1. Barbosa JG, Benetti F, de Oliveira Gallinari M, Carminatti M, da Silva ABD, Lopes INI, et al. Bleaching gel mixed with MI Paste Plus reduces penetration of H
2O
2 and damage to pulp tissue and maintains bleaching effectiveness. Clin Oral Investig. 2020; 24:1299–1309.

2. Vladislavic NZ, Tadin A, Gavic L, Jerkovic D, Franic I, Verzak Z.
In vivo evaluation of whitening toothpaste efficiency and patient treatment satisfaction: a randomized controlled trial. Clin Oral Investig. 2022; 26:739–750.

3. Gallinari MO, Cintra LTÂ, Benetti F, Rahal V, Ervolino E, Briso ALF. Pulp response of rats submitted to bleaching and the use of different anti-inflammatory drugs. PLoS One. 2019; 14:e0210338. PMID:
30620760.

4. Costa CA, Riehl H, Kina JF, Sacono NT, Hebling J. Human pulp responses to in-office tooth bleaching. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e59–e64.
5. Cintra LT, Benetti F, da Silva Facundo AC, Ferreira LL, Gomes-Filho JE, Ervolino E, et al. The number of bleaching sessions influences pulp tissue damage in rat teeth. J Endod. 2013; 39:1576–1580. PMID:
24238450.

6. Soares DG, Ribeiro AP, Lima AF, Sacono NT, Hebling J, de Souza Costa CA. Effect of fluoride-treated enamel on indirect cytotoxicity of a 16% carbamide peroxide bleaching gel to pulp cells. Braz Dent J. 2013; 24:121–127. PMID:
23780364.

7. Reis-Prado AH, Grossi IR, Chaves HGS, André CB, Morgan LFSA, Briso ALF, et al. Influence of hydrogen peroxide on mineralization in dental pulp cells: a systematic review. Front Dent Med. 2021; 2:689537.

8. Favoreto MW, Vochikovski L, Terra RMO, Campos VS, Santos ME, Meireles SS, et al. Topical application of Otosporin® before in-office bleaching: a split mouth, triple-blind, multicenter randomized clinical trial. Clin Oral Investig. 2022; 26:2555–2564.

9. Vochikovski L, Favoreto MW, Rezende M, Terra RMO, da Silva KL, Farago PV, et al. Effect of an experimental desensitizing gel on bleaching-induced tooth sensitivity after in-office bleaching-a double-blind, randomized controlled trial. Clin Oral Investig. 2023; 27:1567–1576.

10. Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: a multi regression and logistic analysis. J Dent. 2016; 45:1–6. PMID:
26612623.

11. Benetti F, Briso ALF, Ferreira LL, Carminatti M, Álamo L, Ervolino E, et al.
In vivo study of the action of a topical anti-inflammatory drug in rat teeth submitted to dental bleaching. Braz Dent J. 2018; 29:555–561. PMID:
30517478.

12. Carminatti M, Benetti F, Siqueira RL, Zanotto ED, Briso ALF, Chaves-Neto AH, et al. Experimental gel containing bioactive glass-ceramic to minimize the pulp damage caused by dental bleaching in rats. J Appl Oral Sci. 2020; 28:e20190384. PMID:
32520077.

13. Santana Jorge O, Noronha Ferraz de Arruda C, Tonani Torrieri R, Geng Vivanco R, de Carvalho Panzeri Pires-de-Souza F. Over-the-counter bleaching agents can help with tooth whitening maintenance. J Esthet Restor Dent. 2022; 34:328–334. PMID:
32627389.

14. Souza RO, Lombardo GH, Pereira SM, Zamboni SC, Valera MC, Araujo MA, et al. Analysis of tooth enamel after excessive bleaching: a study using scanning electron microscopy and energy dispersive X-ray spectroscopy. Int J Prosthodont. 2010; 23:29–32. PMID:
20234888.
15. Deng M, Wen HL, Dong XL, Li F, Xu X, Li H, et al. Effects of 45S5 bioglass on surface properties of dental enamel subjected to 35% hydrogen peroxide. Int J Oral Sci. 2013; 5:103–110. PMID:
23743618.
16. Yang SY, Han AR, Kim KM, Kwon JS. Effects of incorporating 45S5 bioactive glass into 30% hydrogen peroxide solution on whitening efficacy and enamel surface properties. Clin Oral Investig. 2022; 26:5301–5312.

