [23], 76.5% and 20.6% of patients rated the cosmetic results of BABA thyroidectomy as “excellent” and “good,” respectively. From the results of this study, we can postulate that pHPT patients’ quality of life can be greatly improved not only by curing pHPT but also by improving cosmetic satisfaction with BABA-RP.
Cost is also a major concern for patients and healthcare institutions. The initial outlay (US $1.4 million), maintenance (US $15,000 per annum), and consumables (US $1,700 per case) costs are not affordable for every patient or hospital. Currently, robotic surgery is limited by high-cost manufacturers and the requirement for special training. These issues may preclude the widespread use of robotic surgery.
In conclusion, BABA robotic methods provide a good view of and approach to the bilateral neck during parathyroidectomy. This surgical technique is safe and feasible for patients undergoing pHPT.
Notes
References
1. Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013; 98:1122–1129. PMID: 23418315.
2. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016; 151:959–968. PMID: 27532368.
3. Zhu CY, Sturgeon C, Yeh MW. Diagnosis and management of primary hyperparathyroidism. JAMA. 2020; 323:1186–1187. PMID: 32031566.
4. Delbridge LW, Palazzo FF. First parathyroid surgeon: Sir John Bland-Sutton and the parathyroids. ANZ J Surg. 2007; 77:1058–1061. PMID: 17973666.
5. Udelsman R, Donovan PI. Open minimally invasive parathyroid surgery. World J Surg. 2004; 28:1224–1226. PMID: 15517494.
6. Russell C. Unilateral neck exploration for primary hyperparathyroidism. Surg Clin North Am. 2004; 84:705–716. PMID: 15145229.
7. Agarwal G, Barraclough BH, Reeve TS, Delbridge LW. Minimally invasive parathyroidectomy using the 'focused' lateral approach. II. Surgical technique. ANZ J Surg. 2002; 72:147–151. PMID: 12074068.
8. Kandil E, Attia AS, Hadedeya D, Shihabi A, Elnahla A. Robotic thyroidectomy: past, future, and current perspectives. Otolaryngol Clin North Am. 2020; 53:1031–1039. PMID: 33127039.
9. Kandil E, Hadedeya D, Shalaby M, Toraih E, Aparício D, Garstka M, et al. Robotic-assisted parathyroidectomy via transaxillary approach: feasibility and learning curves. Gland Surg. 2021; 10:953–960. PMID: 33842239.
10. Mohamed HE, Bhatia P, Aslam R, Moulthrop T, Kandil E. Robotic transaxillary and retroauricular parathyroid surgery. Gland Surg. 2015; 4:420–428. PMID: 26425455.
11. Tolley N, Arora A, Palazzo F, Garas G, Dhawan R, Cox J, et al. Robotic-assisted parathyroidectomy: a feasibility study. Otolaryngol Head Neck Surg. 2011; 144:859–866. PMID: 21546590.
12. He Q, Zhu J, Zhuang D, Fan Z. Robotic total parathyroidectomy by the axillo-bilateral-breast approach for secondary hyperparathyroidism: a feasibility study. J Laparoendosc Adv Surg Tech A. 2015; 25:311–313. PMID: 25760735.
13. Lee KE, Choi JY, Youn YK. Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech. 2011; 21:230–236. PMID: 21857470.
14. Kwak J, Yu HW, Ahn JH, Kim SJ, Chai YJ, Choi JY, et al. A time trend analysis of 5,000 robotic thyroidectomies via bilateral axillo-breast approach. World J Surg. 2023; 47:403–411. PMID: 36525062.
15. Lee KE, Rao J, Youn YK. Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech. 2009; 19:e71–e75. PMID: 19542833.
16. Choi JY, Yu HW, Bae IE, Kim JK, Seong CY, Yi JW, et al. Novel method to save the parathyroid gland during thyroidectomy: Subcapsular saline injection. Head Neck. 2018; 40:801–807. PMID: 29356201.
