This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
The formation of new bone by periosteum due to an insult is called periosteal bone reaction (PBR). This study assessed the cone beam computed tomography (CBCT) patterns of periosteal bone reactions associated with periapical inflammatory lesion (apical periodontitis/periapical rarefying osteitis).
Materials and Methods
Twenty-two small field of view CBCT images of patients with PBR were selected from a database of a private practice limited to endodontics. The volume of the periapical inflammatory lesion, the presence of cortical fenestration, the distance of the root apices to the affected cortex, and the location, pattern, and longest diameter of the periosteal reaction were recorded. Statistical analysis was performed using Wilcoxon Ranksum, Fischer’s exact, Spearman Correlation Coefficient, and paired t-test.
Results
In all cases, periosteal bone reaction manifested as either parallel (90.9%) or irregular (9.1%). No correlation was found between periapical inflammatory lesion volume and the periosteal reaction's longest diameter (p > 0.05). Cortical fenestration was noted in 72.7% of the cases. In addition, the findings showed that periosteal reactions were located mostly on the buccal and were present 53.8% and 100% of the time in the mandible and maxilla, respectively.
Conclusions
The periosteal reactions of endodontic origin had a nonaggressive form (i.e., parallel or irregular), and none of the lesions resulted in a periosteal reaction with an ominous Codman’s triangle or spicule pattern.
Go to :

Keywords: Cone beam computed tomography, Differential diagnosis, Imaging, jaw, Periapical periodontitis, Periosteal bone reaction
INTRODUCTION
In recent years, research has helped us to understand how patterns of periosteal bone reactions come into existence, the nature of their progression, and the role they play in the field of endodontics. The formation of new bone by periosteum as a result of an insult is called periosteal reaction [
1]. There are many possible injuries or stimuli that can cause a cortical bone reaction, such as infection, trauma, arthritis, malignancies, and certain medications [
2]. When repair begins, the duration and aggressiveness of the underlying cause determine the pattern and manifestation of the new periosteal bone formation. An underlying disease that can progress rapidly can result in an aggressive periosteal reaction (
e.g., spiculated pattern or Codman triangle). In contrast, the conditions that are slowly progressing and are less invasive are expected to form nonaggressive patterns of bone formation (
e.g., parallel pattern) [
2]. Although it may not be possible to make an exact differential diagnosis based on the pattern of periosteal reaction, their appearance can suggest a certain disease type. The radiographic repair pattern can be one of the pieces of a puzzle that can help differentiate between malignant and non-malignant diseases.
Periosteal reaction is an incidental finding in conventional and 3-dimensional radiography of the jaws. This can be associated with various types of bony lesions, such as osteomyelitis, fracture, cysts, ossifying fibroma, fibrous dysplasia, and osteogenic sarcoma. Apical periodontitis is a common underlying disease that can also cause osteomyelitis of the jaw and, in many instances, may result in periosteal bone formation [
3]. The diagnosis of osteomyelitis can be made when radiographic features are correlated with clinical and histopathologic findings [
4]. However, the radiographic presence of periosteal bone formation is not sufficient evidence for a diagnosis of osteomyelitis. Even in the absence of clinical signs or symptoms of osteomyelitis, the identification of periosteal reaction is of utmost importance. A nonaggressive periosteal reaction associated with apical periodontitis/periapical rarefying osteitis indicates an intense inflammatory response and suggests the need for comprehensive treatment and long-term monitoring. More importantly, an aggressive form of periosteal reaction adjacent to a periapical radiolucency should be considered a warning sign and must be further evaluated for a possible non-endodontic etiology. Therefore, a thorough understanding of the radiographic patterns of new periosteal bone formation is essential for proper differential diagnosis.
To the best of our knowledge, no study has exclusively reported the periosteal bone formations associated with root canal infections. Therefore, this study aims to evaluate the cone beam computed tomography (CBCT) patterns of periosteal bone reactions associated with periapical inflammatory lesion (apical periodontitis/periapical rarefying osteitis [AP/PAR]).