17. Lima AF, Marques MR, Soares DG, Hebling J, Marchi GM, de Souza Costa CA. Antioxidant therapy enhances pulpal healing in bleached teeth. Restor Dent Endod. 2016; 41:44–54. PMID:
26877990.

18. Benetti F, Gomes-Filho JE, Ferreira LL, Ervolino E, Briso ALF, Sivieri-Araújo G, et al. Hydrogen peroxide induces cell proliferation and apoptosis in pulp of rats after dental bleaching
in vivo: effects of the dental bleaching in pulp. Arch Oral Biol. 2017; 81:103–109. PMID:
28500951.

19. Benetti F, Gomes-Filho JE, Ferreira LL, Sivieri-Araújo G, Ervolino E, Briso ALF, et al. Concentration-dependent effect of bleaching agents on the immunolabelling of interleukin-6, interleukin-17 and CD5-positive cells in the dental pulp. Int Endod J. 2018; 51:789–799. PMID:
29352770.

20. Benetti F, Briso ALF, Carminatti M, de Araújo Lopes JM, Barbosa JG, Ervolino E, et al. The presence of osteocalcin, osteopontin and reactive oxygen species-positive cells in pulp tissue after dental bleaching. Int Endod J. 2019; 52:665–675. PMID:
30488465.

21. Benetti F, Briso ALF, de Araújo Lopes JM, Carminatti M, Conti LC, Gallinari MO, et al.
In vivo analysis of the presence of heme oxygenase-1, transcription factor Jun-D and CD90
+/CD73
+/CD105
+/CD45
- cells in the pulp of bleached teeth. Int Endod J. 2019; 52:1723–1737. PMID:
31322737.

22. Cintra LT, Benetti F, Ferreira LL, Gomes-Filho JE, Ervolino E, Gallinari MO, et al. Penetration capacity, color alteration and biological response of 2 in-office bleaching protocols. Braz Dent J. 2016; 27:169–175. PMID:
27058379.

23. Soares DG, Marcomini N, Duque CCO, Bordini EAF, Zuta UO, Basso FG, et al. Increased whitening efficacy and reduced cytotoxicity are achieved by the chemical activation of a highly concentrated hydrogen peroxide bleaching gel. J Appl Oral Sci. 2019; 27:e20180453. PMID:
31411261.

24. Lee DS, Li B, Kim KS, Jeong GS, Kim EC, Kim YC. Butein protects human dental pulp cells from hydrogen peroxide-induced oxidative toxicity via Nrf2 pathway-dependent heme oxygenase-1 expressions. Toxicol In Vitro. 2013; 27:874–881. PMID:
23318726.

25. da Silva LMAV, Cintra LTA, Gallinari MO, Benetti F, Rahal V, Ervolino E, et al. Influence of pain-relieving therapies on inflammation and the expression of proinflammatory neuropeptides after dental bleaching treatment. Restor Dent Endod. 2020; 45:e20. PMID:
32483537.

26. Louzada LM, Briso ALF, Benetti F, Vieira LB, de Castilho Jacinto R, Dezan-Júnior E, et al. Anti-inflammatory potential of a carvedilol gel in the pulpal tissue of rats after dental bleaching: a histopathological evaluation. J Investig Clin Dent. 2019; 10:e12401.

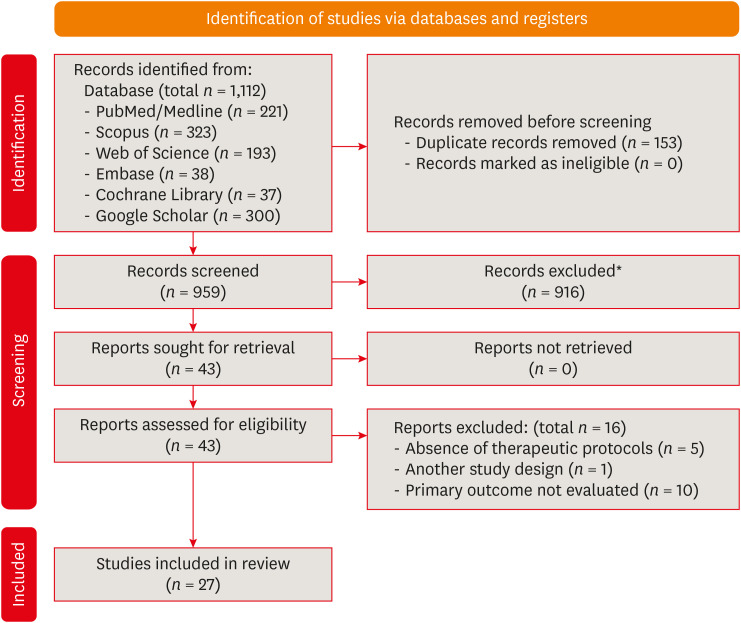
27. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. 2021; 134:103–112. PMID:
33577987.

28. Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS One. 2015; 10:e0138237. PMID:
26379270.

29. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID:
843571.

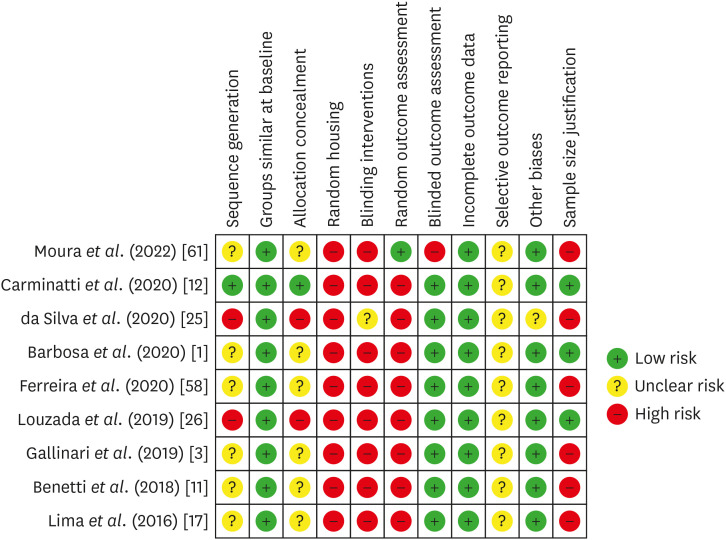
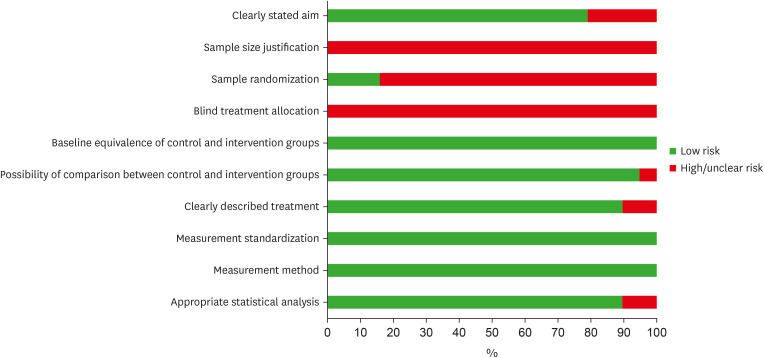
30. Hooijmans CR, Rovers MM, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014; 14:43. PMID:
24667063.

31. Dos Reis-Prado AH, Abreu LG, Tavares WLF, Peixoto IFDC, Viana ACD, de Oliveira EMC, et al. Comparison between immediate and delayed post space preparations: a systematic review and meta-analysis. Clin Oral Investig. 2021; 25:417–440.

32. Schulte JR, Morrissette DB, Gasior EJ, Czajewski MV. The effects of bleaching application time on the dental pulp. J Am Dent Assoc. 1994; 125:1330–1335. PMID:
7844297.

33. Soares DG, Ribeiro AP, Sacono NT, Coldebella CR, Hebling J, Costa CA. Transenamel and transdentinal cytotoxicity of carbamide peroxide bleaching gels on odontoblast-like MDPC-23 cells. Int Endod J. 2011; 44:116–125. PMID:
21083572.

34. Soares DG, Ribeiro AP, da Silveira Vargas F, Hebling J, de Souza Costa CA. Efficacy and cytotoxicity of a bleaching gel after short application times on dental enamel. Clin Oral Investig. 2013; 17:1901–1909.
35. Soares DG, Basso FG, Hebling J, de Souza Costa CA. Immediate and late analysis of dental pulp stem cells viability after indirect exposition to alternative in-office bleaching strategies. Clin Oral Investig. 2015; 19:1013–1020.
36. Guazzo R, Gardin C, Bellin G, Sbricoli L, Ferroni L, Ludovichetti FS, et al. Graphene-based nanomaterials for tissue engineering in the dental field. Nanomaterials (Basel). 2018; 8:349. PMID:
29783786.

