Abstract
Purpose
This study aims to investigate regional patterns and graft survival rates in kidney transplantation (KT) within South Korea using the National Health Insurance Service database.
Methods
By analyzing KT data from 2002 to 2017, including patient residency, KT location, and post-KT dialysis information, graft survival was assessed through post-KT dialysis and validated against Ulsan University Hospital and the Korean Organ Transplantation Registry’s 2017 report.
Results
Among the 20,978 KTs, 60.5% occurred in the Korean capital, Seoul, whereas 39.5% occurred outside. The overall graft survival rate was 81.5% with a median survival duration of 57 months. Patient survival was 83.8%, with a median survival duration of 61 months. For KTs from 2002 to 2007, the 10-year graft and patient survival rates were 89.1% and 90.3%, respectively. The KT recipients living outside Seoul who underwent the KT within their residential regions had a graft survival rate of 88.3%, and those receiving KTs outside their original region had a graft survival rate of 88.0%. Among Seoul residents who underwent KTs in the city, the graft survival rate was 90.5%. Importantly, hospital location did not significantly affect graft survival rates (P = 0.136).
Conclusion
This study revealed a regional preference for KT in South Korea, particularly in the capital city, likely because of nonresidents. Nevertheless, the graft and patient survival rates showed no significant regional disparities. These findings emphasize the necessity for equitable KT service access across regions in order to optimize patient outcomes.
Kidney transplantation (KT) is the most effective renal replacement therapy for patients with end-stage renal disease (ESRD) patients [1]. Since the first successful KT in 1969 [2], South Korea has performed over 2,000 KTs annually [3]. Transplant surgery requires extensive collaboration among medical departments and involves complex surgical and pharmacological treatments.
Despite South Korea’s compulsory national health insurance system, medical resources remain heavily concentrated in Seoul. The healthcare delivery system in South Korea underwent a significant shift with the introduction of nationwide health insurance in July 1989, marked by the implementation of a patient referral system [45]. However, the effectiveness of this system is low as it has only shown short-term effects [6], leading to the concentration of patients in large hospitals within the capital area [78]. A major concern in the medical delivery system is people’s preference for large metropolitan hospitals, which leads to a lower preference for local and medium-sized hospitals [9]. Despite government efforts to address this issue, the number of patients from nonmetropolitan areas seeking treatment in Seoul’s tertiary general hospitals continues to increase [10]. It has been noted that in Seoul’s top 5 hospitals, outpatient and inpatient visits have significantly increased, indicating a growing reliance on medical care in high-level general hospitals within the metropolitan region [11].
Prior research has analyzed graft survival in KT using Korean Network for Organ Sharing (KONOS) data in South Korea and compared graft survival rates across different regions [3]. This study aimed to examine the nationwide distribution of KT since 2002, focusing on the concentration of KT cases in the metropolitan areas, and to investigate potential differences in graft survival rates by region and between residents and nonresidents.
This study was approved by the Institutional Review Board of the Ulsan University Hospital in Ulsan, Korea (No. UUH-2019-04-005-002). It was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
In South Korea, the National Health Insurance Service (NHIS) is a compulsory social insurance that covers the entire Korean population. All healthcare providers in the country are legally required to participate in this system and provide medical services on a fee-for-service basis. The NHIS database includes medical claims for the entire population covered under NHIS [4].
We requested customized health information data from the NHIS and were granted data access permission for a limited duration to obtain edited data from the Big Data Analysis Center of NHIS for the purposes of our study.
To compile our dataset, we extracted specific data elements of sex, age, operation date, and patient identifiers from the edited database. Patients’ regions of residence and the locations of the hospitals where their KTs were conducted at the time of transplantation were also collected.
