1. Patel S, Dawood A, Whaites E, Pitt Ford T. New dimensions in endodontic imaging: part 1. conventional and alternative radiographic systems. Int Endod J. 2009; 42:447–462. PMID:
19298577.
2. Jain S, Choudhary K, Nagi R, Shukla S, Kaur N, Grover D. New evolution of cone-beam computed tomography in dentistry: combining digital technologies. Imaging Sci Dent. 2019; 49:179–190. PMID:
31583200.
3. Patel S. New dimensions in endodontic imaging: part 2. cone beam computed tomography. Int Endod J. 2009; 42:463–475. PMID:
19298576.
4. Pauwels R, Araki K, Siewerdsen JH, Thongvigitmanee SS. Technical aspects of dental CBCT: state of the art. Dentomaxillofac Radiol. 2015; 44:20140224. PMID:
25263643.
5. Park JS, Chung MS, Park HS, Shin DS, Har DH, Cho ZH, et al. A proposal of new reference system for the standard axial, sagittal, coronal planes of brain based on the serially-sectioned images. J Korean Med Sci. 2010; 25:135–141. PMID:
20052359.
6. Uğur Aydin Z, Göller Bulut D. Determination of root canal length up to perforation area using different electronic apex locators and CBCT images obtained at different voxel sizes: a comparative
ex vivo study. Chin J Dent Res. 2021; 24:49–54. PMID:
33890455.
7. Scarfe WC. Cone beam computed tomography: volume acquisition. White SC, Pharoah MJ, editors. White and Pharoah’s oral radiology: principles and interpretation. 8th ed. Amsterdam: Elsevier Health Sciences;2014. p. 386–414.
8. Brüllmann D, Schulze RK. Spatial resolution in CBCT machines for dental/maxillofacial applications-what do we know today? Dentomaxillofac Radiol. 2015; 44:20140204. PMID:
25168812.
9. Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 120:508–512. PMID:
26346911.
10. Scarfe WC, Levin MD, Gane D, Farman AG. Use of cone beam computed tomography in endodontics. Int J Dent. 2009; 2009:634567. PMID:
20379362.
11. Metska ME, Aartman IH, Wesselink PR, Özok AR. Detection of vertical root fractures
in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod. 2012; 38:1344–1347. PMID:
22980175.
12. Tanimoto H, Arai Y. The effect of voxel size on image reconstruction in cone-beam computed tomography. Oral Radiol. 2009; 25:149–153.
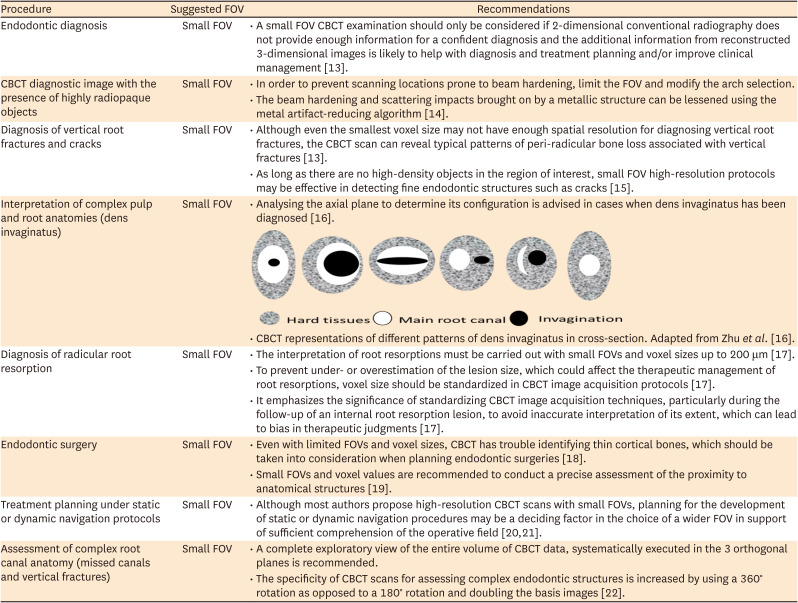
13. Patel S, Brown J, Semper M, Abella F, Mannocci F. European Society of Endodontology position statement: use of cone beam computed tomography in endodontics: European Society of Endodontology (ESE) developed by. Int Endod J. 2019; 52:1675–1678. PMID:
31301231.
14. Sinha A, Mishra A, Srivastava S, Sinha PM, Chaurasia A. Understanding artifacts in cone beam computed tomography. Int J Maxillofac Imaging. 2016; 2:51–53.