37. Babich H, Reisbaum AG, Zuckerbraun HL.
In vitro response of human gingival epithelial S-G cells to resveratrol. Toxicol Lett. 2000; 114:143–153. PMID:
10713479.
38. Soares DG, Basso FG, Pontes EC, Garcia LF, Hebling J, de Souza Costa CA. Effective tooth-bleaching protocols capable of reducing H
2O
2 diffusion through enamel and dentine. J Dent. 2014; 42:351–358. PMID:
24056046.

39. Kwon SR, Dawson DV, Schenck DM, Fiegel J, Wertz PW. Spectrophotometric evaluation of potassium nitrate penetration into the pulp cavity. Oper Dent. 2015; 40:614–621. PMID:
26151563.

40. Kwon SR, Dawson DV, Wertz PW. Time course of potassium nitrate penetration into the pulp cavity and the effect of penetration levels on tooth whitening efficacy. J Esthet Restor Dent. 2016; 28(Supplement 1):S14–S22. PMID:
27079767.

41. Kwon SR, Pallavi F, Shi Y, Oyoyo U, Mohraz A, Li Y. Effect of bleaching gel viscosity on tooth whitening efficacy and pulp chamber penetration: an
in vitro study. Oper Dent. 2018; 43:326–334. PMID:
29676980.

42. Balladares L, Alegría-Acevedo LF, Montenegro-Arana A, Arana-Gordillo LA, Pulido C, Salazar-Gracez MT, et al. Effects of pH and application technique of in-office bleaching gels on hydrogen peroxide penetration into the pulp chamber. Oper Dent. 2019; 44:659–667. PMID:
31009314.

43. Ma Q, Chen J, Xu X, Wang T. Impact of transparent tray-based application of bioactive glasses desensitizer on the permeability of enamel and dentin to hydrogen peroxide: an
in vitro study. BMC Oral Health. 2020; 20:103. PMID:
32276623.
44. Parreiras SO, Favoreto MW, Lenz RE, Serra ME, Borges CPF, Loguercio AD, et al. Effect of prior application of desensitizing agent on the teeth submitted to in-office bleaching. Braz Dent J. 2020; 31:236–243. PMID:
32667516.

45. Duque CC, Soares DG, Basso FG, Hebling J, de Souza Costa CA. Bleaching effectiveness, hydrogen peroxide diffusion, and cytotoxicity of a chemically activated bleaching gel. Clin Oral Investig. 2014; 18:1631–1637.
46. Jeong GS, Lee DS, Li B, Lee HJ, Kim EC, Kim YC. Effects of sappanchalcone on the cytoprotection and anti-inflammation via heme oxygenase-1 in human pulp and periodontal ligament cells. Eur J Pharmacol. 2010; 644:230–237. PMID:
20621084.

47. Lima AF, Lessa FC, Mancini MN, Hebling J, Costa CA, Marchi GM. Transdentinal protective role of sodium ascorbate against the cytopathic effects of H2O2 released from bleaching agents. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e70–e76.
48. Choi YJ, Lee JY, Chung CP, Park YJ. Cell-penetrating superoxide dismutase attenuates oxidative stress-induced senescence by regulating the p53-p21(Cip1) pathway and restores osteoblastic differentiation in human dental pulp stem cells. Int J Nanomedicine. 2012; 7:5091–5106. PMID:
23049256.
49. Lee YH, Kang YM, Heo MJ, Kim GE, Bhattarai G, Lee NH, et al. The survival role of peroxisome proliferator-activated receptor gamma induces odontoblast differentiation against oxidative stress in human dental pulp cells. J Endod. 2013; 39:236–241. PMID:
23321237.

50. Lee DS, Kim KS, Ko W, Keo S, Jeong GS, Oh H, et al. Cytoprotective effects of sulfuretin from Rhus verniciflua through regulating of heme oxygenase-1 in human dental pulp cells. Nat Prod Sci. 2013; 19:54–60.
51. Lee YH, Lee NH, Bhattarai G, Kim GE, Lee IK, Yun BS, et al. Anti-inflammatory effect of pachymic acid promotes odontoblastic differentiation via HO-1 in dental pulp cells. Oral Dis. 2013; 19:193–199. PMID:
22849812.

