1. Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021; 397(10278):1023–1034. PMID:
33587887.

2. Romer D, Winneg KM, Jamieson PE, Brensinger C, Jamieson KH. Misinformation about vaccine safety and uptake of COVID-19 vaccines among adults and 5-11-year-olds in the United States. Vaccine. 2022; 40(45):6463–6470. PMID:
36192273.

3. Song I, Lee SH. COVID-19 vaccine refusal associated with health literacy: findings from a population-based survey in Korea. BMC Public Health. 2023; 23(1):255. PMID:
36747179.

4. de Figueiredo A, Simas C, Larson HJ. COVID-19 vaccine acceptance and its socio-demographic and emotional determinants: a multi-country cross-sectional study. Vaccine. 2023; 41(2):354–364. PMID:
36414475.

5. Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022; 22(9):1293–1302. PMID:
35753318.

6. Lip A, Pateman M, Fullerton MM, Chen HM, Bailey L, Houle S, et al. Vaccine hesitancy educational tools for healthcare providers and trainees: a scoping review. Vaccine. 2023; 41(1):23–35. PMID:
36437208.

7. Whitehead HS, French CE, Caldwell DM, Letley L, Mounier-Jack S. A systematic review of communication interventions for countering vaccine misinformation. Vaccine. 2023; 41(5):1018–1034. PMID:
36628653.

8. Gesser-Edelsburg A, Diamant A, Hijazi R, Mesch GS. Correcting misinformation by health organizations during measles outbreaks: a controlled experiment. PLoS One. 2018; 13(12):e0209505. PMID:
30566485.

9. Jeon M, Kim J, Oh CE, Lee JY. Adverse events following immunization associated with coronavirus disease 2019 vaccination reported in the mobile vaccine adverse events reporting system. J Korean Med Sci. 2021; 36(17):e114. PMID:
33942578.

10. Excler JL, Saville M, Berkley S, Kim JH. Vaccine development for emerging infectious diseases. Nat Med. 2021; 27(4):591–600. PMID:
33846611.

11. Zhang Z, Shen Q, Chang H. Vaccines for COVID-19: a systemic review of immunogenicity, current development, and future prospects. Front Immunol. 2022; 13:843928. PMID:
35572592.

12. Ford A, Hwang A, Mo AX, Baqar S, Touchette N, Deal C, et al. Meeting summary: global vaccine and immunization research forum, 2021. Vaccine. 2023; 41(11):1799–1807. PMID:
36803897.

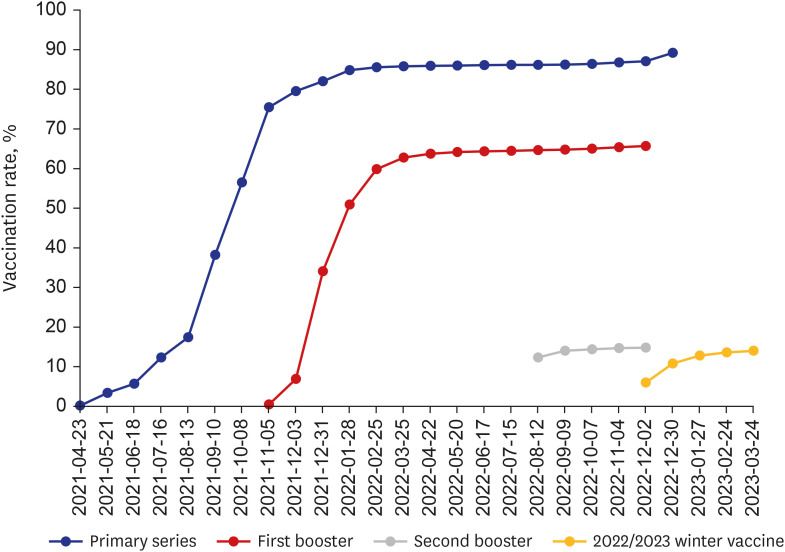
13. Nham E, Song JY, Noh JY, Cheong HJ, Kim WJ. COVID-19 vaccination in Korea: past, present, and the way forward. J Korean Med Sci. 2022; 37(47):e351. PMID:
36472087.

14. Jamieson KH, Romer D, Jamieson PE, Winneg KM, Pasek J. The role of non-COVID-specific and COVID-specific factors in predicting a shift in willingness to vaccinate: a panel study. Proc Natl Acad Sci U S A. 2021; 118(52):e2112266118. PMID:
34930844.

15. Jung J. Preparing for the coronavirus disease (COVID-19) vaccination: evidence, plans, and implications. J Korean Med Sci. 2021; 36(7):e59. PMID:
33619920.

16. Thompson KM, Gellin BG, Hinman AR, Orenstein WA. The national vaccine advisory committee at 30: Impact and opportunity. Vaccine. 2018; 36(11):1330–1344. PMID:
29422369.