15. Pinto JC, de Faria Vasconcelos K, Leite AF, Wanderley VA, Pauwels R, Oliveira ML, et al. Image quality for visualization of cracks and fine endodontic structures using 10 CBCT devices with various scanning protocols and artefact conditions. Sci Rep. 2023; 13:4001. PMID:
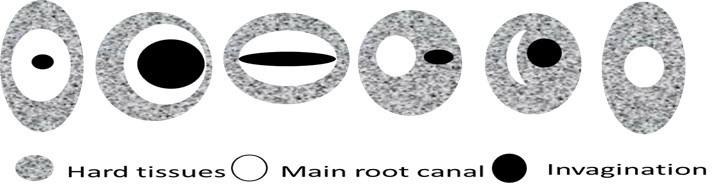
36899046.
16. Zhu J, Wang X, Fang Y, Von den Hoff JW, Meng L. An update on the diagnosis and treatment of dens invaginatus. Aust Dent J. 2017; 62:261–275. PMID:
28306163.
17. Da Silveira PF, Fontana MP, Oliveira HW, Vizzotto MB, Montagner F, Silveira HL, et al. CBCT-based volume of simulated root resorption - influence of FOV and voxel size. Int Endod J. 2015; 48:959–965. PMID:
25283786.
18. Pérez-Sánchez G, González-Torres M, Guzmán-Espinosa MA, Hernández-Vidal V, Teutle-Coyotecatl B, Mendoza-García LV, et al. Vestibular alveolar bone height measurement: accuracy and correlation between direct and indirect techniques. Acta Odontol Latinoam. 2020; 33:22–26. PMID:
32621595.
19. Strbac GD, Schnappauf A, Giannis K, Moritz A, Ulm C. Guided modern endodontic surgery: a novel approach for guided osteotomy and root resection. J Endod. 2017; 43:496–501. PMID:
28139285.
20. Mayo CV Jr, Replogle KJ, Marshall JG, Best AM, Sehgal HS, Sousa Melo SL, et al. Accuracy of presurgical limited field of view cone-beam computed tomography in predicting intraoperative buccal cortical bone. J Endod. 2020; 46:169–177.e1. PMID:
31839413.
21. Antal M, Nagy E, Sanyó L, Braunitzer G. Digitally planned root end surgery with static guide and custom trephine burs: a case report. Int J Med Robot. 2020; 16:e2115. PMID:
32304137.
22. Bechara B, McMahan CA, Nasseh I, Geha H, Hayek E, Khawam G, et al. Number of basis images effect on detection of root fractures in endodontically treated teeth using a cone beam computed tomography machine: an
in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115:676–681. PMID:
23601223.
23. ICRP. Rehani MM, Gupta R, Bartling S, Sharp GC, Pauwels R, et al. Radiological protection in cone beam computed tomography (CBCT). ICRP publication 129. Ann ICRP. 2015; 44:9–127. PMID:
26116562.
24. Kadesjö N, Lynds R, Nilsson M, Shi XQ. Radiation dose from X-ray examinations of impacted canines: cone beam CT vs two-dimensional imaging. Dentomaxillofac Radiol. 2018; 47:20170305. PMID:
29303367.
25. Ludlow JB, Timothy R, Walker C, Hunter R, Benavides E, Samuelson DB, et al. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 2015; 44:20140197. PMID:
25224586.
26. Patel S, Brown J, Pimentel T, Kelly RD, Abella F, Durack C. Cone beam computed tomography in endodontics - a review of the literature. Int Endod J. 2019; 52:1138–1152. PMID:
30868610.
27. Candemil AP, Salmon B, Vasconcelos KF, Oenning AC, Jacobs R, Freitas DQ, et al. Cone beam CT optimisation for detection of vertical root fracture with metal in the field of view or the exomass. Sci Rep. 2021; 11:19155. PMID:
34580339.
28. Van Acker JW, Pauwels NS, Cauwels RG, Rajasekharan S. Outcomes of different radioprotective precautions in children undergoing dental radiography: a systematic review. Eur Arch Paediatr Dent. 2020; 21:463–508. PMID:
32557182.
29. Gamache C, English JD, Salas-Lopez AM, Rong J, Akyalcin S. Assessment of image quality in maxillofacial cone-beam computed tomography imaging. Semin Orthod. 2015; 21:248–253.
30. Soares MR, Batista WO, Antonio PL, Caldas LV, Maia AF. Study of effective dose of various protocols in equipment cone beam CT. Appl Radiat Isot. 2015; 100:21–26. PMID:
25665897.
31. Lagos de Melo LP, Oenning AC, Nadaes MR, Nejaim Y, Neves FS, Oliveira ML, et al. Influence of acquisition parameters on the evaluation of mandibular third molars through cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017; 124:183–190. PMID:
28483471.
32. Goulston R, Davies J, Horner K, Murphy F. Dose optimization by altering the operating potential and tube current exposure time product in dental cone beam CT: a systematic review. Dentomaxillofac Radiol. 2016; 45:20150254. PMID:
26732433.