Thus, nearly all KT procedures performed in South Korea during the study period were included. Additionally, specific information about concomitant medications (immunosuppressants, dialysis solutions) and procedures was identified using codes from the NHIS database. Medication codes of dialysis solution were shown in Supplementary Material 1.
The cases included in this study were patients who underwent KTs between 2002 and 2017 and were identified using the NHIS procedure code R3280 (Renal Transplantation). We assumed that these patients had no history of KT before 2002 and underwent only 1 KT during the study period. In cases where patients underwent multiple KTs within the study period, only their first known KT was analyzed as an index KT, and the others were excluded as the next KT indicating graft failure of the index KT.
To analyze the correlation between patients’ residences and the hospitals where they underwent KT, we focused on the major metropolitan cities for this study (Seoul, Incheon, Daejeon, Gwangju, Daegu, Busan, and Ulsan).
Specifically, when examining the correlation between the patients’ residence and the hospitals' location for the KT, those who had the transplant at a hospital in their own region were labeled as within, while those who underwent the transplant at a hospital outside their region were labeled as beyond.
The primary endpoint of this study was graft failure after the index KT hospitalization. Graft failure was defined in 2 scenarios: the first was when the second KT replaced the first KT, and the second was when consecutive post-KT dialyses lasted for more than 12 months. Post-KT dialysis includes all types of dialysis, such as hemodialysis and peritoneal dialysis, performed the month after KT. Multiple dialyses were considered consecutive if they occurred within 3 months of the first postoperative dialysis. Hemodialysis was identified using the procedure codes for hemodialysis in the NHIS database, whereas peritoneal dialysis was identified using the medication codes for the dialysis solution in the NHIS database. The secondary endpoint of this study was all-cause mortality after discharge following the index KT hospitalization, which was identified using NHIS data indicating the date of death. The 10-year graft and patient survival rates were calculated using the NHIS data from 2002 to 2007.
Baseline patient characteristics are presented as either mean ± standard deviation for continuous variables or frequency (%) for categorical variables. Continuous variables were compared between the case and control groups using the Student t-test. Categorical data were compared using the chi-square test. The cumulative survival rates for clinical outcomes between the case and control groups were estimated using the Kaplan-Meier method and compared using the log-rank test. All statistical analyses were conducted using SAS software ver. 9.4 (SAS Institute), and a P-value of <0.05 was considered statistically significant.
To ensure the accuracy of the NHIS data, we collected KT data from Ulsan University Hospital, which is the only hospital in Ulsan city that performs KT surgeries. We compared the sex, age, and graft survival of KT patients between 2002 and 2017 with the results obtained from the NHIS data. Additionally, we cross-referenced our NHIS results for kidney graft survival with a 2017 report from the Korean Organ Transplantation Registry (KOTRY, https://www.kotry.org).
Between 2002 and 2017, 20,978 KT cases involving 20,717 patients were reported in South Korea. The mean age of patients was 45.9 ± 12.66 for 12,305 male patients (59.4%) and 44.9 ± 12.25 for 8,413 female patients (40.6%). The overall graft survival rate was 81.5% for a median duration of 57 months, with a mean duration of 65.9 ± 49.0 months. The overall patient survival rate was 83.8% for a median duration of 61 months, with a mean duration of 69.1 ± 50.3 months, from 2002 to 2017.
During the same period, major metropolitan cities and districts in South Korea witnessed the collective performance of KTs, as shown in Table 1 and Fig. 1. Notably, a substantial majority of KTs, totaling 60.5% (12,688 cases), were conducted in Seoul, while the remaining 39.5% (8,290 cases) occurred in regions outside Seoul. Upon considering population ratios, Seoul emerged as a standout performer in KTs, conducting 3.24 times more procedures than its metropolitan counterparts (Table 1, Fig. 1).
