1. Lugo LM, Ferreiro JL. Dual antiplatelet therapy after coronary stent implantation: Individualizing the optimal duration. J Cardiol. 2018; 72(2):94–104. PMID:
29602648.
2. Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018; 39(3):213–260. PMID:
28886622.
3. Ammirati E, Guida V, Latib A, Moroni F, Arioli F, Scotti I, et al. Determinants of outcome in patients with chronic ischemic left ventricular dysfunction undergone percutaneous coronary interventions. BMC Cardiovasc Disord. 2015; 15(1):137. PMID:
26503520.
4. Shantsila E, Lip GY. Antiplatelet versus anticoagulation treatment for patients with heart failure in sinus rhythm. Cochrane Database Syst Rev. 2016; 9(9):CD003333. PMID:
27629776.
5. Marcano AL, Lugo LM, Besteiro A, Gomez-Lara J, Roura G, Fuentes L, et al. Association of fractalkine with functional severity of heart failure and impact on clopidogrel efficacy in patients with ischemic heart disease. Thromb Res. 2020; 196:215–221. PMID:
32916563.
6. Quyyumi AA, Cannon RO 3rd, Panza JA, Diodati JG, Epstein SE. Endothelial dysfunction in patients with chest pain and normal coronary arteries. Circulation. 1992; 86(6):1864–1871. PMID:
1451258.
7. Steinhubl SR, Berger PB, Mann JT 3rd, Fry ET, DeLago A, Wilmer C, et al. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002; 288(19):2411–2420. PMID:
12435254.
8. Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357(20):2001–2015. PMID:
17982182.
9. Park Y, Kim KH, Kang MG, Ahn JH, Jang JY, Park HW, et al. Antiplatelet therapy combinations and thrombogenicity in patients with non-valvular atrial fibrillation. Korean Circ J. 2017; 47(3):366–376. PMID:
28567087.
10. Matetzky S, Shenkman B, Guetta V, Shechter M, Beinart R, Goldenberg I, et al. Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation. 2004; 109(25):3171–3175. PMID:
15184279.
11. Gurbel PA, Bliden KP, Samara W, Yoho JA, Hayes K, Fissha MZ, et al. Clopidogrel effect on platelet reactivity in patients with stent thrombosis: results of the CREST Study. J Am Coll Cardiol. 2005; 46(10):1827–1832. PMID:
16286166.
12. Geisler T, Langer H, Wydymus M, Göhring K, Zürn C, Bigalke B, et al. Low response to clopidogrel is associated with cardiovascular outcome after coronary stent implantation. Eur Heart J. 2006; 27(20):2420–2425. PMID:
17005534.
13. Hochholzer W, Trenk D, Bestehorn HP, Fischer B, Valina CM, Ferenc M, et al. Impact of the degree of peri-interventional platelet inhibition after loading with clopidogrel on early clinical outcome of elective coronary stent placement. J Am Coll Cardiol. 2006; 48(9):1742–1750. PMID:
17084243.
14. Adamski P, Buszko K, Sikora J, Niezgoda P, Fabiszak T, Ostrowska M, et al. Determinants of high platelet reactivity in patients with acute coronary syndromes treated with ticagrelor. Sci Rep. 2019; 9(1):3924. PMID:
30850677.
15. Cornel JH, Ohman EM, Neely B, Jakubowski JA, Bhatt DL, White HD, et al. Relationship of platelet reactivity with bleeding outcomes during long-term treatment with dual antiplatelet therapy for medically managed patients with non-st-segment elevation acute coronary syndromes. J Am Heart Assoc. 2016; 5(11):e003977. PMID:
27815268.
16. Nishikawa M, Isshiki T, Kimura T, Ogawa H, Yokoi H, Miyazaki S, et al. No association between on-treatment platelet reactivity and bleeding events following percutaneous coronary intervention and antiplatelet therapy: a post hoc analysis. Thromb Res. 2015; 136(5):947–954. PMID:
26460279.