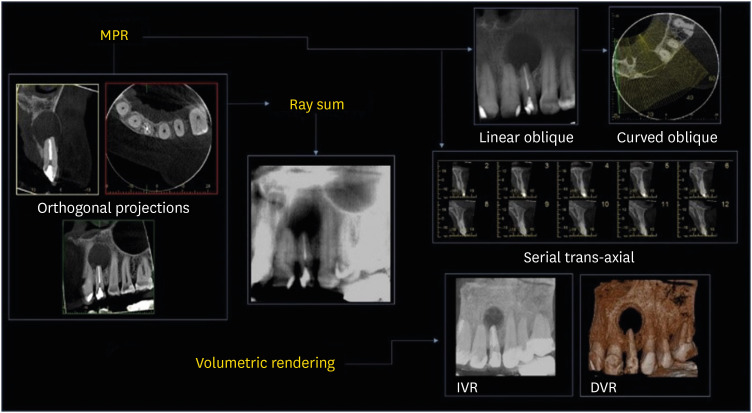
33. Scarfe WC, Li Z, Aboelmaaty W, Scott SA, Farman AG. Maxillofacial cone beam computed tomography: essence, elements and steps to interpretation. Aust Dent J. 2012; 57(Supplement 1):46–60. PMID:
22376097.
34. Durack C, Patel S. Cone beam computed tomography in endodontics. Braz Dent J. 2012; 23:179–191. PMID:
22814684.
35. Hoff MN, Zamora D, Spiekerman C, Aps JKM, Bollen AM, Herring SW, et al. Can cephalometric parameters be measured reproducibly using reduced-dose cone-beam computed tomography? J World Fed Orthod. 2019; 8:43–50.
36. Dillenseger JP, Gros CI, Sayeh A, Rasamimanana J, Lawniczak F, Leminor JM, et al. Image quality evaluation of small FOV and large FOV CBCT devices for oral and maxillofacial radiology. Dentomaxillofac Radiol. 2017; 46:20160285. PMID:
27580474.
37. Uysal S, Akcicek G, Yalcin ED, Tuncel B, Dural S. The influence of voxel size and artifact reduction on the detection of vertical root fracture in endodontically treated teeth. Acta Odontol Scand. 2021; 79:354–358. PMID:
33337942.
38. Liedke GS, da Silveira HE, da Silveira HL, Dutra V, de Figueiredo JA. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod. 2009; 35:233–235. PMID:
19166780.
39. BashizadehFakhar H, Bolhari B, Shamshiri A, Amini S, Ranji P. Diagnostic accuracy of cone-beam computed tomography at different tube voltages for vertical root fractures in endodontically treated teeth with metallic posts. Dent Hypotheses. 2021; 12:132–138.
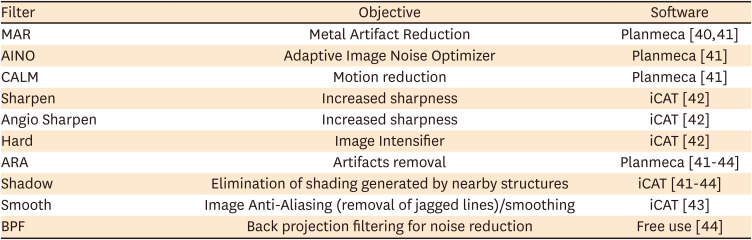
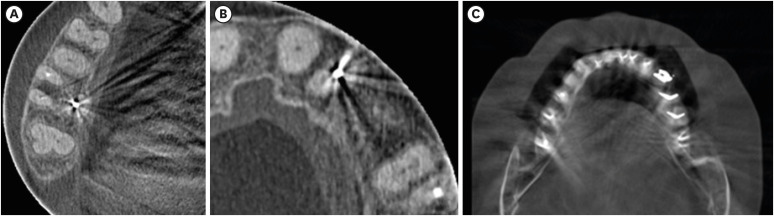
40. Bechara B, McMahan CA, Geha H, Noujeim M. Evaluation of a cone beam CT artefact reduction algorithm. Dentomaxillofac Radiol. 2012; 41:422–428. PMID:
22362221.
41. Bagis N, Kurt MH, Evli C, Camgoz M, Atakan C, Peker Ozturk H, et al. Evaluation of a metal artifact reduction algorithm and an adaptive image noise optimization filter in the estimation of peri-implant fenestration defects using cone beam computed tomography: an
in-vitro study. Oral Radiol. 2022; 38:325–335. PMID:
34387842.
42. Nascimento MC, Nejaim Y, de Almeida SM, Bóscolo FN, Haiter-Neto F, Sobrinho LC, et al. Influence of cone beam CT enhancement filters on diagnosis ability of longitudinal root fractures. Dentomaxillofac Radiol. 2014; 43:20130374. PMID:
24408819.