Go to :

MATERIALS AND METHODS
Twenty-two small field of view CBCT images of patients with periosteal bone reaction were selected from a database of a private practice limited to endodontics. All the scans were obtained between July 2018 and December 2020 for routine endodontic examination and treatment planning. The images were obtained with CS 9300 device (Carestream Health, Rochester, NY, USA) with a voxel size of 90 mm (60–90 kV, 2–15 mA). The study protocol was approved by the institutional review board of the authors’ affiliated institution (IRB2021-0973). Inclusion criteria were as follows: cases with periosteal bone reaction associated with AP/PAR, and diagnostic-quality CBCT images.
The scans were evaluated simultaneously by 2 observers (an endodontist and an oral and maxillofacial radiologist) using InVivoMac application version 6.0.5 (Anatomage, San Jose, CA, USA) on a Macbook Pro 2018 (Apple Inc., Cupertino, CA, USA) with a 13.3-inch display and a resolution of 2560 × 1600.
The following radiographic data were recorded:
1) The volume of the periapical inflammatory lesion.
2) The presence or absence of cortical fenestration.
3) The presence or absence of root canal filling.
4) The distance of the apex/apices to the buccal and lingual/palatal cortex.
5) The location of the periosteal reaction (buccal or lingual/palatal).
6) The pattern of periosteal reaction; recorded as parallel, irregular, spicule, or Codman’s triangle [5].
7) Longest diameter of periosteal bone reaction.
The volume of the periapical inflammatory lesion was calculated using Mimics Innovation Suite Version 23 (Materialise NV, Leuven, Belgium) (
Figure 1). Radiolucent lesions were segmented using region grow, thresholding tools, and 3D Live wire tools. The volume of each periapical radiolucency was recorded after converting the masks to a 3-dimensional form. The volume of the lesions for multirooted teeth was measured according to the criteria previously described [
6]. The size of the periosteal bone reaction was measured in axial and sagittal views, and the longest diameter was recorded.
 | Figure 1 The volume of the apical periodontitis/periapical rarefying osteitis was calculated using Mimics Innovation Suite.
|
Statistical analysis
Stata/SE 16.1 (StataCorp, College Station, TX, USA) was used for statistical analysis. The data regarding the AP/PAR volume and the largest diameter of the periosteal reaction showed right-skewed distribution, and the Shapiro-Wilk test also confirmed the nonlinear distribution of the data. Wilcoxon Ranksum test was used to determine if the longest diameter of periosteal reaction and AP/PAR volume differed significantly between the maxilla and mandible. The location of periosteal reaction (occurrence in the buccal or lingual/palatal side) was compared between the maxilla and mandible using Fischer exact test. Also, paired t-test was used (normality confirmed with Shapiro-Wilk test and histogram) to determine if the mean distance of the apex to the affected side (buccal or lingual/palatal) differed significantly from the mean distance of the apex to the non-affected side (buccal or lingual/palatal). Spearman Correlation Coefficient was used to measure the correlation between the volume of the AP/PAR and the longest diameter of the periosteal reaction. The level of significance was set as 5% (p < 0.05).
Go to :

RESULTS
The CBCT scans of 22 patients (12 men and 9 women) ranging from 8–80 years old (median = 57, interquartile range = 19.5) with periosteal reaction were evaluated in this study. The demographic data and combined radiographic findings are summarized in
Table 1. The cross-tabulation of data based on the affected jaw is presented in
Table 2.
