INTRODUCTION
MATERIALS AND METHODS
Search strategy
Eligibility criteria
• Population (P) – adult patients undergoing primary non-surgical endodontic treatment;
• Intervention (I) – different obturation techniques;
• Comparison (C) – cold lateral compaction technique;
• Outcome (O) – clinical and radiographic success rate;
• Study design (S) – randomized clinical trials, nonrandomized clinical trials, and longitudinal (prospective and retrospective) studies.
Selection of the studies
1. Data extraction
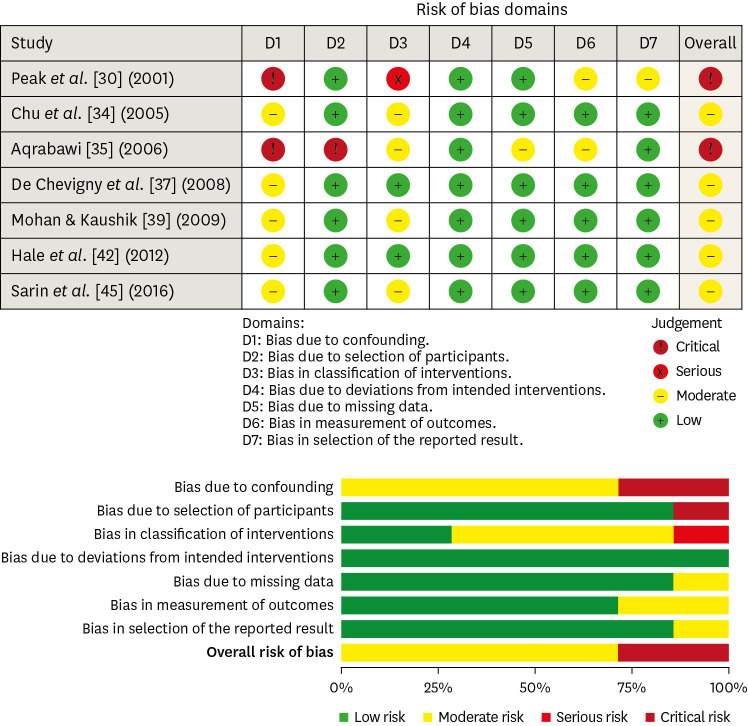
2. Risk of bias analysis
1) Confounding factors: ‘Low’ risk of bias was considered when all possible confounding factors were checked in the design or the statistical analysis. ‘Moderate’ risk of bias when some possible confounding factors were controlled. ‘Serious’ risk of bias when no possible confounding factors were controlled. ‘Critical’ risk of bias when possible confounding factors were not even discussed.
2) Selection of participants: ‘Low’ risk of bias was considered when all eligible participants were included in the study. ‘Moderate’ risk of bias when the participant selection may have been related to intervention/outcome. ‘Serious’ risk of bias when participant selection was related to intervention/outcome. ‘Critical’ risk of bias when the selection process was not described.
3) Classification of interventions: ‘Low’ risk of bias was considered when the chemo-mechanical preparation and obturation techniques were well described. ‘Moderate’ risk of bias when the chemo-mechanical preparation and obturation techniques presented some missing information, but the missing data were not relevant to the purpose of the included study. ‘Serious’ risk of bias when the chemo-mechanical preparation and obturation techniques were not well described. ‘Critical’ risk of bias when the chemo-mechanical preparation and obturation techniques were not described.
4) Deviations from intended interventions: ‘Low’ risk of bias was considered when no differences occurred after the beginning of the study, or differences in one or both groups occurred after the beginning of the study, but the participant continued (for analysis purposes) to be part of the study. ‘Moderate’ risk of bias when differences occurred after the beginning of the study, but it does not seem to affect its outcome. ‘Serious’ risk of bias when few differences occurred after the beginning of the study and changes in the sample or intervention were required. ‘Critical’ risk of bias when several differences occurred after the beginning of the study.
