Abstract
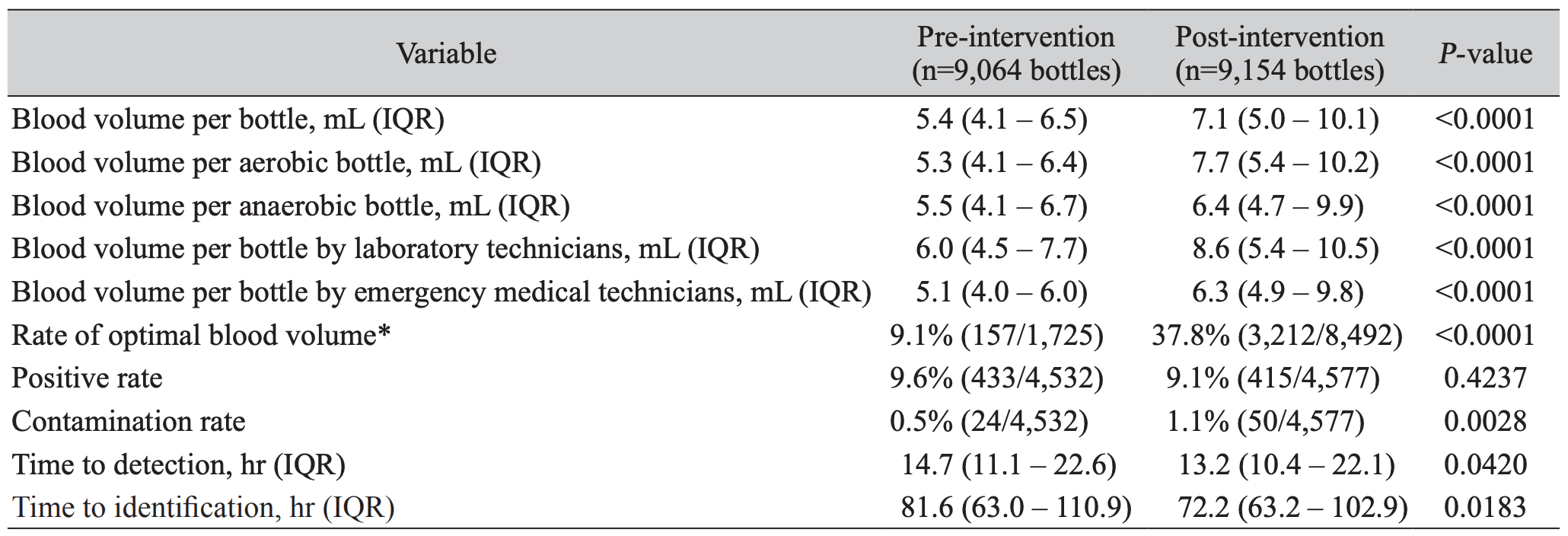
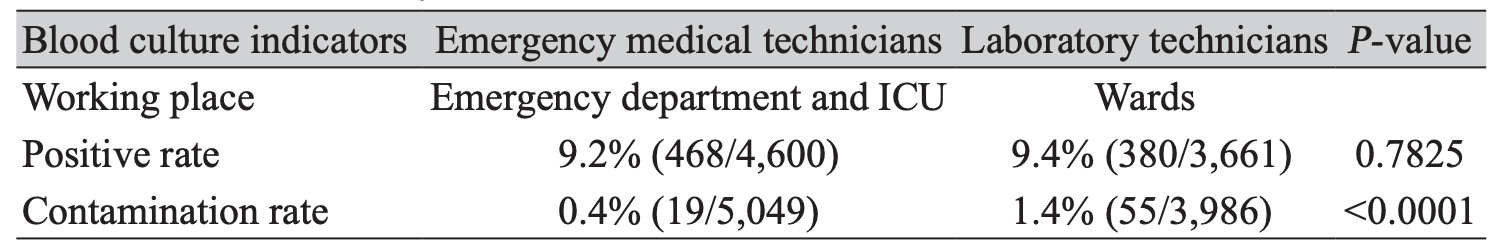
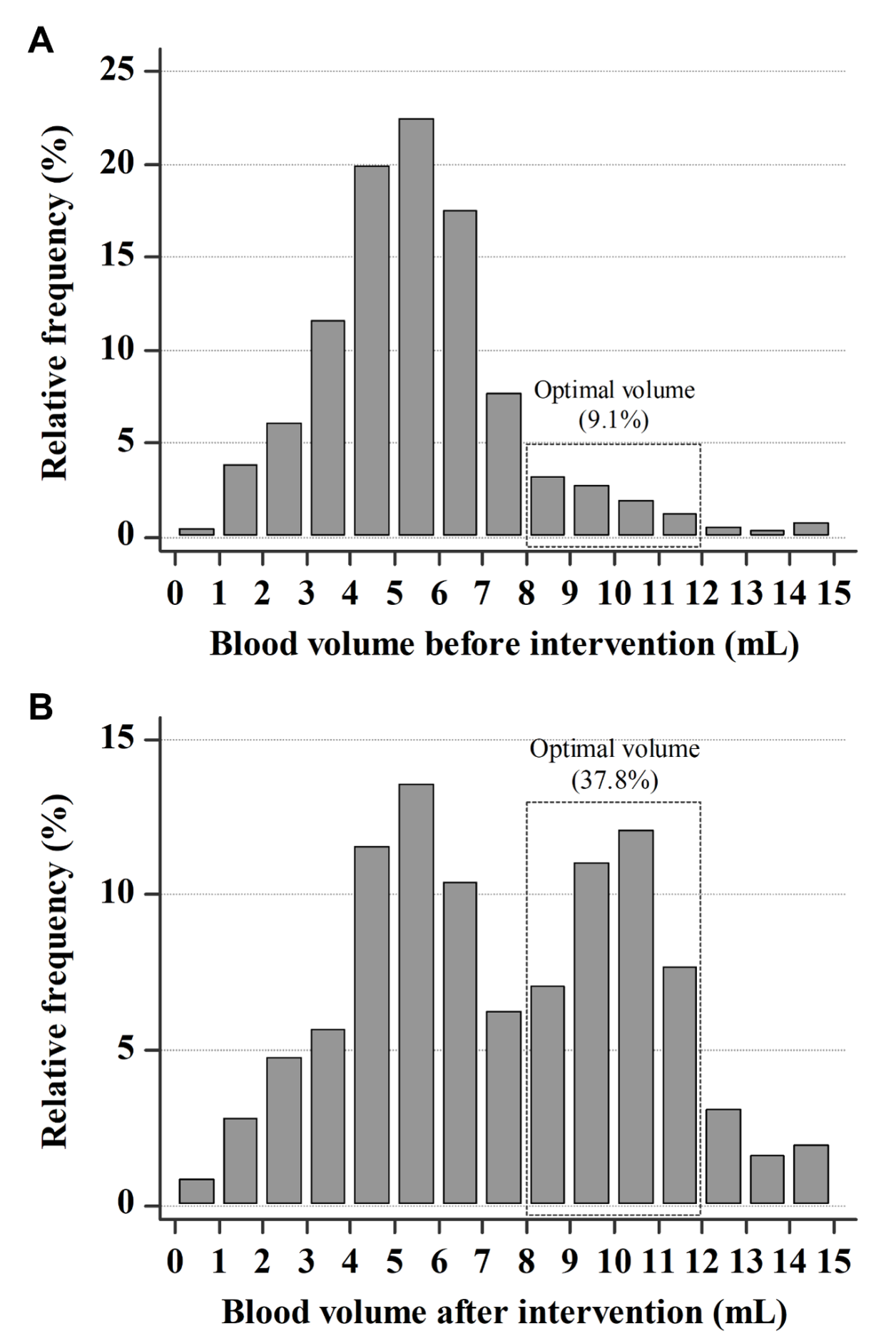
Background: Blood culture is essential for diagnosis of sepsis. However, usually the available blood volume is not sufficient to meet the guidelines. Thus, periodic monitoring and feedback are essential to improve the quality of blood cultures. Methods: We analyzed blood cultures requested between November 2018 and June 2019, and provided educational intervention and coaching for phlebotomists at the end of February 2019. Then, we evaluated the impact of education on blood cultures in a secondary‑care hospital. Blood volume, positive rate, contamination rate, and time to detection (TTD) were compared between the pre- (November 2018 to February, 2019) and post-intervention periods (March to June, 2019). Results: The average blood volume increased significantly from 5.4 mL to 7.1 mL (P < 0.0001) (35.2%) after intervention. Accordingly, the proportion of optimal blood volume (8–12 mL) increased from 9.1% to 37.8% (P < 0.0001). Before the intervention, the positivity rate was 9.6% and the contamination rate was 0.5%, whereas after the intervention, the positivity rate decreased to 9.1% and the contamination rate increased to 1.1%. TTD improved from 14.7 hours to 13.1 hours (P = 0.0420). Conclusion: The educational intervention of the phlebotomy team improved the quality of blood cultures, especially blood volumes and TTD. However, the positivity rate did not increase, suggesting that it is affected not only by the blood volumes but also by the severity of the underlying illnesses of the patient in a secondary-care hospital.