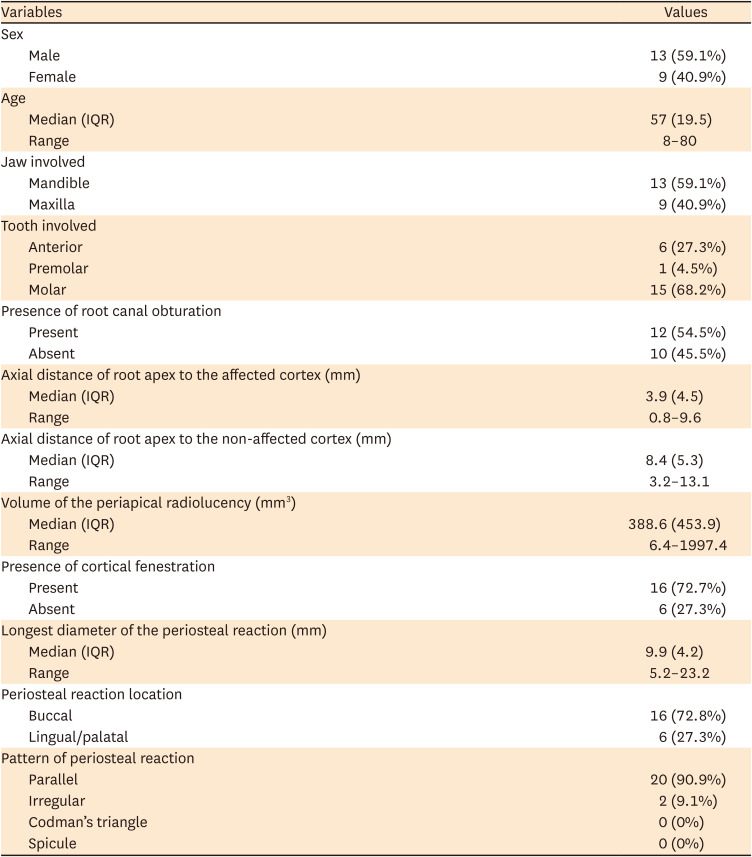
Table 1
Demographic data and radiographic findings
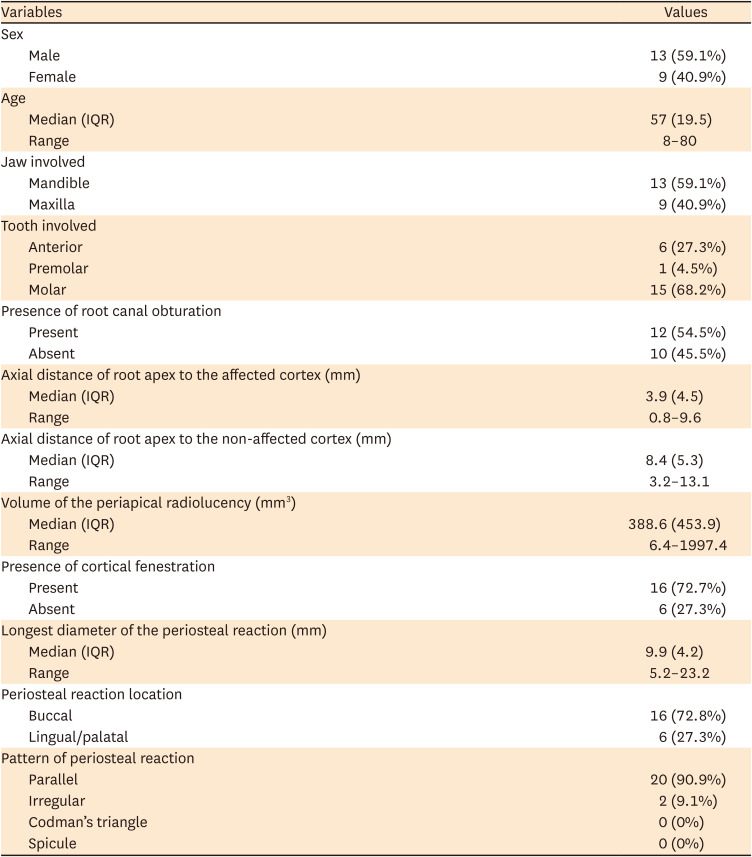
|
Variables |
Values |
|
Sex |
|
|
Male |
13 (59.1%) |
|
Female |
9 (40.9%) |
|
Age |
|
|
Median (IQR) |
57 (19.5) |
|
Range |
8–80 |
|
Jaw involved |
|
|
Mandible |
13 (59.1%) |
|
Maxilla |
9 (40.9%) |
|
Tooth involved |
|
|
Anterior |
6 (27.3%) |
|
Premolar |
1 (4.5%) |
|
Molar |
15 (68.2%) |
|
Presence of root canal obturation |
|
|
Present |
12 (54.5%) |
|
Absent |
10 (45.5%) |
|
Axial distance of root apex to the affected cortex (mm) |
|
|
Median (IQR) |
3.9 (4.5) |
|
Range |
0.8–9.6 |
|
Axial distance of root apex to the non-affected cortex (mm) |
|
|
Median (IQR) |