5) Missing data: ‘Low’ risk of bias was considered when the number of teeth evaluated per group, type of teeth, preparation technique, number of visits, obturation technique, follow-up time, and parameters evaluated to determine success were well reported. ‘Moderate’ risk of bias when there were some missing data, but the missing data were not relevant to the purpose of the included study. ‘Serious’ risk of bias when there were some relevant missing data. ‘Critical’ risk of bias when there were several relevant missing data
6) Measurement of outcomes: ‘Low’ risk of bias was considered when valid parameters (clinical and radiographic) were used to determine success. ‘Moderate’ risk of bias when using a valid methodology, but the methodology was not well described. ‘Serious’ risk of bias when a valid methodology was not used, but the methodology was well described. ‘Critical’ risk of bias when a valid methodology was not used, not well described, or the methodology used was not described.
7) Selection of described results: ‘Low’ risk of bias was considered when all results were presented. ‘Moderate’ risk of bias when results were reported but not well described. ‘Serious’ risk of bias when there was a substantial difference in the description of the results of each intervention. ‘Critical’ risk of bias when information is not presented.
3. Certainty of evidence
RESULTS
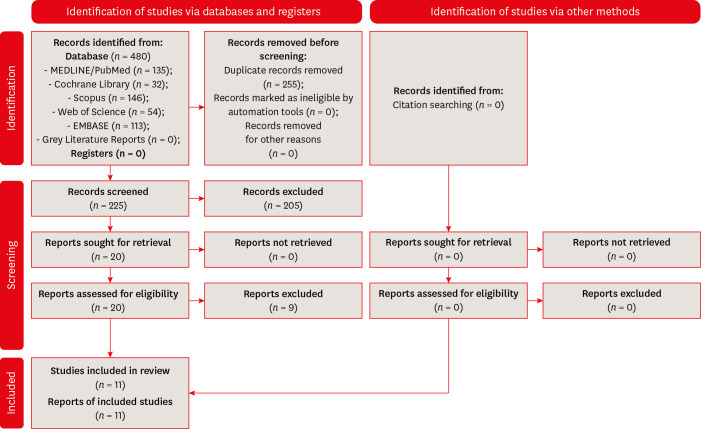
Study selection
Data extraction
Table 1
Characteristics of the included studies
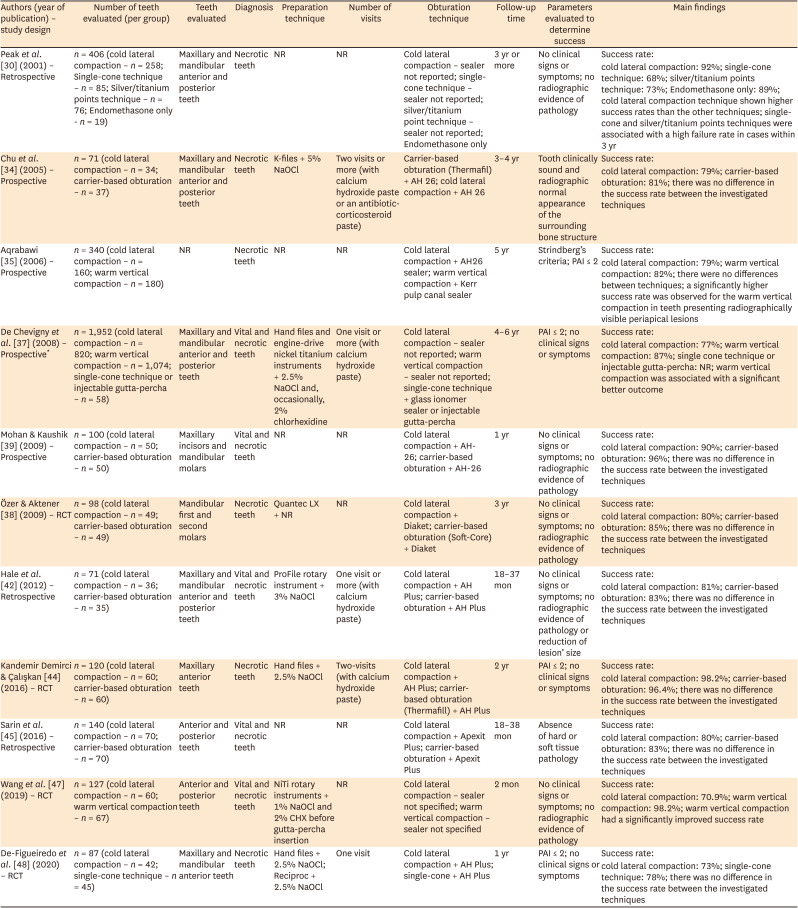
| Authors (year of publication) – study design | Number of teeth evaluated (per group) | Teeth evaluated | Diagnosis | Preparation technique | Number of visits | Obturation technique | Follow-up time | Parameters evaluated to determine success | Main findings |
|---|---|---|---|---|---|---|---|---|---|
| Peak et al. [30] (2001) – Retrospective | n = 406 (cold lateral compaction – n = 258; Single-cone technique – n = 85; Silver/titanium points technique – n = 76; Endomethasone only - n = 19) | Maxillary and mandibular anterior and posterior teeth | Necrotic teeth | NR | NR | Cold lateral compaction – sealer not reported; single-cone technique – sealer not reported; silver/titanium point technique – sealer not reported; Endomethasone only | 3 yr or more | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 92%; single-cone technique: 68%; silver/titanium points technique: 73%; Endomethasone only: 89%; cold lateral compaction technique shown higher success rates than the other techniques; single-cone and silver/titanium points techniques were associated with a high failure rate in cases within 3 yr | |||||||||