43. Verner FS, D’Addazio PS, Campos CN, Devito KL, Almeida SM, Junqueira RB. Influence of cone-beam computed tomography filters on diagnosis of simulated endodontic complications. Int Endod J. 2017; 50:1089–1096. PMID:
27977857.
44. Xia D, Cho S, Pan X. Backprojection-filtration reconstruction without invoking a spatially varying weighting factor. Med Phys. 2010; 37:1201–1209. PMID:
20384257.
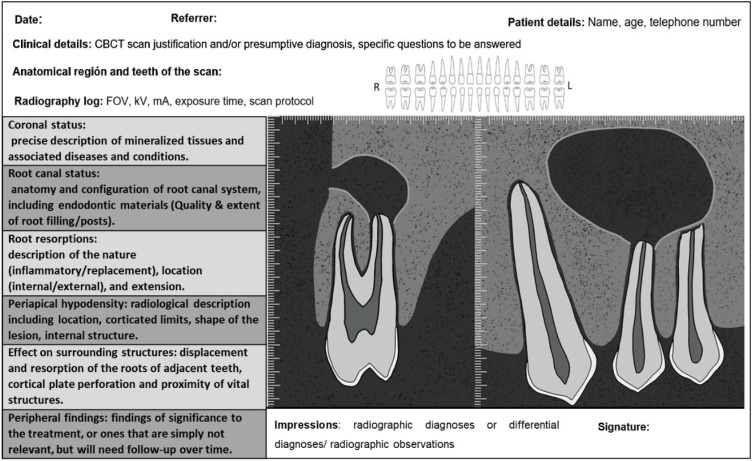
45. Patel S, Harvey S. Guidelines for reporting on CBCT scans. Int Endod J. 2021; 54:628–633. PMID:
33170952.
46. Moshfeghi M, Tavakoli MA, Ghaznavi D, Ghaznavi A. Effect of slice thickness on the accuracy of linear measurements made on cone beam computed tomography images. J Dent Sch. 2019; 34:100–108.
47. Pham VK, Pham TL. Root canal length estimated by cone-beam computed tomography at different slice thicknesses, dedicated endodontic software, or measured by an electronic apex locator. Sci Rep. 2022; 12:6531. PMID:
35444163.
48. Moudi E, Haghanifar S, Madani Z, Alhavaz A, Bijani A, Bagheri M. Assessment of vertical root fracture using cone-beam computed tomography. Imaging Sci Dent. 2014; 44:37–41. PMID:
24701457.
49. Patel S, Brady E, Wilson R, Brown J, Mannocci F. The detection of vertical root fractures in root filled teeth with periapical radiographs and CBCT scans. Int Endod J. 2013; 46:1140–1152. PMID:
23617242.
50. Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008; 52:707–730. PMID:
18805225.
51. Martins JN, Gu Y, Marques D, Francisco H, Caramês J. Differences on the root and root canal morphologies between Asian and White ethnic groups analyzed by cone-beam computed tomography. J Endod. 2018; 44:1096–1104. PMID:
29861062.
52. European Society of Radiology (ESR). Good practice for radiological reporting. Guidelines from the European Society of Radiology (ESR). Insights Imaging. 2011; 2:93–96. PMID:
22347937.
53. Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011; 40:265–273. PMID:
21697151.
54. Bidgood WD Jr, Horii SC, Prior FW, Van Syckle DE. Understanding and using DICOM, the data interchange standard for biomedical imaging. J Am Med Inform Assoc. 1997; 4:199–212. PMID:
9147339.
55. Rodrigues CT, Jacobs R, Vasconcelos KF, Lambrechts P, Rubira-Bullen IR, Gaêta-Araujo H, et al. Influence of CBCT-based volumetric distortion and beam hardening artefacts on the assessment of root canal filling quality in isthmus-containing molars. Dentomaxillofac Radiol. 2021; 50:20200503. PMID:
33400563.
56. Gregoris Rabelo LE, Bueno MD, Costa MV, de Musis CR, Estrela CR, Guedes OA, et al. Blooming artifact reduction using different cone-beam computed tomography software to analyze endodontically treated teeth with intracanal posts. Comput Biol Med. 2021; 136:104679. PMID:
34325229.
57. Spin-Neto R, Marcantonio E Jr, Gotfredsen E, Wenzel A. Exploring CBCT-based DICOM files. A systematic review on the properties of images used to evaluate maxillofacial bone grafts. J Digit Imaging. 2011; 24:959–966. PMID:
21448762.
58. Varma DR. Managing DICOM images: tips and tricks for the radiologist. Indian J Radiol Imaging. 2012; 22:4–13. PMID:
22623808.
59. Gibaud B. The DICOM standard: a brief overview. Lemoigne Y, Caner A, editors. Molecular imaging: computer reconstruction and practice. NATO science for peace and security series B: physics and biophysics. Berlin: Springer;2008. p. 229–238.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download