1. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020; 75:285–292. PMID:
31865786.
2. Ibrahim B, Jafari R. Cuffless blood pressure monitoring from a wristband with calibration-free algorithms for sensing location based on bio-impedance sensor array and autoencoder. Sci Rep. 2022; 12:319. PMID:
35013376.
3. Kario K, Shimada K, Pickering TG. Abnormal nocturnal blood pressure falls in elderly hypertension: clinical significance and determinants. J Cardiovasc Pharmacol. 2003; 41(Suppl 1):S61–S66. PMID:
12688399.
4. Kario K, Shimada K. Risers and extreme-dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens. 2004; 26:177–189. PMID:
15038628.
5. Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001; 38:852–857. PMID:
11641298.
6. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104. PMID:
30165516.
7. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:e13–115. PMID:
29133356.
8. Sherwood A, Hill LK, Blumenthal JA, Hinderliter AL. The effects of ambulatory blood pressure monitoring on sleep quality in men and women with hypertension: dipper vs. nondipper and race differences. Am J Hypertens. 2019; 32:54–60. PMID:
30204833.
9. Agarwal R, Light RP. The effect of measuring ambulatory blood pressure on nighttime sleep and daytime activity--implications for dipping. Clin J Am Soc Nephrol. 2010; 5:281–285. PMID:
20019118.
10. Davies RJ, Jenkins NE, Stradling JR. Effect of measuring ambulatory blood pressure on sleep and on blood pressure during sleep. BMJ. 1994; 308:820–823. PMID:
8167489.
11. Stergiou GS, Palatini P, Parati G, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021; 39:1293–1302. PMID:
33710173.
12. Teng X, Zhang YT. Proceedings of the 25th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (IEEE Cat. No.03CH37439). Piscataway (NJ): Institute of Electrical and Electronics Engineers;2003. p. 3153–3156.
13. Elgendi M, Fletcher R, Liang Y, et al. The use of photoplethysmography for assessing hypertension. NPJ Digit Med. 2019; 2:60. PMID:
31388564.
14. Stergiou GS, Mukkamala R, Avolio A, et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2022; 40:1449–1460. PMID:
35708294.
15. El-Hajj C, Kyriacou PA. A review of machine learning techniques in photoplethysmography for the non-invasive cuff-less measurement of blood pressure. Biomed Signal Process Control. 2020; 58:101870.
16. Stergiou GS, Avolio AP, Palatini P, et al. European Society of Hypertension recommendations for the validation of cuffless blood pressure measuring devices: European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2023; 41:2074–2087. PMID:
37303198.
17. Joung J, Jung CW, Lee HC, et al. Continuous cuffless blood pressure monitoring using photoplethysmography-based PPG2BP-net for high intrasubject blood pressure variations. Sci Rep. 2023; 13:8605. PMID:
37244974.
18. Charmoy A, Würzner G, Ruffieux C, et al. Reactive rise in blood pressure upon cuff inflation: cuff inflation at the arm causes a greater rise in pressure than at the wrist in hypertensive patients. Blood Press Monit. 2007; 12:275–280. PMID:
17890965.
19. International Organization for Standardization (ISO). ISO 81060-2:2018 Non-invasive sphygmomanometers—Part 2: Clinical investigation of intermittent automated measurement type. Geneva: International Organization for Standardization;2018.
20. Islam SM, Cartledge S, Karmakar C, et al. Validation and acceptability of a cuffless wrist-worn wearable blood pressure monitoring device among users and health care professionals: mixed methods study. JMIR Mhealth Uhealth. 2019; 7:e14706. PMID:
31628788.
21. Nachman D, Gilan A, Goldstein N, et al. Twenty-four-hour ambulatory blood pressure measurement using a novel noninvasive, cuffless, wireless device. Am J Hypertens. 2021; 34:1171–1180. PMID:
34143867.
22. Falter M, Scherrenberg M, Driesen K, et al. Smartwatch-based blood pressure measurement demonstrates insufficient accuracy. Front Cardiovasc Med. 2022; 9:958212. PMID:
35898281.
23. Sola J, Cortes M, Perruchoud D, et al. Guidance for the interpretation of continual cuffless blood pressure data for the diagnosis and management of hypertension. Front Med Technol. 2022; 4:899143. PMID:
35655524.
24. Tan I, Gnanenthiran SR, Chan J, et al. Evaluation of the ability of a commercially available cuffless wearable device to track blood pressure changes. J Hypertens. 2023; 41:1003–1010. PMID:
37016925.
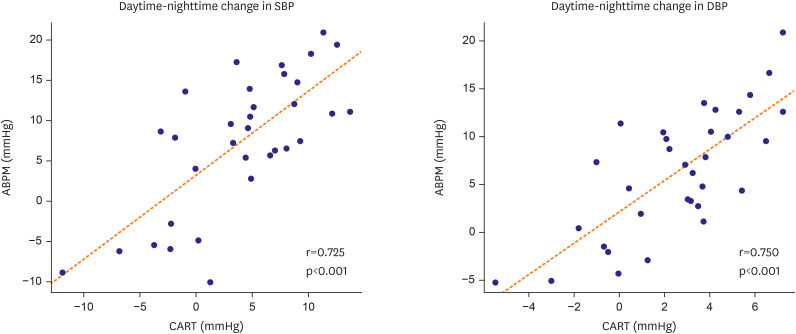
25. Park SW. Prospective, Single-center, Single group, Pivotal clinical trial to evaluate the blood pressure accuracy of ‘CART-I plus’ compared to the reference blood pressure reading with an auscultatory sphygmomanometer. J Korean Med Sci. 2024; [Epub ahead of print].
26. Nwankwo T, Coleman King SM, Ostchega Y, et al. Comparison of 3 devices for 24-hour ambulatory blood pressure monitoring in a nonclinical environment through a randomized trial. Am J Hypertens. 2020; 33:1021–1029. PMID:
32701144.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download