17. Choi YY, Kim MK, Kwon HC, Kim GH. Safety monitoring after the BNT162b2 COVID-19 vaccine among adults aged 75 years or older. J Korean Med Sci. 2021; 36(45):e318. PMID:
34811980.

18. García-Grimshaw M, Ceballos-Liceaga SE, Hernández-Vanegas LE, Núñez I, Hernández-Valdivia N, Carrillo-García DA, et al. Neurologic adverse events among 704,003 first-dose recipients of the BNT162b2 mRNA COVID-19 vaccine in Mexico: a nationwide descriptive study. Clin Immunol. 2021; 229:108786. PMID:
34147649.

19. SeyedAlinaghi S, Karimi A, Pashaei Z, Afzalian A, Mirzapour P, Ghorbanzadeh K, et al. Safety and adverse events related to COVID-19 mRNA vaccines; a systemic review. Arch Acad Emerg Med. 2022; 10(1):e41. PMID:
35765616.
20. Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risk of myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by age and sex. Circulation. 2022; 146(10):743–754. PMID:
35993236.

21. Link-Gelles R, Weber ZA, Reese SE, Payne AB, Gaglani M, Adams K, et al. Estimates of bivalent mRNA vaccine durability in preventing COVID-19-Associated hospitalization and critical illness among adults with and without immunocompromising conditions — VISION Network, September 2022–April 2023. MMWR Morb Mortal Wkly Rep. 2023; 72(21):579–588. PMID:
37227984.

22. Tenforde MW, Weber ZA, Natarajan K, Klein NP, Kharbanda AB, Stenehjem E, et al. Early estimates of bivalent mRNA vaccine effectiveness in preventing COVID-19-associated emergency department or urgent care encounters and hospitalizations among immunocompetent adults—VISION Network, Nine States, September–November 2022. MMWR Morb Mortal Wkly Rep. 2023; 71(53):1637–1646. PMID:
36921274.
23. Nham E, Kim YE, Jung J, Kim DW, Jang H, Hyun H, et al. COVID-19 vaccination rates in patients with chronic medical conditions: a nationwide cross-sectional study. J Korean Med Sci. 2022; 37(45):e325. PMID:
36413798.

24. Shin A, Kim DW, Kim YE, Kim DR, Jung J, Kim YJ. COVID-19 vaccination status among Korean pediatric population with comorbidities. J Korean Med Sci. 2023; 38(32):e248. PMID:
37582498.

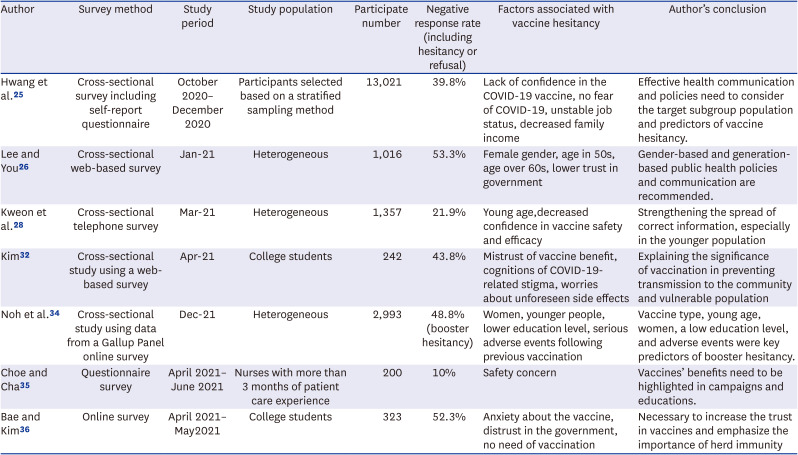
25. Hwang SE, Kim WH, Heo J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum Vaccin Immunother. 2022; 18(1):1–8.

26. Lee M, You M. Direct and indirect associations of media use with COVID-19 vaccine hesitancy in South Korea: cross-sectional web-based survey. J Med Internet Res. 2022; 24(1):e32329. PMID:
34870605.

27. Pires C. Global predictors of COVID-19 vaccine hesitancy: a systemic review. Vaccines (Basel). 2022; 10(8):1349. PMID:
36016237.
28. Kweon SS, Yun I, Choi C, Ryu SY, Cho JH, Shin MH. Factors associated with COVID-19 vaccine hesitancy in Korea. Chonnam Med J. 2022; 58(1):43–47. PMID:
35169559.

29. Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016; 34(52):6700–6706. PMID:
27810314.

30. Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. Am J Transplant. 2021; 21(4):1650–1656. PMID:
33788992.

31. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015; 33(34):4161–4164. PMID:
25896383.

32. Kim JS. Association of COVID-19 vaccine attitudes and cognitions of COVID-19-related stigma with vaccine hesitancy among college students. J Korean Acad Soc Nurs Educ. 2022; 28(3):296–304.