The frequencies of KTs per million people, stratified by hospital region and patient residence, are shown in Fig. 2. Notably, Seoul (1,304.01), Busan (639.30), and Daegu (714.75) recorded the highest KT rates per million people, exceeding the national average of 404.59. Conversely, all the other regions exhibited lower rates. Outside Seoul, Busan, and Daegu, fewer than 70% of patients underwent KT within their residential areas. Notably, more than 50% of the patients who did not receive KT within their residential region chose to undergo the surgery in hospitals located in Seoul. It is noteworthy that no hospitals performed KTs in Jeonnam, Gyeongbuk, or Sejong (Sejong was established as a new city in 2012). The relationship between the patient’s place of residence and the KT hospital region is depicted in Supplementary Fig. 1.
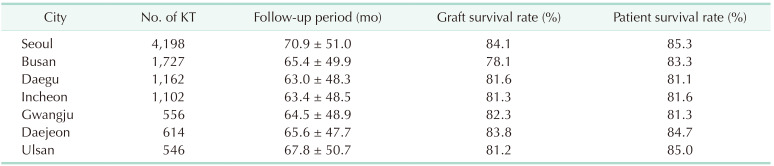
The graft and patient survival rates after KT among residents of major metropolitan cities in South Korea during the study period from 2002 to 2017 are presented. Specifically, graft survival rates in Seoul, Busan, Daegu, and Incheon were 84.1%, 78.1%, 81.6%, and 81.3%, respectively. Correspondingly, the patient survival rates in these cities were 85.3%, 83.3%, 81.1%, and 81.6%, respectively (Table 2).
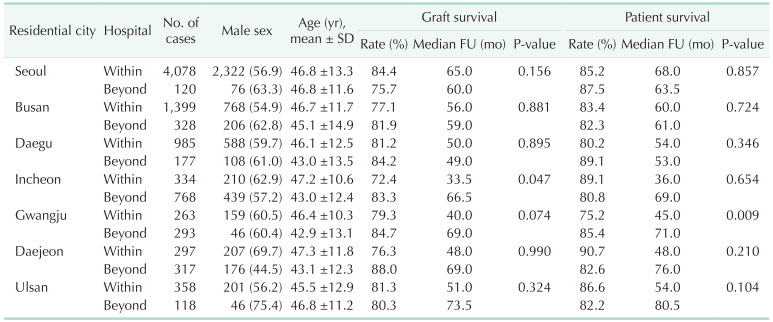
The graft and patient survival rates of KT recipients who underwent transplantation either within or outside their residential areas in major metropolitan cities in South Korea are presented in Table 3. Remarkably, except for Gwangju, no noteworthy differences were observed in graft and patient survival rates between the 2 groups across most major cities (Table 3).
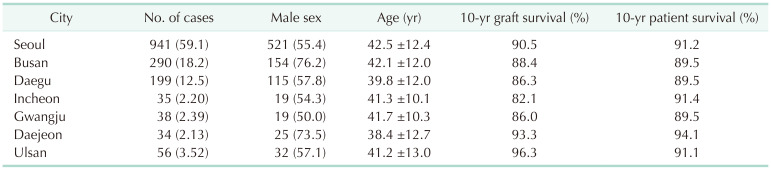
Between 2002 and 2007, South Korea performed 4,167 KTs, with 10-year graft and patient survival rates of 89.1% and 90.3%, respectively. Table 4 presents the 10-year graft and patient survival rates for individuals who resided in and underwent KT within the same region, covering 7 major cities. These results are consistent with the overall graft and patient survival rates observed in South Korea.
It was found that the 10-year graft survival rate was not significantly different between patients who underwent KT in their residential areas and those outside their residential areas (89.6% vs. 91.8%, P = 0.1532) (Fig. 3B). Furthermore, among the patients living outside Seoul, those who underwent KT within their residential region demonstrated a graft survival rate of 88.3%, whereas those who underwent KTs outside their original region exhibited a graft survival rate of 88.0%. Among patients residing in Seoul who underwent KT within the city, the graft survival rate was 90.5%. Notably, there was no statistically significant variation in the graft survival rate based on the location of the hospital where KT was performed (P = 0.136) (Fig. 3C).
This study is the first to offer comprehensive insights into KT outcomes across South Korea over the past decade. The utilization of the NHIS database, which covers the entire Korean population, ensured the accuracy and precision of our evaluation. The extended tracking of recipients of KT enabled effective assessment of graft survival rates. Furthermore, we validated the accuracy of the NHIS database by cross-referencing KT survival data with our Ulsan University Hospital database and the 2017 KOTRY report and confirmed the concurrence of graft and patient survival rates using both KT counts and postoperative dialysis information.
Our study revealed that the overall graft and patient survival rates for KTs in South Korea were 81.5% and 83.8%, respectively. Focusing on KTs conducted between 2002 and 2007, we observed 10-year graft and patient survival rates of 89.1% and 90.3%, respectively. Contrastingly, Ahn et al. [2] investigated the 1- and 3-year survival rates based on the KOTRY database in 2009 and 2010 and reported 98.9% and 96.0% overall survival rates at 1 and 3 years, respectively, along with corresponding graft survival rates of 98.6% and 93.7%, respectively. Additionally, Wang et al. [12] reported allograft survival rates of KTs performed in 2014 in different countries. In the United States, the 5-year survival rates for living- and deceased-donor KTs are 84.6% and 72.4%, respectively, whereas in Australia, New Zealand, Europe, and Canada, these rates range from 81% to 90%. Our study holds significance as it provides long-term national KT outcomes, enabling valuable comparisons with global results [212131415].