17. Soomro NA, Hashimoto DA, Porteous AJ, Ridley CJ, Marsh WJ, Ditto R, et al. Systematic review of learning curves in robot-assisted surgery. BJS Open. 2020; 4:27–44. PMID: 32011823.
18. Catchpole K, Perkins C, Bresee C, Solnik MJ, Sherman B, Fritch J, et al. Safety, efficiency and learning curves in robotic surgery: a human factors analysis. Surg Endosc. 2016; 30:3749–3761. PMID: 26675938.
19. Higgins KM, Mandell DL, Govindaraj S, Genden EM, Mechanick JI, Bergman DA, et al. The role of intraoperative rapid parathyroid hormone monitoring for predicting thyroidectomy-related hypocalcemia. Arch Otolaryngol Head Neck Surg. 2004; 130:63–67. PMID: 14732770.
20. Orloff LA, Wiseman SM, Bernet VJ, Fahey TJ, Shaha AR, Shindo ML, et al. American Thyroid Association statement on postoperative hypoparathyroidism: diagnosis, prevention, and management in adults. Thyroid. 2018; 28:830–841. PMID: 29848235.
21. Busaidy NL, Jimenez C, Habra MA, Schultz PN, El-Naggar AK, Clayman GL, et al. Parathyroid carcinoma: a 22-year experience. Head Neck. 2004; 26:716–726. PMID: 15287039.
22. Harari A, Waring A, Fernandez-Ranvier G, Hwang J, Suh I, Mitmaker E, et al. Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab. 2011; 96:3679–3686. PMID: 21937626.
23. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606. PMID: 17308853.
Fig. 1
Preoperative imaging studies of parathyroid tumor localization . Commonly used imaging modalities for localizing parathyroid tumors. (A) Sonographic findings of the left parathyroid tumor (arrow). (B) Parathyroid 4-dimensional CT of the left parathyroid tumor (arrow). (C) Technetium-99m sestamibi scan of the left parathyroid tumor (arrow). (D) Single photon emission CT image after technetium-99m sestamibi injection into the left parathyroid tumor (arrow).
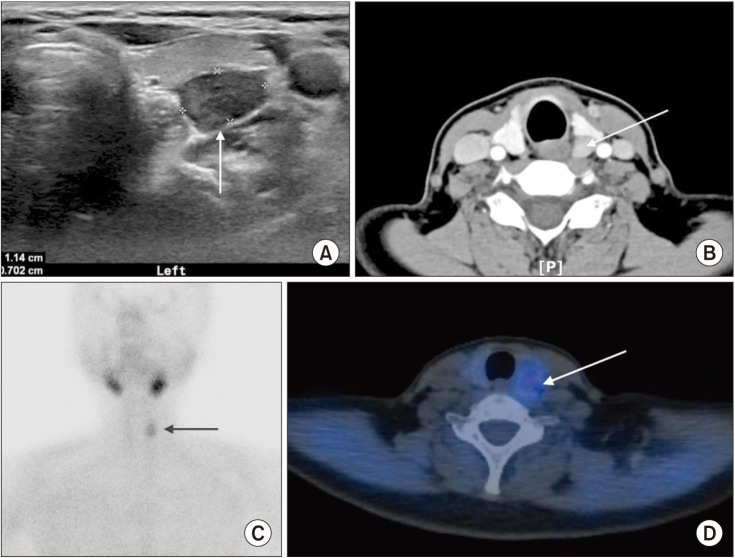
Fig. 2
Flap dissection area and trocar insertion sites of bilateral axillo-breast approach robotic parathyroidectomy. Two 8-mm ports were inserted through bilateral circumareolar incisions for the videoscope and electrocautery hook (or harmonic scalpel). Two 8-mm ports were inserted through the bilateral axillary incision for the Maryland Bipolar and Prograsp. Flap dissection around the sternocleidomastoid and anterior neck provided a working space.