8.4 (5.3) |
|
Range |
3.2–13.1 |
|
Volume of the periapical radiolucency (mm3) |
|
|
Median (IQR) |
388.6 (453.9) |
|
Range |
6.4–1997.4 |
|
Presence of cortical fenestration |
|
|
Present |
16 (72.7%) |
|
Absent |
6 (27.3%) |
|
Longest diameter of the periosteal reaction (mm) |
|
|
Median (IQR) |
9.9 (4.2) |
|
Range |
5.2–23.2 |
|
Periosteal reaction location |
|
|
Buccal |
16 (72.8%) |
|
Lingual/palatal |
6 (27.3%) |
|
Pattern of periosteal reaction |
|
|
Parallel |
20 (90.9%) |
|
Irregular |
2 (9.1%) |
|
Codman’s triangle |
0 (0%) |
|
Spicule |
0 (0%) |

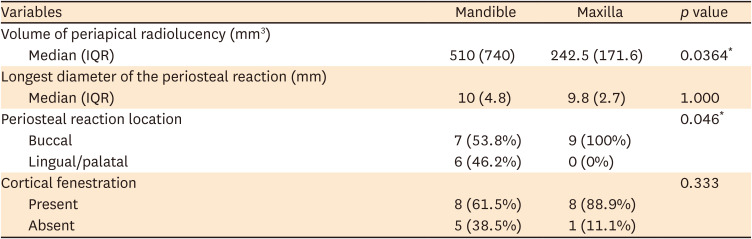
Table 2
The cross-tabulation of the radiographic findings based on the affected jaw
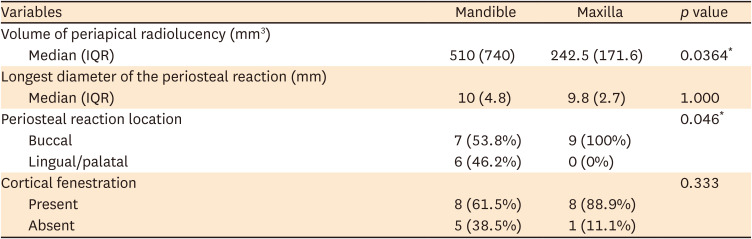