Our study showed that a significant majority of the patients who underwent KT outside their local areas preferred hospitals in the capital region. This preference likely arises from the belief that larger metropolitan hospitals offer a higher level of expertise among surgeons, more extensive medical staff, and enhanced services than smaller healthcare facilities [1016]. This expectation has led to the anticipation of improved KT outcomes in metropolitan hospitals. Notably, even after enduring waiting periods of 2–3 months, a substantial proportion of patients within South Korea’s larger hospitals still faced further prolonged waiting times before receiving KT [16]. The concentration of patients within these major medical centers may be attributed to a lack of well-informed decision-making or misguided selection processes [1718]. Disseminating precise and up-to-date information could potentially alleviate the issue of overpopulation of KT patients in larger medical facilities [1920].
Thus, KT recipients are required to regularly visit outpatient clinics before and after surgical procedures. Additionally, it was found that these patients often seek care in the emergency room because of acute complications. Research conducted in the United States revealed that the cumulative incidences of emergency department visits for KT patients reached 57% within 24 months, with nearly half of these visits resulting in hospital admissions [21]. In 2016, the Korean government allocated over 50 million US dollars to support approximately 2 thousand recipients, highlighting the rising economic expenses associated with transplantation [22]. Transitioning to a nonresidential area may introduce delays in accessing timely treatment during instances of acute complications, subsequently leading to increased time constraints and financial burden.
A significant aspect of our study was the examination of the regional disparities in KT graft survival. Surprisingly, we found no substantial differences in the graft and patient survival rates when comparing metropolitan cities or when distinguishing between transplants performed within and outside the recipients’ residential areas. However, an intriguing trend has emerged concerning the concentration of KT cases in the capital city, often due to nonresidents seeking KTs. Our study also revealed that >50% of patients who did not undergo KT locally opted for surgery within the capital region. Remarkably, despite this trend, there were no significant regional disparities in ESRD incidence or deceased donor KT rates. This finding is supported by the 2019 statistics from KONOS [3].
Although this study’s retrospective design based on the extensive NHIS dataset yielded valuable insights, certain critical details that could influence clinical outcomes, such as preemptive treatment status, donor status (deceased or living), human leukocyte antigen matching status, and ABO-incompatible status, were unavailable within the health insurance database. Future studies that incorporate regional variations in these factors could offer a deeper understanding of their potential impact on KT outcomes.
In our study, the high incidence of KT in Seoul was primarily due to nonresidents seeking treatment in the capital city. Along with surgery, posttransplant care, including immunosuppressive agents, is crucial for addressing potential complications. Surprisingly, our study revealed no significant differences in graft and patient survival between Seoul and other major metropolitan cities.
To improve patient convenience and accessibility to posttransplant care, facilitating transplants closer to patients’ homes would be a more efficient way to get positive outcomes. In Korea, given the mandatory enrollment of all citizens in medical insurance, the government should undertake this responsibility.
Thus, our study provides a comprehensive overview of national KT outcomes in South Korea over an extended period. Overall, the graft and patient survival rates were promising, with no significant regional disparities. However, the preference for KT in the capital city, driven by nonresident patients, highlights the need for equitable resource distribution and warrants careful consideration.
Notes
References
1. Garcia GG, Harden P, Chapman J. World Kidney Day Steering Committee 2012. The global role of kidney transplantation. Lancet. 2012; 379:e36–e38. PMID: 22405254.