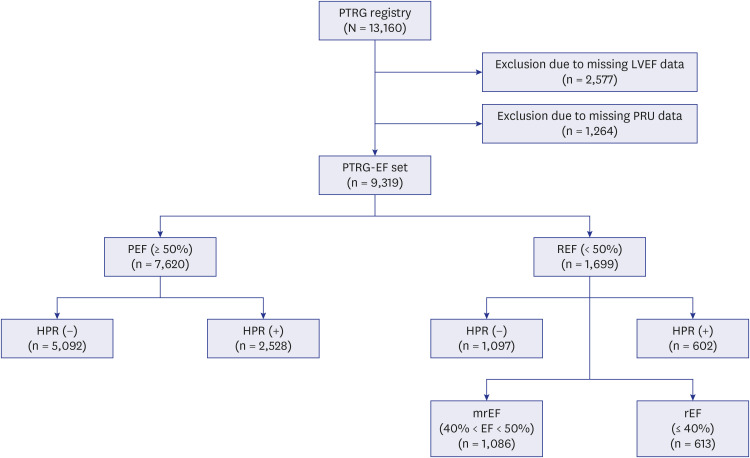
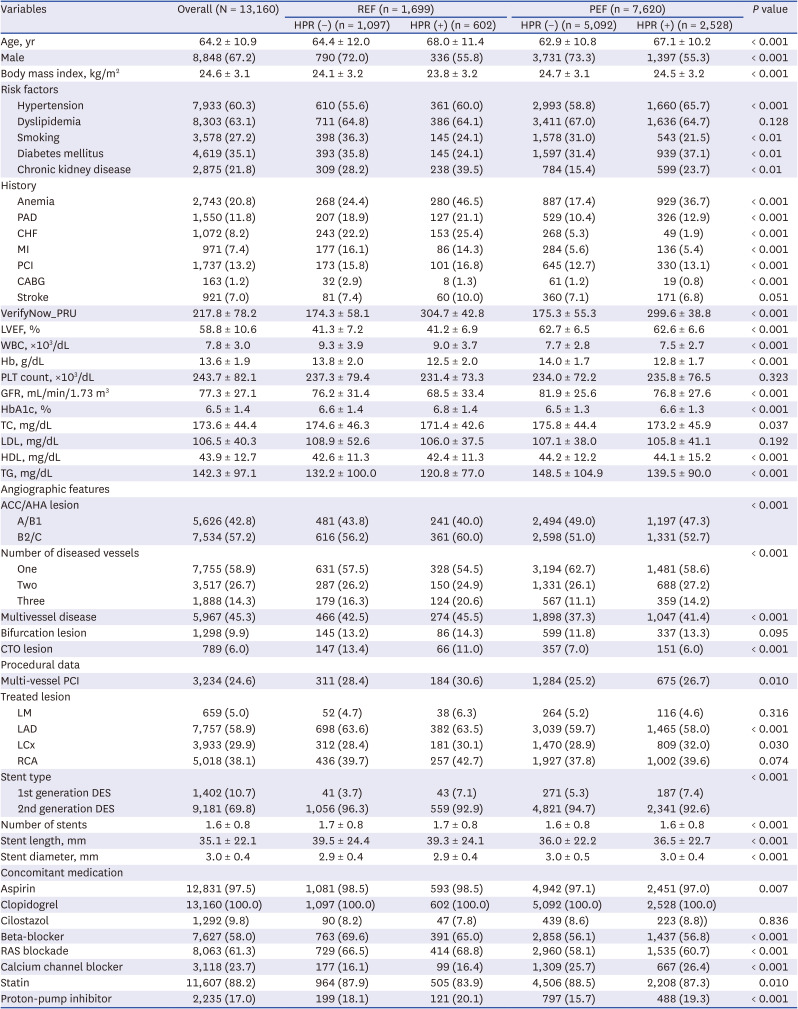
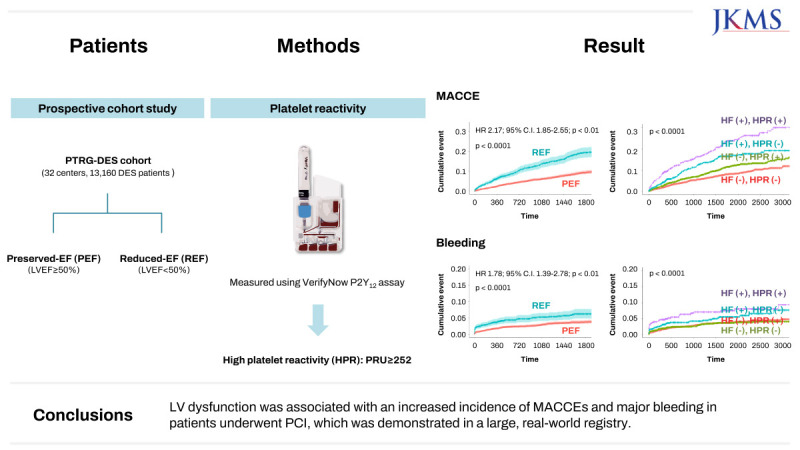
17. Her AY, Jeong YH, Kim BK, Joo HJ, Chang K, Park Y, et al. Platelet function and genotype after DES implantation in east asian patients: rationale and characteristics of the PTRG-DES consortium. Yonsei Med J. 2022; 63(5):413–421. PMID:
35512743.