52. Vargas FS, Soares DG, Basso FG, Hebling J, Costa CA. Dose-response and time-course of α-tocoferol mediating the cytoprotection of dental pulp cells against hydrogen peroxide. Braz Dent J. 2014; 25:367–371. PMID:
25517769.

53. da Silveira Vargas F, Soares DG, Ribeiro AP, Hebling J, De Souza Costa CA. Protective effect of alpha-tocopherol isomer from vitamin E against the H
2O
2 induced toxicity on dental pulp cells. BioMed Res Int. 2014; 2014:895049. PMID:
24587995.
54. Kim D, Kim H, Kim K, Roh S. The protective effect of indole-3-acetic acid (IAA) on H
2O
2-damaged human dental pulp stem cells is mediated by the AKT pathway and involves increased expression of the transcription factor nuclear factor-erythroid 2-related factor 2 (Nrf2) and its downstream target heme oxygenase 1 (HO-1). Oxid Med Cell Longev. 2017; 2017:8639485. PMID:
28694916.

55. Kim NY, Ahn SG, Kim SA. Cinnamaldehyde protects human dental pulp cells against oxidative stress through the Nrf2/HO-1-dependent antioxidant response. Eur J Pharmacol. 2017; 815:73–79. PMID:
28882558.

56. Huang S, Zheng B, Jin X, Yu Q, Zhang X, Sun X, et al. Blockade of cyclophilin D attenuates oxidative stress-induced cell death in human dental pulp cells. Oxid Med Cell Longev. 2019; 2019:1729013. PMID:
31089403.

57. Ortecho-Zuta U, de Oliveira Duque CC, Leite ML, Bordini E, Basso FG, Hebling J, et al. Effects of enzymatic activation of bleaching gels on hydrogen peroxide degradation rates, bleaching effectiveness, and cytotoxicity. Oper Dent. 2019; 44:414–423. PMID:
30444688.

58. Ferreira L, Benetti F, Álamo L, Bosisio AC, Proença A, Rahal V, et al. Otosporin reduces pulp inflammatory reactions after dental bleaching of rat molars. Dent Press Endod. 2020; 10:54–61.
59. Ribeiro R, de Oliveira Duque CC, Ortecho-Zuta U, Leite ML, Hebling J, Soares DG, et al. Influence of manganese oxide on the esthetic efficacy and toxicity caused by conventional in-office tooth bleaching therapy. Oper Dent. 2022; 47:425–436. PMID:
35917237.

60. de Oliveira Ribeiro RA, Zuta UO, Soares IPM, Anselmi C, Soares DG, Briso ALF, et al. Manganese oxide increases bleaching efficacy and reduces the cytotoxicity of a 10% hydrogen peroxide bleaching gel. Clin Oral Investig. 2022; 26:7277–7286.

61. Moura SKSCF, dos Santos MLV, do Nascimento LA, da Silva MFA, de França GM, da Costa LM, et al. Design of a thermosensitive ibuprofen-loaded nanogel as smart material applied as anti-inflammatory in tooth bleaching: an in vivo study. J Drug Deliv Sci Technol. 2022; 68:103123.
62. Dias MF, Martins BV, de Oliveira Ribeiro RA, Leite ML, Ortecho-Zuta U, Hebling J, et al. A new approach for professional dental bleaching using a polymeric catalyst primer. J Esthet Restor Dent. 2023; 35:406–415. PMID:
36193855.

63. Cintra LT, Benetti F, Ferreira LL, Rahal V, Ervolino E, Jacinto RC, et al. Evaluation of an experimental rat model for comparative studies of bleaching agents. J Appl Oral Sci. 2016; 24:95–104. PMID:
27008262.

64. Benetti F, Lemos CAA, de Oliveira Gallinari M, Terayama AM, Briso ALF, de Castilho Jacinto R, et al. Influence of different types of light on the response of the pulp tissue in dental bleaching: a systematic review. Clin Oral Investig. 2018; 22:1825–1837.

65. Caviedes-Bucheli J, Ariza-García G, Restrepo-Méndez S, Ríos-Osorio N, Lombana N, Muñoz HR. The effect of tooth bleaching on substance P expression in human dental pulp. J Endod. 2008; 34:1462–1465. PMID:
19026874.