2. Ahn C, Koo TY, Jeong JC, Kim M, Yang J, Lee J, et al. Initial report of the Korean Organ Transplant Registry: the first report of national kidney transplantation data. Transplant Proc. 2014; 46:425–430. PMID: 24655980.

3. Korean Network for Organ Sharing (KONOS). 2019 Annual report on organ transplants and human tissue donation [Internet]. KONOS;2019. cited 2023 Aug 26. Available from: https://www.konos.go.kr/board/boardListPage.do?page=sub4_2_1&boardId=30.
4. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab J. 2014; 38:395–403. PMID: 25349827.

5. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009; 24:63–71. PMID: 19004861.

6. Ock M, Kim JE, Jo MW, Lee HJ, Kim HJ, Lee JY. Perceptions of primary care in Korea: a comparison of patient and physician focus group discussions. BMC Fam Pract. 2014; 15:178. PMID: 25358391.

7. Lee JY, Jo MW, Yoo WS, Kim HJ, Eun SJ. Evidence of a broken healthcare delivery system in Korea: unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J Korean Med Sci. 2014; 29:1590–1596. PMID: 25469056.

8. Lim B. Korean medicine coverage in the National Health Insurance in Korea: present situation and critical issues. Integr Med Res. 2013; 2:81–88. PMID: 28664058.

10. Kim AM, Cho S, Kim HJ, Jung H, Jo MW, Lee JY, et al. Primary care patients' preference for hospitals over clinics in Korea. Int J Environ Res Public Health. 2018; 15:1119. PMID: 29848995.

11. Shin JH. Continued increase in patients from regions seeking major general hospitals in Seoul and metropolitan areas [Internet]. Dailymedi;2021. 10. 01. cited 2023 Aug 26. Available from: https://www.dailymedi.com/news/news_view.php?wr_id=874820.
12. Wang JH, Skeans MA, Israni AK. Current status of kidney transplant outcomes: dying to survive. Adv Chronic Kidney Dis. 2016; 23:281–286. PMID: 27742381.

13. Mudiayi D, Shojai S, Okpechi I, Christie EA, Wen K, Kamaleldin M, et al. Global estimates of capacity for kidney transplantation in world countries and regions. Transplantation. 2022; 106:1113–1122. PMID: 34495014.

14. Ojo AO, Morales JM, González-Molina M, Steffick DE, Luan FL, Merion RM, et al. Comparison of the long-term outcomes of kidney transplantation: USA versus Spain. Nephrol Dial Transplant. 2013; 28:213–220. PMID: 22759384.

15. Merion RM, Goodrich NP, Johnson RJ, McDonald SP, Russ GR, Gillespie BW, et al. Kidney transplant graft outcomes in 379 257 recipients on 3 continents. Am J Transplant. 2018; 18:1914–1923. PMID: 29573328.

16. Chong HJ, Kim HK, Kim SR, Lee S. Waiting for a kidney transplant: the experience of patients with end-stage renal disease in South Korea. J Clin Nurs. 2016; 25:930–939. PMID: 26994991.

17. Christiansen T, Vrangbæk K. Hospital centralization and performance in Denmark: ten years on. Health Policy. 2018; 122:321–328. PMID: 29475739.

18. Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K, et al. Toward a consensus on centralization in surgery. Ann Surg. 2018; 268:712–724. PMID: 30169394.

19. Hong du P, Song J. The effective distribution system for the concentration of patients to extra-large hospitals. J Korean Surg Soc. 2011; 80:373–383. PMID: 22066063.

20. Huguet M. Centralization of care in high volume hospitals and inequalities in access to care. Soc Sci Med. 2020; 260:113177. PMID: 32712556.

21. Schold JD, Elfadawy N, Buccini LD, Goldfarb DA, Flechner SM, P Phelan M, et al. Emergency department visits after kidney transplantation. Clin J Am Soc Nephrol. 2016; 11:674–683. PMID: 27012951.

22. Park S, Kim M, Kim JE, Kim K, Park M, Kim YC, et al. Characteristics of kidney transplantation recipients over time in South Korea. Korean J Intern Med. 2020; 35:1457–1467. PMID: 32218102.