|
Variables |
Mandible |
Maxilla |
p value |
|
Volume of periapical radiolucency (mm3) |
|
|
|
|
Median (IQR) |
510 (740) |
242.5 (171.6) |
0.0364*
|
|
Longest diameter of the periosteal reaction (mm) |
|
|
|
|
Median (IQR) |
10 (4.8) |
9.8 (2.7) |
1.000 |
|
Periosteal reaction location |
|
|
0.046*
|
|
Buccal |
7 (53.8%) |
9 (100%) |
|
Lingual/palatal |
6 (46.2%) |
0 (0%) |
|
Cortical fenestration |
|
|
0.333 |
|
Present |
8 (61.5%) |
8 (88.9%) |
|
Absent |
5 (38.5%) |
1 (11.1%) |

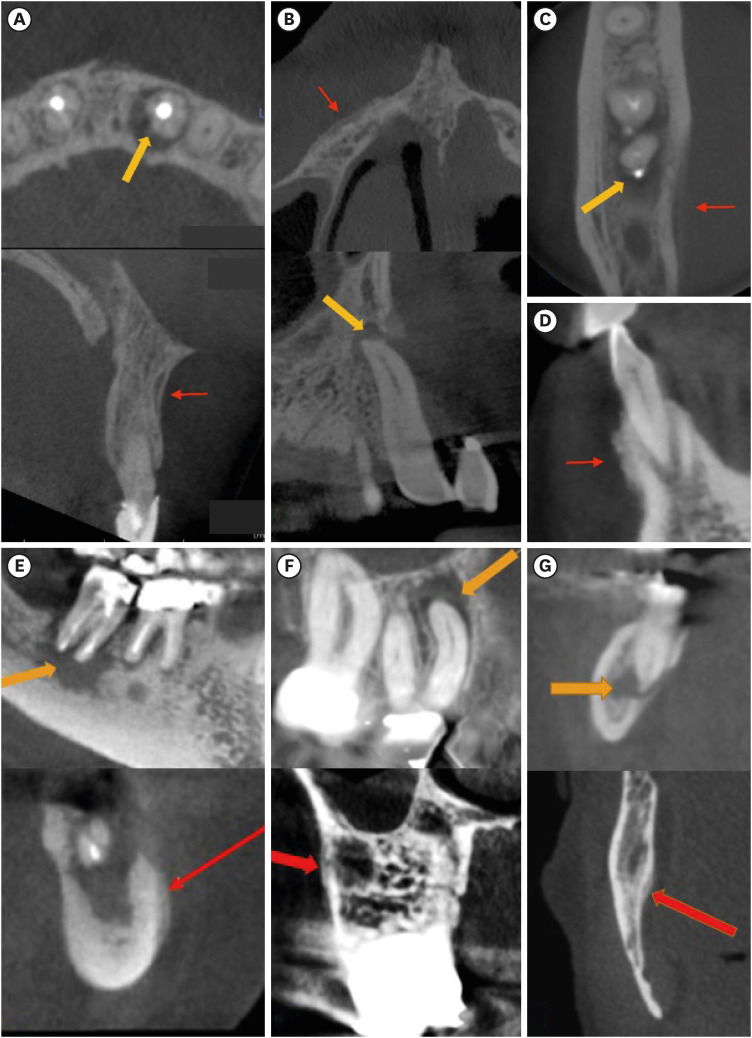
In all cases, periosteal bone reaction manifested as either parallel (90.9%) or irregular (9.1%). None of the cases showed a Codman's triangle or spicule pattern (
Figure 2).