66. Paula E, Kossatz S, Fernandes D, Loguercio A, Reis A. The effect of perioperative ibuprofen use on tooth sensitivity caused by in-office bleaching. Oper Dent. 2013; 38:601–608. PMID:
23586657.

67. Galler KM, Weber M, Korkmaz Y, Widbiller M, Feuerer M. Inflammatory response mechanisms of the dentine-pulp complex and the periapical tissues. Int J Mol Sci. 2021; 22:1480. PMID:
33540711.

68. Vaseenon S, Srisuwan T, Chattipakorn N, Chattipakorn SC. Lipopolysaccharides and hydrogen peroxide induce contrasting pathological conditions in dental pulpal cells. Int Endod J. 2023; 56:179–192. PMID:
36269677.

69. Panzarini SR, Trevisan CL, Brandini DA, Poi WR, Sonoda CK, Luvizuto ER, et al. Intracanal dressing and root canal filling materials in tooth replantation: a literature review. Dent Traumatol. 2012; 28:42–48. PMID:
22230725.

70. Marinho AC, Polay AR, Gomes BP. Accuracy of turbidimetric limulus amebocyte lysate assay for the recovery of endotoxin interacted with commonly used antimicrobial agents of endodontic therapy. J Endod. 2015; 41:1653–1659. PMID:
26254546.

71. Markovic L, Jordan RA, Lakota N, Gaengler P. Micromorphology of enamel surface after vital tooth bleaching. J Endod. 2007; 33:607–610. PMID:
17437883.

72. Jurema AL, Claudino ES, Torres CR, Bresciani E, Caneppele TM. Effect of over-the-counter whitening products associated or not with 10% carbamide peroxide on color change and microhardness:
in vitro study. J Contemp Dent Pract. 2018; 19:359–366. PMID:
29728537.
73. Bayrak S, Tunc ES, Sonmez IS, Egilmez T, Ozmen B. Effects of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) application on enamel microhardness after bleaching. Am J Dent. 2009; 22:393–396. PMID:
20178219.
74. Yassin O, Milly H. Effect of CPP-ACP on efficacy and postoperative sensitivity associated with at-home vital tooth bleaching using 20% carbamide peroxide. Clin Oral Investig. 2019; 23:1555–1559.

75. Pintado-Palomino K, Tirapelli C. The effect of home-use and in-office bleaching treatments combined with experimental desensitizing agents on enamel and dentin. Eur J Dent. 2015; 9:66–73. PMID:
25713487.

76. Charakorn P, Cabanilla LL, Wagner WC, Foong WC, Shaheen J, Pregitzer R, et al. The effect of preoperative ibuprofen on tooth sensitivity caused by in-office bleaching. Oper Dent. 2009; 34:131–135. PMID:
19363967.

77. de Souza Costa CA, Hebling J, Scheffel DL, Soares DG, Basso FG, Ribeiro AP. Methods to evaluate and strategies to improve the biocompatibility of dental materials and operative techniques. Dent Mater. 2014; 30:769–784. PMID:
24877759.

78. de Oliveira Duque CC, Soares DG, Basso FG, Hebling J, de Souza Costa CA. Influence of enamel/dentin thickness on the toxic and esthetic effects of experimental in-office bleaching protocols. Clin Oral Investig. 2017; 21:2509–2520.

79. Llena C, Martínez-Galdón O, Forner L, Gimeno-Mallench L, Rodríguez-Lozano FJ, Gambini J. Hydrogen peroxide diffusion through enamel and dentin. Materials (Basel). 2018; 11:1694. PMID:
30213083.

80. Sato C, Rodrigues FA, Garcia DM, Vidal CM, Pashley DH, Tjäderhane L, et al. Tooth bleaching increases dentinal protease activity. J Dent Res. 2013; 92:187–192. PMID:
23242228.

81. Garcia EJ, Mena-Serrano A, de Andrade AM, Reis A, Grande RH, Loguercio AD. Immediate bonding to bleached enamel treated with 10% sodium ascorbate gel: a case report with one-year follow-up. Eur J Esthet Dent. 2012; 7:154–162. PMID:
22645730.
82. The Council of the European Union. Council directive 2011/84/EU of 20 September 2011. Amending directive 76/768/EEC, concerning cosmetic products, for the purpose of adapting Annex III thereto to technical progress. Off J Eur Union. 2011; 283:36–38.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download