SUPPLEMENTARY MATERIALS
Supplementary Material 1 and Supplementary Fig. 1 can be found via https://doi.org/10.4174/astr.2024.106.1.11.
Supplementary Material 1
Medication codes of dialysis solution from the NHIS database
Supplementary Fig. 1
Relationship between the patient’s residence and the kidney transplant hospital region in South Korea (2002–2017). *Sejong was established as a major city in 2012.
Fig. 1
Cumulative kidney transplantation numbers in major South Korean metropolitan cities (2002–2017).
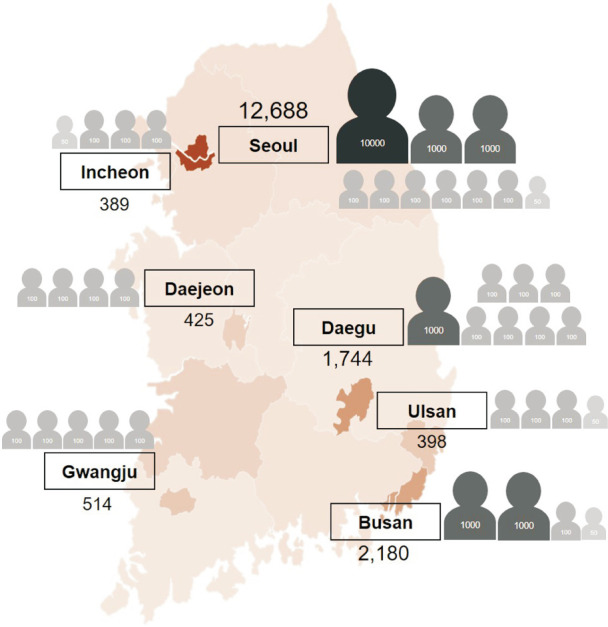
Fig. 2
Kidney transplantation (KT) numbers in major South Korean metropolitan cities (2002–2017), categorized by hospital region and patient residence (per million population). (A) Kidney transplantations per million population, categorized by hospital region (2002–2017). (B) Kidney transplantations per million population, categorized by patient residence (2002–2017).
