INTRODUCTION
MATERIALS AND METHODS
Subjects and study size
CBCT scan acquisition and image analysis
Inclusion and exclusion criteria
Morphological analysis and classification of tooth groups
-
1. MnSMs: According to the number of roots, this tooth group was divided into 1-, 2-, and 3-rooted teeth; 2- and 3-rooted teeth were named multi-rooted, and no further classification was made. Teeth with one root, i.e., a fused or non-divided root, were divided into the following subgroups (Figure 1) [2]:
C-shaped: Having a prominent radicular groove between the roots and exhibiting C1, C2, and C3 configurations in axial cross-section according to Fan classification [6].
Fused: Teeth that are simply notched without the presence of a distinct radicular groove between the roots.
Conical: A single, large, oval, or long oval configuration of the root canal system from the canal orifice to the root tip (C4 configuration).
-
2. Mandibular central and lateral incisors (Figure 2A) [913]:
-
3. MnCns (Figure 2B and 2C) [17]:
-
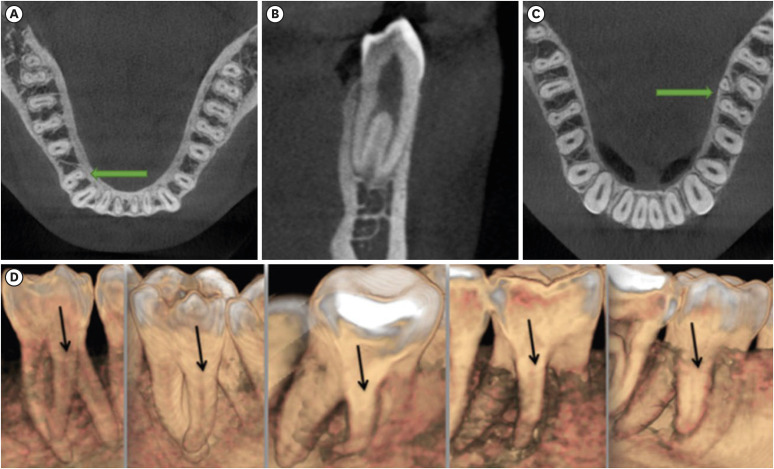
4. Mandibular premolars (Figure 3A and 3B) [8]:
5. MnFMs (Figure 3C and 3D) [8]: These teeth were categorized as 2-rooted and 3-rooted. Three-rooted teeth were considered to have a complicated root structure.
Figure 1
Examples of (A) 1-rooted, and (B) multi-rooted MnSM teeth and 1-rooted types, (C) C-shaped, (D) conical, (E) fused.
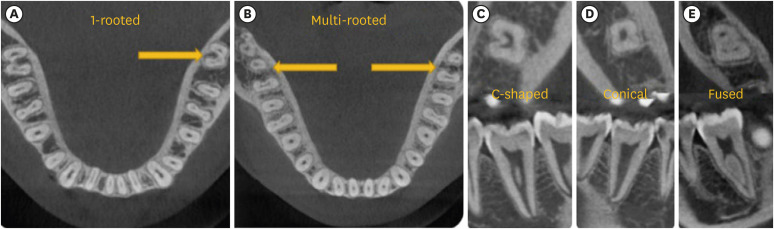
Figure 2
(A) Mandibular central and lateral incisors with complicated root canals, (B) 2-rooted mandibular canine, (C) 1-rooted/complicated canal mandibular canine.
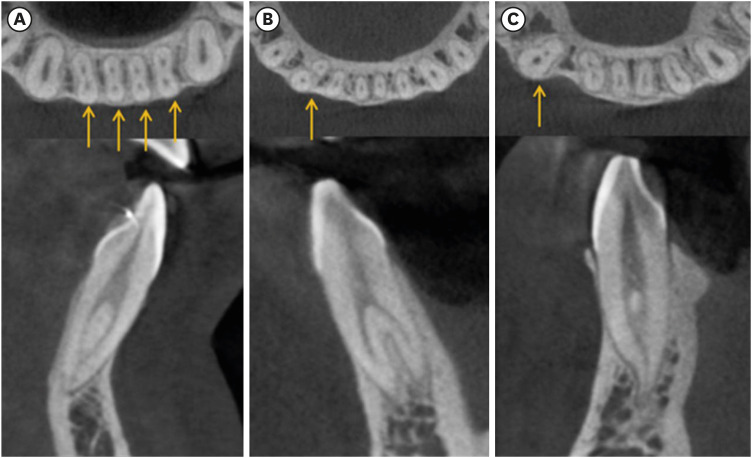
Figure 3
(A, B) Mandibular first premolar with complicated root canals, (C, D) examples of radix entomolaris in the mandibular first molar tooth.