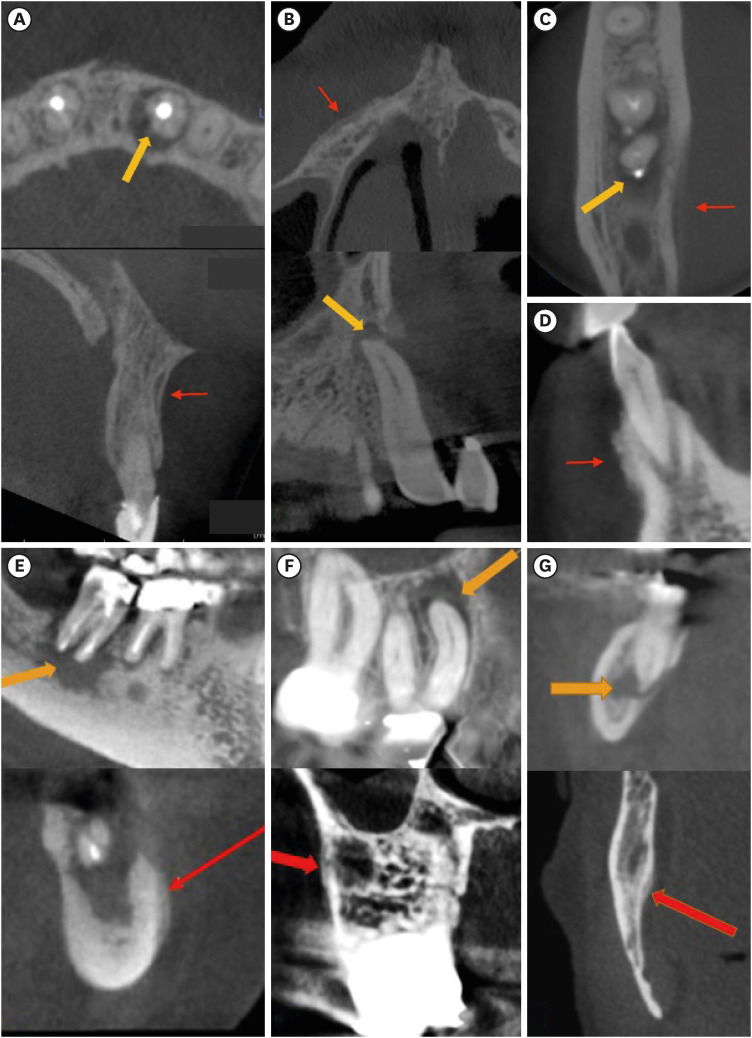 | Figure 2 Cone beam computed tomography images of 7 cases with periosteal reactions (red arrow) and periapical inflammatory lesion (yellow arrow). (A-C), (E-G) manifesting parallel periosteal reactions, and (D) showing irregular periosteal reaction.
|
In this cohort, 59% of the cases were located in the mandible, and the volume of AP/PARs was larger in the mandible compared to the maxilla (p = 0.0364). However, there was no statistically significant difference in the periosteal reaction's longest diameter between maxilla and mandible (p = 1.0000). Although a positive correlation was found between the volume of AP/PAR and periosteal reaction’s longest diameter, the relationship was very weak and not statistically significant (R = 0.0480, p = 0.8320). In addition, a weak positive correlation was found between the patient’s age and the longest diameter of periosteal reaction, and the correlation was not statistically significant (R = 0.0068, p = 0.9761).
Occurrence of periosteal reactions in the buccal cortex was more common in the maxilla (100%) compared to the mandible (53.8%) (p = 0.046). The periosteal reaction did not occur on the palatal side of any of the maxillary cases. The root apex of the involved teeth was significantly closer to the affected side (i.e., cortex with periosteal reaction) than the non-affected side (p = 0.0014).
Go to :

DISCUSSION
Periosteal bone reaction results from a cortical bone response to various insults. Understanding the different types of periosteal reactions and their subcategories aids clinicians in being more alert and cognizant of such types of patterns if and when presented with them. These reactions are broken down into different categories based on their nature of aggression as well as the speed with which they progress and develop [
2]. From a radiographic perspective, periosteal reactions tend to be identified incidentally when clinical signs and symptoms of odontogenic or non-odontogenic origin are experienced by the patient. It is possible that these reactions have rarely been recognized on radiographs because they are very fine and involve only a small area [
5]. A wide range of malignant tumors, inflammatory and infection-related etiologies in the jaws have the potential to lead to periosteal reaction [
7]. This study exclusively evaluated the periosteal reactions that are associated with endodontic lesions.
The periosteal reactions of all the cases in this study had a nonaggressive form (
i.e., parallel or irregular), and none of the lesions resulted in a periosteal response with Codman's triangle or a spicule pattern. This finding is consistent with the results of a study by Ida
et al. [
5], in which the aggressive forms (Codman’s triangle or spicule pattern) were mostly found in malignant tumors and trauma cases. They found that 43 out of 44 cases with osteomyelitis (98%) had either a parallel or irregular pattern, and only 1 showed a spicule pattern. This is also consistent with medical literature, where it was reported that nonaggressive forms of periosteal reaction are predominantly seen in benign, slow-growing lesions [
2]. In this study, although histopathologic evaluation was not performed in any of the cases, the pulpal diagnosis, together with the pattern of the periradicular radiolucency, are suggestive of lesions with an endodontic etiology.