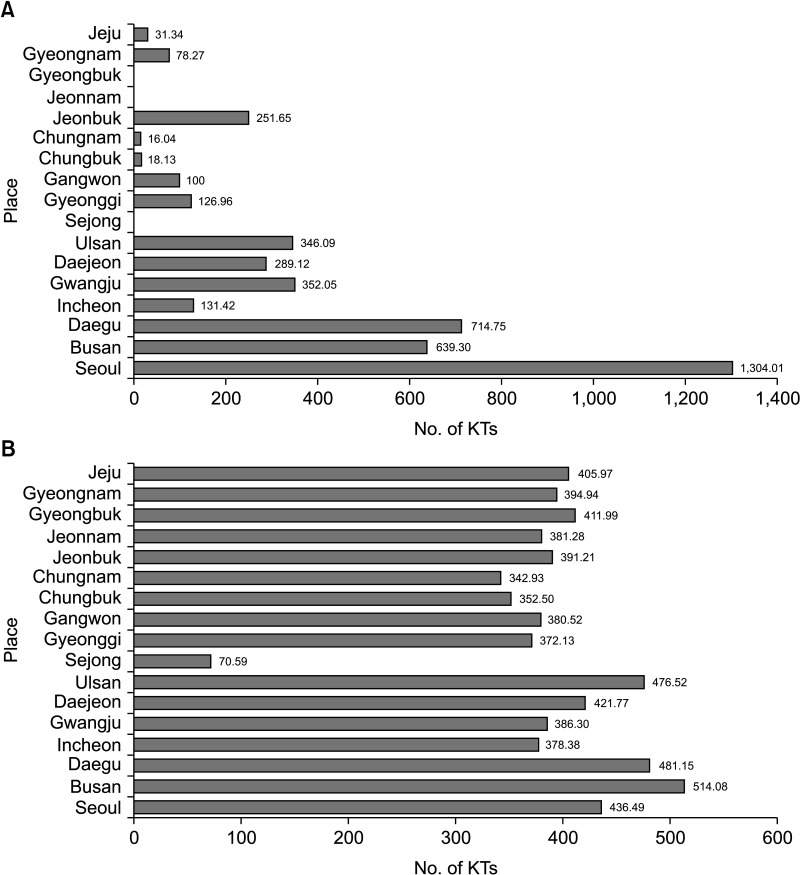
Fig. 3
Kaplan-Meier plots for 10-year graft survival after kidney transplantations performed from 2002 to 2007. (A) Ten-year graft survival after kidney transplantations between 2002 and 2007. (B) Ten-year graft survival categorized by residence. (C) Ten-year graft survival for both Seoul and non-Seoul major cities, categorized by residence.
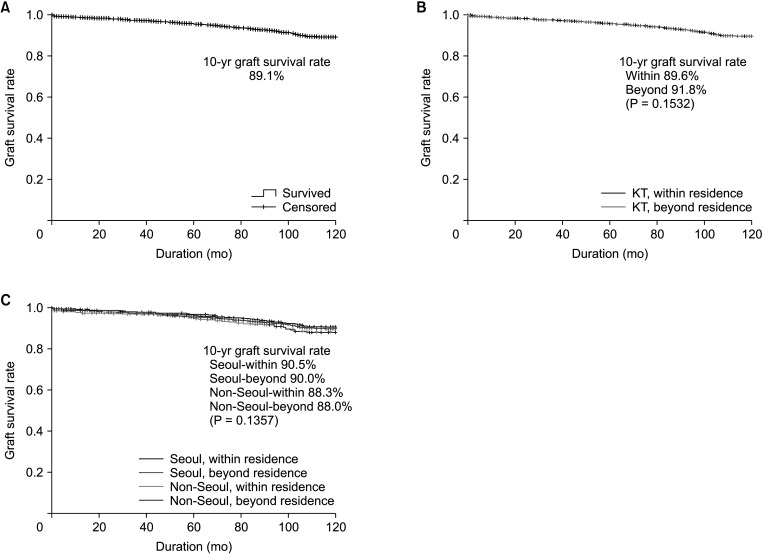
Table 1
Cumulative kidney transplantation (KT) counts in major metropolitan cities and districts in South Korea (2002–2017)
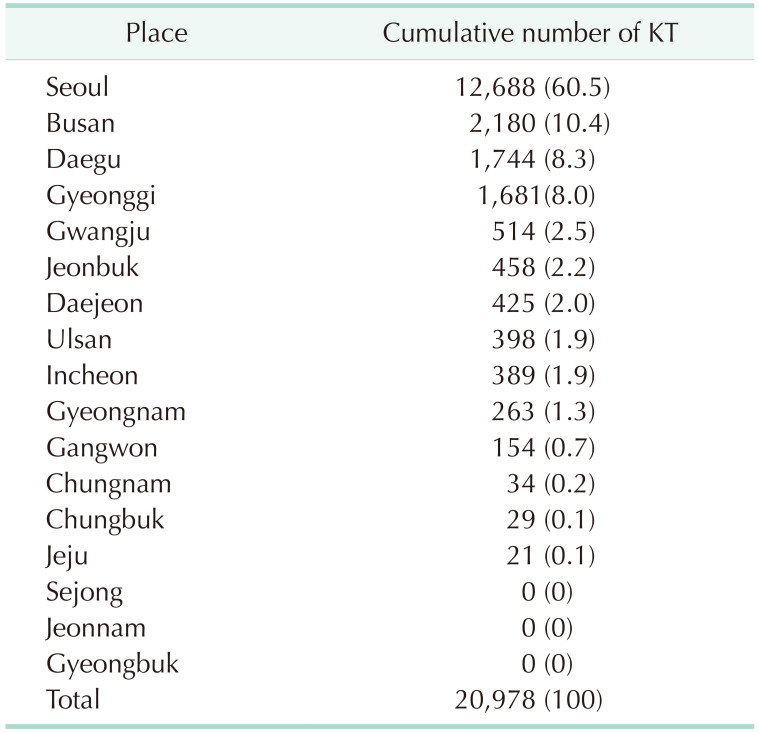
Table 2
Graft survival rate among kidney transplant (KT) patients residing in major metropolitan cities in South Korea (2002–2017)




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download