Statistical analysis
RESULTS
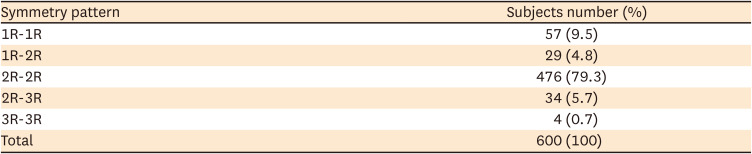
Root and root canal anatomies of MnSMs
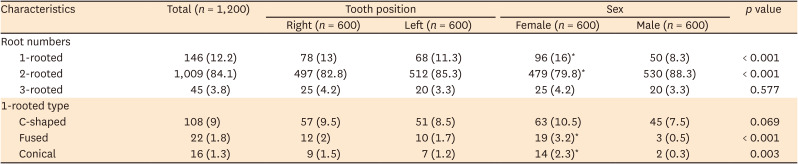
Table 1
Numbers and percentages of root numbers and 1-rooted types in mandibular second molars, and their distribution by tooth position and sex
Root and root canal anatomies of MnCI, MnLI, and MnCn teeth
Table 3
Distribution of mandibular central incisor (MnCI), mandibular lateral incisor (MnLI), mandibular canine (MnCn), mandibular first premolar (MnFP), mandibular second premolar (MnSP), and mandibular first molar (MnFM) teeth by number and percentage of root and canal types, tooth position, and sex
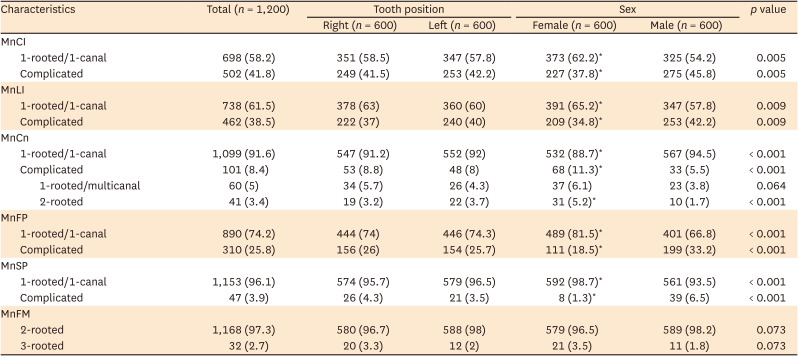
Root and root canal anatomies of mandibular premolars
Root numbers of MnFM teeth
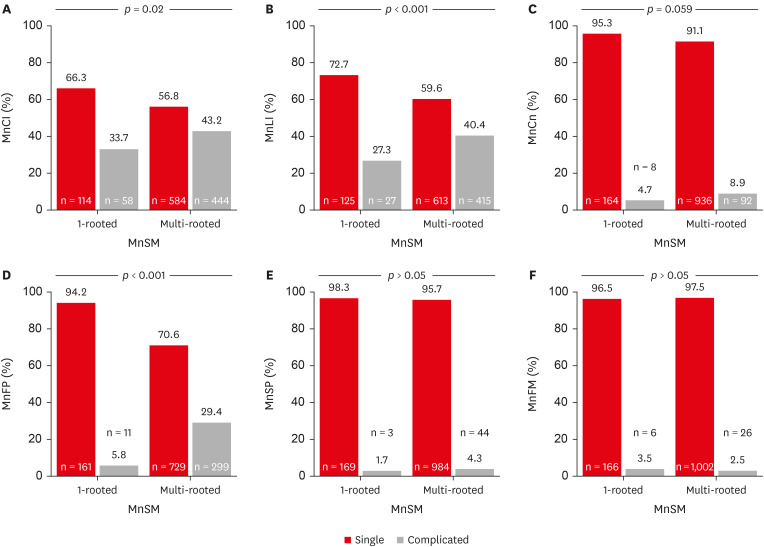
Differences in root and root canal anatomies in subjects with 1-rooted and multi-rooted MnSM teeth
Figure 4
In individuals with 1-rooted and multi-rooted mandibular second molar (MnSM) teeth, the number, percentages, and p values of the root anatomy of other teeth separately. (A) Mandibular central incisor (MnCI), (B) mandibular lateral incisor (MnLI), (C) mandibular canine (MnCn), (D) mandibular first premolar (MnFP), (E) mandibular second premolar (MnSP), (F) mandibular first molar (MnFM).
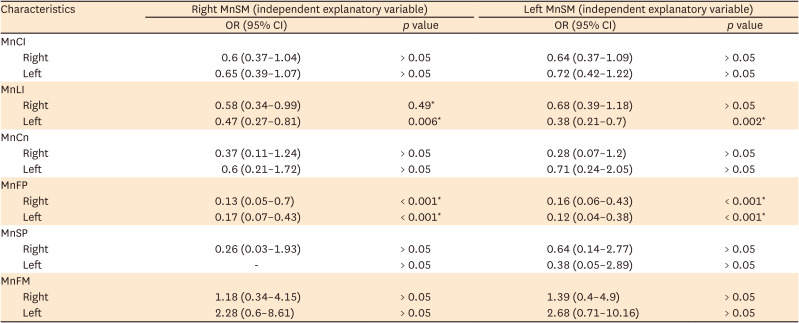
Predictive effects of root numbers of MnSM teeth on root-canal anatomy of other teeth
Table 4
Predictive effects of right and left mandibular second molars (MnSMs) with 1 root on complicated root and canal anatomy of other teeth, according to logistic regression analysis




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download