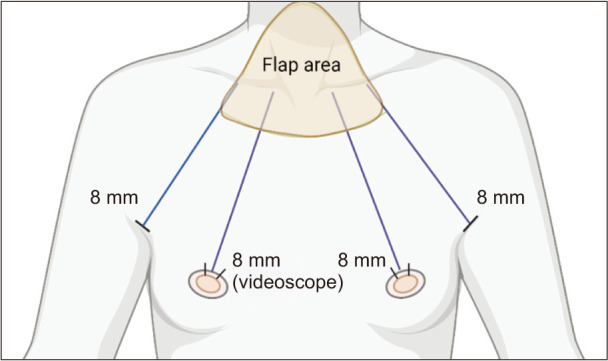
Fig. 3
Bilateral axillo-breast approach (BABA) robotic view of bilateral parathyroid tumor during BABA robotic parathyroidectomy. (A) BABA robotic view of the right parathyroid tumor (arrow). Asterisk, right thyroid gland. (B) BABA robotic view of the left parathyroid tumor (arrow). Asterisk, left thyroid gland. H, head direction; CCA, right common carotid artery; T, trachea; S, strap muscle.
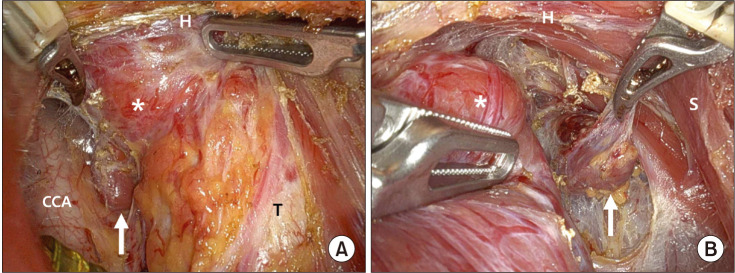
Fig. 4
Biochemical remission trend of the bilateral axillo-breast approach robotic parathyroidectomy (BABA-RP) and open parathyroidectomy groups during the 6-month follow-up. All patients in the BABA-RP (n = 37) and open surgery (n = 37) groups achieved biochemical remission at 1 month of follow-up, and no recurrence occurred during the 6-month follow-up. (A) Serum parathyroid hormone (PTH) level (normal range of serum PTH, 15–65 pg/mL). (B) Serum calcium level (normal range of serum calcium, 8.8–10.5 mg/dL).
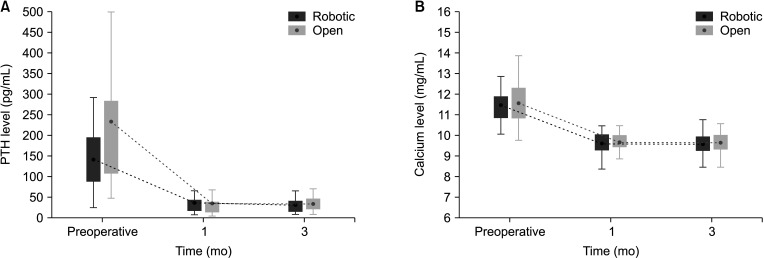
Table 1
Patient demographics and parathyroidectomy indications of 74 patients with primary hyperparathyroidism
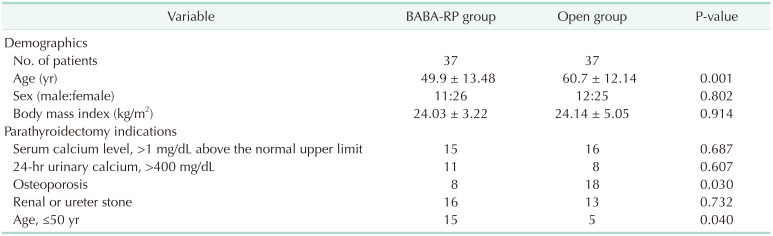
Table 2
Mean operative data, tumor characteristics, and histopathology of the 74 patients with primary hyperparathyroidism




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download