REFERENCES
1. Shin JH, Song SA, Kim MN, Lee NY, Kim EC, Kim S, et al. Comprehensive analysis of blood culture performed at nine university hospitals in Korea. Korean J Lab Med 2011;31:101-6.
2. Schifman RB, Strand CL. Blood culture contamination data analysis and critique. In: Q-Probes. Chicago: CAP 1995;1-19.
3. Clinical and Laboratory Standards Institute (CLSI). Principles and procedures for blood cultures; approved guideline. CLSI document M47-A. Wayne; PA: 2007.
4. Weinstein MP. Blood culture contamination: persisting problems and partial progress. J Clin Microbiol 2003;41:2275-8.
5. Hughes JA, Cabilan CJ, Williams J, Ray M, Coyer F. The effectiveness of interventions to reduce peripheral blood culture contamination in acute care: a systematic review protocol. Syst Rev 2018;7:216.
6. Kang H, Kim SC, Kim S. Comparison of chlorhexidine-alcohol and povidone-iodine for skin antisepsis and the effect of increased blood volume in blood culture. Korean J Clin Microbiol 2012;15:37-42.
7. Libertin CR, Sacco KA, Peterson JH. Education and coaching to optimise blood culture volumes: continuous quality improvement in microbiology. BMJ Open Qual 2018;7:e000228.
8. Lin HH, Liu YF, Tien N, Ho CM, Hsu LN, Lu JJ. Evaluation of the blood volume effect on the diagnosis of bacteremia in automated blood culture systems. J Microbiol Immunol Infect 2013;46:48-52.
9. Cockerill FR 3rd, Wilson JW, Vetter EA, Goodman KM, Torgerson CA, Harmsen WS, et al. Optimal testing parameters for blood cultures. Clin Infect Dis 2004;38:1724-30.
10. Koh EH, Kim S, Lee DH, Kim SC. Compliance with blood volumes collected for blood cultures between physicians and phlebotomists. Ann Clin Microbiol 2013;16:81-6.
11. Bae M, Kim HI, Park JH, Ryu BH, Chang J, Sung H, et al. Improvement of blood culture contamination rate, blood volume, and true positive rate after introducing a dedicated phlebotomy team. Eur J Clin Microbiol Infect Dis 2019;38:325-30.
12. Khare R, Kothari T, Castagnaro J, Hemmings B, Tso M, Juretschko S. Active monitoring and feedback to improve blood culture fill volumes and positivity across a large integrated health system. Clin Infect Dis 2020;70:262-8.
13. Bouza E, Sousa D, Rodriguez-Creixems M, Lechuz JG, Munoz P. Is the volume of blood cultured still a significant factor in the diagnosis of bloodstream infections? J Clin Microbiol 2007;45:2765-9.
14. Ramirez P, Gordon M, Cortes C, Villarreal E, Perez-Belles C, Robles C, et al. Blood culture contamination rate in an intensive care setting: effectiveness of an education-based intervention. Am J Infect Control 2015;43:844-7.
15. El Feghaly RE, Chatterjee J, Dowdy K, Stempak LM, Morgan S, Needham W, et al. A quality improvement initiative: reducing blood culture contamination in a children's hospital. Pediatrics 2018;142.
16. Choi ECE, Chia YH, Koh YQ, Lim CZQ, Lim JC, Ooi SBS, et al. Appropriateness of blood culture: a comparison of practices between the emergency department and general wards. Infect Dis Health 2019;24:49-55. .




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download