18. Patel MR, Calhoon JH, Dehmer GJ, Grantham JA, Maddox TM, Maron DJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2017; 69(17):2212–2241. PMID:
28291663.
19. Sibbing D, Aradi D, Alexopoulos D, Ten Berg J, Bhatt DL, Bonello L, et al. Updated expert consensus statement on platelet function and genetic testing for guiding P2Y
12 receptor inhibitor treatment in percutaneous coronary intervention. JACC Cardiovasc Interv. 2019; 12(16):1521–1537. PMID:
31202949.
20. Jeong YH, Bliden KP, Antonino MJ, Park KS, Tantry US, Gurbel PA. Usefulness of the VerifyNow P2Y12 assay to evaluate the antiplatelet effects of ticagrelor and clopidogrel therapies. Am Heart J. 2012; 164(1):35–42. PMID:
22795280.
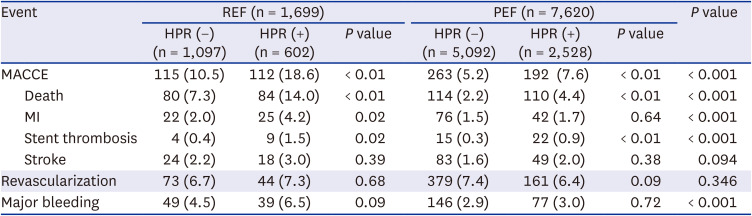
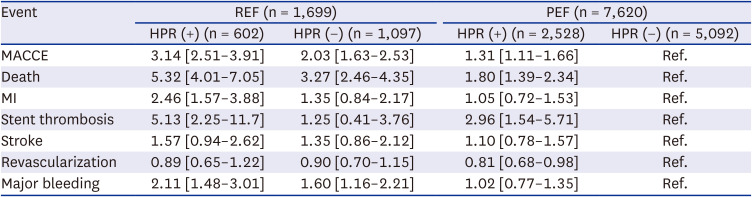
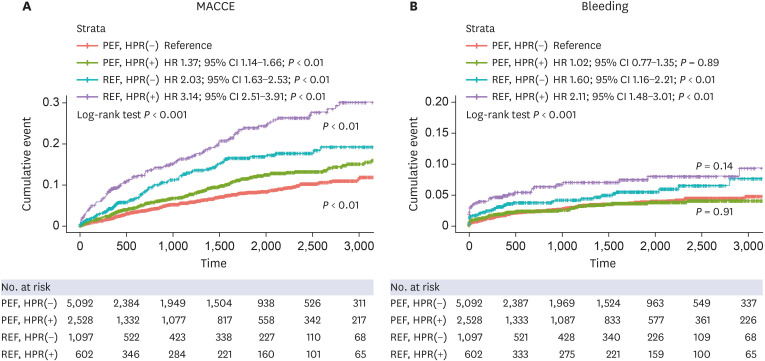
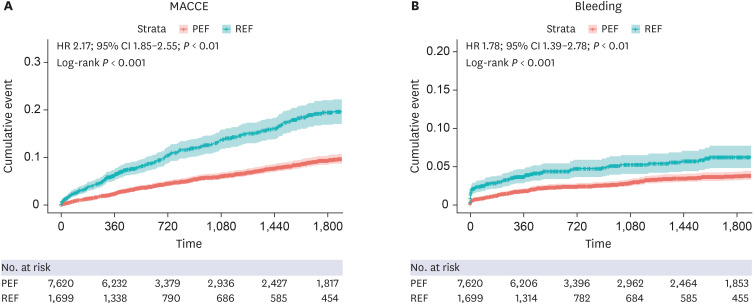
21. Lee SJ, Cha JJ, Jeong YH, Hong SJ, Ahn CM, Kim JS, et al. Platelet reactivity and clinical outcomes after drug-eluting stent implantation: results from the PTRG-DES consortium. JACC Cardiovasc Interv. 2022; 15(22):2253–2265. PMID:
36423968.