In this study, cortical fenestration was absent in 27% of the cases. This shows that cortical fenestration is not necessary for the formation of periosteal reaction. This is consistent with a study by Jalali
et al. [
6] that showed acute apical abscess could occur in cases with the intact cortical bone. In that study, it was suggested that inflammation can spread through bone marrow, cortical micro-channels, lymphatics, or blood vessels. In addition, the findings showed that periosteal reactions were noted mostly on the buccal and were present 53.8% and 100% of the time in the mandible and maxilla, respectively. This is not surprising, as the root apices of the maxillary teeth are generally closer to the buccal cortex than the palatal cortex.
Through our evaluation, a significant correlation was not found between the patient's age and the longest diameter of periosteal reaction. Due to the small sample size and methodology of this study, the prevalence of periosteal reactions cannot be determined. In a study by Ida
et al. [
5] they found that the frequency of periosteal reactions was the highest in the osteomyelitis group, with an average age of 22 years old, followed by their malignant tumor group. Hayashi
et al. [
8] further support that osteomyelitis of the mandible is seen in younger patients. In their series, of 1,008 cases, only a small fraction above 11% had osteomyelitis with subsequent periosteal new bone formation. The proportion of periosteal new bone formation was greater among young patients and, to a lesser degree, apparent in patients 30 years or older. Therefore, this implies that patients of a young age are more prone to osteomyelitis of the mandible with periosteal new bone formation.
There is very limited literature on evaluating the periosteal bone reactions of endodontic origin. A few case reports by Bougatef
et al. [
9], Zand
et al. [
10], de Andrade Freitas Oliveria
et al. [
11], and Ebihara
et al. [
12] have discussed the occurrences of periosteal reactions associated with endodontic lesions. Each of their patients was a young adolescent that had presented with a chief complaint of swelling in the mandibular region. Upon radiographic evaluation, the teeth in question showed AP/PAR and an onion-skin appearance of the cortical plate in the area. In each of these case reports, after completion of endodontic treatment, the periapical radiographs showed a reduction of AP/PAR, and the occlusal films demonstrated resolution of the periosteal bone reaction. Therefore, based on these cases, clinical and radiographic interpretation is essential to better understand the evolution of these periosteal reactions. Additionally, as in de Andrade Freitas Oliveria
et al.’s case discussion [
11], a bone biopsy with histological analysis may also be helpful to confirm the diagnosis of such reactions.
Depending on the radiographic and clinical manifestations of the condition, the treatment plan can range from conservative to more invasive procedures. Regardless, early detection and elimination of the source of infection is highly recommended, and CBCT plays a valuable role in the early identification of periosteal reactions. A few case reports, as mentioned above, have demonstrated that endodontic treatment alone may be adequate to resolve the pathology. However, in cases where clinical signs and symptoms of osteomyelitis are present, a more aggressive treatment, including surgical drainage, microbiologic identification, and antibiotics, has been suggested to manage the infection [
4].
Within the confinements of this study, we recognize 3 aspects that limited our overall analysis. These were the bias in case selection (only the cases with an existing CBCT scan were included), the absence of histopathologic biopsy specimens, and the low number of cases.
Go to :

CONCLUSIONS
CBCT imaging is an effective tool for examining changes in the jaw structure and recognizing the pattern of periosteal bone reaction, which can help to differentiate between inflammatory lesions and malignant tumors. Clinical features should be considered to make an accurate diagnosis and provide the appropriate treatment. Further research is needed to understand the bony transformations potentially linked to endodontic lesions.
Go to :





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download