| Chu et al. [34] (2005) – Prospective | n = 71 (cold lateral compaction – n = 34; carrier-based obturation – n = 37) | Maxillary and mandibular anterior and posterior teeth | Necrotic teeth | K-files + 5% NaOCl | Two visits or more (with calcium hydroxide paste or an antibiotic-corticosteroid paste) | Carrier-based obturation (Thermafil) + AH 26; cold lateral compaction + AH 26 | 3–4 yr | Tooth clinically sound and radiographic normal appearance of the surrounding bone structure | Success rate: |
| cold lateral compaction: 79%; carrier-based obturation: 81%; there was no difference in the success rate between the investigated techniques | |||||||||
| Aqrabawi [35] (2006) – Prospective | n = 340 (cold lateral compaction – n = 160; warm vertical compaction – n = 180) | NR | Necrotic teeth | NR | NR | Cold lateral compaction + AH26 sealer; warm vertical compaction + Kerr pulp canal sealer | 5 yr | Strindberg’s criteria; PAI ≤ 2 | Success rate: |
| cold lateral compaction: 79%; warm vertical compaction: 82%; there were no differences between techniques; a significantly higher success rate was observed for the warm vertical compaction in teeth presenting radiographically visible periapical lesions | |||||||||
| De Chevigny et al. [37] (2008) – Prospective* | n = 1,952 (cold lateral compaction – n = 820; warm vertical compaction – n = 1,074; single-cone technique or injectable gutta-percha – n = 58) | Maxillary and mandibular anterior and posterior teeth | Vital and necrotic teeth | Hand files and engine-drive nickel titanium instruments + 2.5% NaOCl and, occasionally, 2% chlorhexidine | One visit or more (with calcium hydroxide paste) | Cold lateral compaction – sealer not reported; warm vertical compaction – sealer not reported; single-cone technique + glass ionomer sealer or injectable gutta-percha | 4–6 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: |
| cold lateral compaction: 77%; warm vertical compaction: 87%; single cone technique or injectable gutta-percha: NR; warm vertical compaction was associated with a significant better outcome | |||||||||
| Mohan & Kaushik [39] (2009) – Prospective | n = 100 (cold lateral compaction – n = 50; carrier-based obturation – n = 50) | Maxillary incisors and mandibular molars | Vital and necrotic teeth | NR | NR | Cold lateral compaction + AH-26; carrier-based obturation + AH-26 | 1 yr | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 90%; carrier-based obturation: 96%; there was no difference in the success rate between the investigated techniques | |||||||||
| Özer & Aktener [38] (2009) – RCT | n = 98 (cold lateral compaction – n = 49; carrier-based obturation – n = 49) | Mandibular first and second molars | Necrotic teeth | Quantec LX + NR | NR | Cold lateral compaction + Diaket; carrier-based obturation (Soft-Core) + Diaket | 3 yr | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 80%; carrier-based obturation: 85%; there was no difference in the success rate between the investigated techniques | |||||||||