22. Porter TR, Shillcutt SK, Adams MS, Desjardins G, Glas KE, Olson JJ, et al. Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults: a report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2015; 28(1):40–56. PMID:
25559474.
23. Folland ED, Parisi AF, Moynihan PF, Jones DR, Feldman CL, Tow DE. Assessment of left ventricular ejection fraction and volumes by real-time, two-dimensional echocardiography. A comparison of cineangiographic and radionuclide techniques. Circulation. 1979; 60(4):760–766. PMID:
476879.
24. Cannon CP, Brindis RG, Chaitman BR, Cohen DJ, Cross JT Jr, Drozda JP Jr, et al. 2013 ACCF/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes and coronary artery disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on clinical data standards (writing committee to develop acute coronary syndromes and coronary artery disease clinical data standards). J Am Coll Cardiol. 2013; 61(9):992–1025. PMID:
23369353.
25. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42(36):3599–3726. PMID:
34447992.
26. Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011; 123(23):2736–2747. PMID:
21670242.
27. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018; 72(18):2231–2264. PMID:
30153967.
28. Gawaz M. Role of platelets in coronary thrombosis and reperfusion of ischemic myocardium. Cardiovasc Res. 2004; 61(3):498–511. PMID:
14962480.
29. Maxwell SR, Lip GY. Reperfusion injury: a review of the pathophysiology, clinical manifestations and therapeutic options. Int J Cardiol. 1997; 58(2):95–117. PMID:
9049675.
30. Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000; 101(25):2981–2988. PMID:
10869273.
31. Lerman A, Holmes DR, Herrmann J, Gersh BJ. Microcirculatory dysfunction in ST-elevation myocardial infarction: cause, consequence, or both? Eur Heart J. 2007; 28(7):788–797. PMID:
17347176.
32. Prasad A, Stone GW, Holmes DR, Gersh B. Reperfusion injury, microvascular dysfunction, and cardioprotection: the “dark side” of reperfusion. Circulation. 2009; 120(21):2105–2112. PMID:
19933949.
33. Robbers LF, Eerenberg ES, Teunissen PF, Jansen MF, Hollander MR, Horrevoets AJ, et al. Magnetic resonance imaging-defined areas of microvascular obstruction after acute myocardial infarction represent microvascular destruction and haemorrhage. Eur Heart J. 2013; 34(30):2346–2353. PMID:
23594591.
34. Sorop O, Merkus D, de Beer VJ, Houweling B, Pistea A, McFalls EO, et al. Functional and structural adaptations of coronary microvessels distal to a chronic coronary artery stenosis. Circ Res. 2008; 102(7):795–803. PMID:
18292598.
35. Mills I, Fallon JT, Wrenn D, Sasken H, Gray W, Bier J, et al. Adaptive responses of coronary circulation and myocardium to chronic reduction in perfusion pressure and flow. Am J Physiol. 1994; 266(2 Pt 2):H447–H457. PMID:
8141345.
36. Heusch G, Libby P, Gersh B, Yellon D, Böhm M, Lopaschuk G, et al. Cardiovascular remodelling in coronary artery disease and heart failure. Lancet. 2014; 383(9932):1933–1943. PMID:
24831770.
37. Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990; 81(4):1161–1172. PMID:
2138525.
38. Lin FJ, Tseng WK, Yin WH, Yeh HI, Chen JW, Wu CC. Residual risk factors to predict major adverse cardiovascular events in atherosclerotic cardiovascular disease patients with and without diabetes mellitus. Sci Rep. 2017; 7(1):9179. PMID:
28835613.
39. Kim W, Kim EJ. Heart failure as a risk factor for stroke. J Stroke. 2018; 20(1):33–45. PMID:
29402070.
40. Mebazaa A, Spiro TE, Büller HR, Haskell L, Hu D, Hull R, et al. Predicting the risk of venous thromboembolism in patients hospitalized with heart failure. Circulation. 2014; 130(5):410–418. PMID:
24970782.
41. Chung I, Lip GY. Platelets and heart failure. Eur Heart J. 2006; 27(22):2623–2631. PMID:
17028108.
42. Gurbel PA, Tantry US. Antiplatelet and anticoagulant agents in heart failure: current status and future perspectives. JACC Heart Fail. 2014; 2(1):1–14. PMID:
24622113.
43. McMurray JJ, Ezekowitz JA, Lewis BS, Gersh BJ, van Diepen S, Amerena J, et al. Left ventricular systolic dysfunction, heart failure, and the risk of stroke and systemic embolism in patients with atrial fibrillation: insights from the ARISTOTLE trial. Circ Heart Fail. 2013; 6(3):451–460. PMID:
23575255.
44. Kirchhof P, Haas S, Amarenco P, Hess S, Lambelet M, van Eickels M, et al. Impact of modifiable bleeding risk factors on major bleeding in patients with atrial fibrillation anticoagulated with rivaroxaban. J Am Heart Assoc. 2020; 9(5):e009530. PMID:
32079476.
45. Mentias A, Briasoulis A, Shantha G, Alvarez P, Vaughan-Sarrazin M. Impact of heart failure type on thromboembolic and bleeding risk in patients with atrial fibrillation on oral anticoagulation. Am J Cardiol. 2019; 123(10):1649–1653. PMID:
30928033.
46. Melgaard L, Overvad TF, Skjøth F, Christensen JH, Larsen TB, Lip GY. Risk of stroke and bleeding in patients with heart failure and chronic kidney disease: a nationwide cohort study. ESC Heart Fail. 2018; 5(2):319–326. PMID:
29383860.
47. O’Rourke MF, Safar ME. Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension. 2005; 46(1):200–204. PMID:
15911742.
48. Stone GW, Witzenbichler B, Weisz G, Rinaldi MJ, Neumann FJ, Metzger DC, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013; 382(9892):614–623. PMID:
23890998.
49. Brar SS, ten Berg J, Marcucci R, Price MJ, Valgimigli M, Kim HS, et al. Impact of platelet reactivity on clinical outcomes after percutaneous coronary intervention. A collaborative meta-analysis of individual participant data. J Am Coll Cardiol. 2011; 58(19):1945–1954. PMID:
22032704.
50. Price MJ, Angiolillo DJ, Teirstein PS, Lillie E, Manoukian SV, Berger PB, et al. Platelet reactivity and cardiovascular outcomes after percutaneous coronary intervention: a time-dependent analysis of the Gauging Responsiveness with a VerifyNow P2Y12 assay: impact on thrombosis and safety (GRAVITAS) trial. Circulation. 2011; 124(10):1132–1137. PMID:
21875913.
51. Kang J, Park KW, Palmerini T, Stone GW, Lee MS, Colombo A, et al. Racial differences in ischaemia/bleeding risk trade-off during anti-platelet therapy: individual patient level landmark meta-analysis from seven RCTs. Thromb Haemost. 2019; 119(1):149–162. PMID:
30597509.
52. Nishikawa M, Takeda Y, Isomura N, Tanigawa T, Nanasato M, Tsukahara K, et al. Association between high platelet reactivity following dual antiplatelet therapy and ischemic events in japanese patients with coronary artery disease undergoing stent implantation. J Atheroscler Thromb. 2020; 27(1):13–24. PMID:
31092743.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download