| Hale et al. [42] (2012) – Retrospective | n = 71 (cold lateral compaction – n = 36; carrier-based obturation – n = 35) | Maxillary and mandibular anterior and posterior teeth | Vital and necrotic teeth | ProFile rotary instrument + 3% NaOCl | One visit or more (with calcium hydroxide paste) | Cold lateral compaction + AH Plus; carrier-based obturation + AH Plus | 18–37 mon | No clinical signs or symptoms; no radiographic evidence of pathology or reduction of lesion’ size | Success rate: |
| cold lateral compaction: 81%; carrier-based obturation: 83%; there was no difference in the success rate between the investigated techniques | |||||||||
| Kandemir Demirci & Çalışkan [44] (2016) – RCT | n = 120 (cold lateral compaction – n = 60; carrier-based obturation – n = 60) | Maxillary anterior teeth | Necrotic teeth | Hand files + 2.5% NaOCl | Two-visits (with calcium hydroxide paste) | Cold lateral compaction + AH Plus; carrier-based obturation (Thermafill) + AH Plus | 2 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: |
| cold lateral compaction: 98.2%; carrier-based obturation: 96.4%; there was no difference in the success rate between the investigated techniques | |||||||||
| Sarin et al. [45] (2016) – Retrospective | n = 140 (cold lateral compaction – n = 70; carrier-based obturation – n = 70) | Anterior and posterior teeth | Vital and necrotic teeth | NR | NR | Cold lateral compaction + Apexit Plus; carrier-based obturation + Apexit Plus | 18–38 mon | Absence of hard or soft tissue pathology | Success rate: |
| cold lateral compaction: 80%; carrier-based obturation: 83%; there was no difference in the success rate between the investigated techniques | |||||||||
| Wang et al. [47] (2019) – RCT | n = 127 (cold lateral compaction – n = 60; warm vertical compaction – n = 67) | Anterior and posterior teeth | Vital and necrotic teeth | NiTi rotary instruments + 1% NaOCl and 2% CHX before gutta-percha insertion | NR | Cold lateral compaction – sealer not specified; warm vertical compaction – sealer not specified | 2 mon | No clinical signs or symptoms; no radiographic evidence of pathology | Success rate: |
| cold lateral compaction: 70.9%; warm vertical compaction: 98.2%; warm vertical compaction had a significantly improved success rate | |||||||||
| De-Figueiredo et al. [48] (2020) – RCT | n = 87 (cold lateral compaction – n = 42; single-cone technique – n = 45) | Maxillary and mandibular anterior teeth | Necrotic teeth | Hand files + 2.5% NaOCl; Reciproc + 2.5% NaOCl | One visit | Cold lateral compaction + AH Plus; single-cone + AH Plus | 1 yr | PAI ≤ 2; no clinical signs or symptoms | Success rate: |
| cold lateral compaction: 73%; single-cone technique: 78%; there was no difference in the success rate between the investigated techniques |
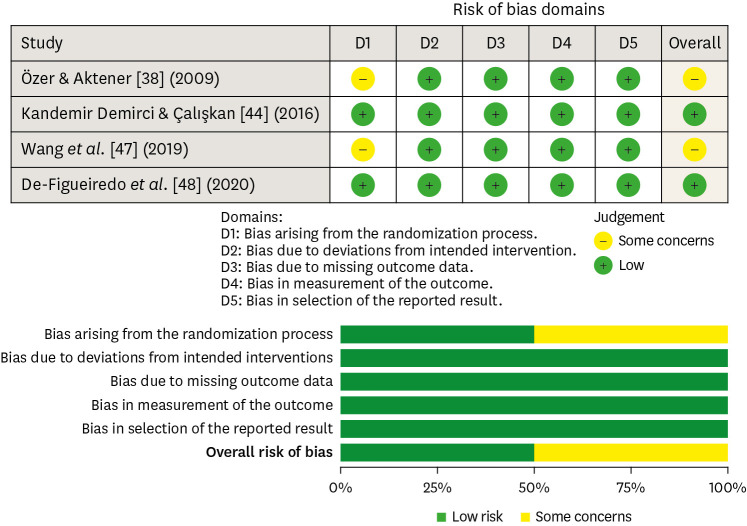
Quality assessment
Strength of evidence
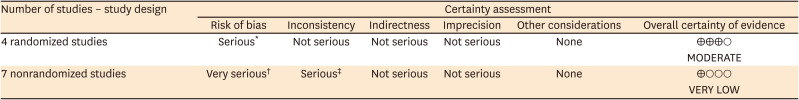
Table 2
Certainty of the evidence of the included studies




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download