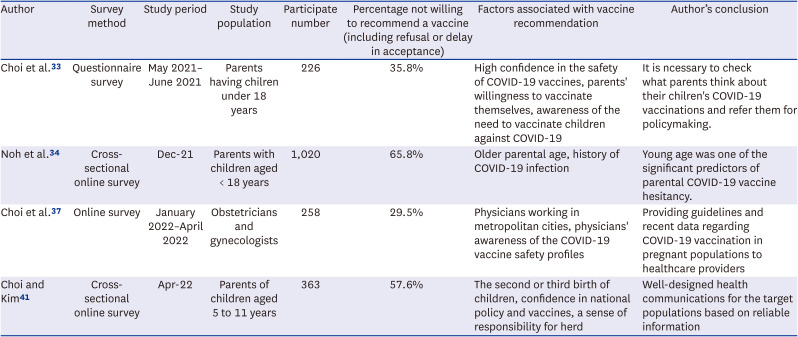
33. Choi SH, Jo YH, Jo KJ, Park SE. Pediatric and parents’ attitudes towards COVID-19 vaccines and intention to vaccinate for children. J Korean Med Sci. 2021; 36(31):e227. PMID:
34402237.

34. Noh Y, Kim JH, Yoon D, Choe YJ, Choe SA, Jung J, et al. Predictors of COVID-19 booster vaccine hesitancy among fully vaccinated adults in Korea: a nationwide cross-sectional survey. Epidemiol Health. 2022; 44:e2022061. PMID:
35914771.

35. Choe YH, Cha J. Factors influencing clinical nurse’s intention for acquiring coronavirus disease 2019 vaccination. J Health Info Stat. 2022; 47(1):48–56.

36. Bae S, Kim HJ. Influencing factors of COVID-19 vaccination intention among college students: based on Andersen’s model. J Korean Public Health Nurs. 2021; 35(3):384–400.
37. Choi BY, Yoon H, Seong WJ, Cho GJ, Na S, Jung YM, et al. Knowledge and acceptability of the COVID-19 vaccine among obstetricians and gynecologists in Korea, and factors affecting its recommendation in the pregnant population. J Korean Soc Matern Child Health. 2022; 26(4):245–253.

38. Peterson CJ, Lee B, Nugent K. COVID-19 vaccination hesitancy among healthcare workers—a review. Vaccines (Basel). 2022; 10(6):948. PMID:
35746556.

39. Janssen C, Maillard A, Bodelet C, Claudel AL, Gaillat J, Delory T, et al. Hesitancy towards COVID-19 vaccination among healthcare workers: a multi-centric survey in France. Vaccines (Basel). 2021; 9(6):547. PMID:
34067490.

40. Toth-Manikowski SM, Swirsky ES, Gandhi R, Piscitello G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. Am J Infect Control. 2022; 50(1):20–25. PMID:
34653527.

41. Choi IS, Kim EA. Factors influencing the COVID-19 vaccination intentions in parents for their children aged 5~11: Korea, April 2022. J Korean Acad Nurs. 2023; 53(2):208–221. PMID:
37164348.

42. Tan LJ, Koh CP, Lai SK, Poh WC, Othman MS, Hussin H. A systemic review and recommendation for an autopsy approach to death followed the COVID 19 vaccination. Forensic Sci Int. 2022; 340:111469. PMID:
36162300.

43. Yoon D, Jeon HL, Noh Y, Choe YJ, Choe SA, Jung J, et al. A nationwide survey of mRNA COVID-19 vaccinee’s experiences on adverse events and its associated factors. J Korean Med Sci. 2023; 38(22):e170. PMID:
37272559.

44. Lu X, Masuda S, Horlad H, Katoh T. Safety and adverse effects of the coronavirus disease 2019 vaccine among the general Japanese adult population. Vaccine. 2023; 41(35):5090–5096. PMID:
37455163.

45. Kahn AL, Steffen CA, Henaff L, MacDonald NE, Morgan C, Faden R, et al. COVID-19 vaccine policy development in a sample of 44 countries - key findings from a December 2021 survey of National Immunization Technical Advisory Groups (NITAGs). Vaccine. 2023; 41(3):676–683. PMID:
36494252.

46. MacDonald NE, Dube E, Comeau JL. Have vaccine hesitancy models oversimplified a complex problem to our detriment? The Adapted Royal Society of Canada vaccine uptake framework. Vaccine. 2022; 40(29):3927–3930. PMID:
35637069.

47. Canning AG, Watson KE, McCreedy KE, Olawepo JO. Ethics and effectiveness of US COVID-19 vaccine mandates and vaccination passports: a review. J Res Health Sci. 2022; 22(2):e00546. PMID:
36511258.

48. Bardosh K, de Figueiredo A, Gur-Arie R, Jamrozik E, Doidge J, Lemmens T, et al. The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good. BMJ Glob Health. 2022; 7(5):e008684.

49. Fishman J, Mandell DS, Salmon MK, Candon M. Large and small financial incentives may motivate COVID-19 vaccination: a randomized, controlled survey experiment. PLoS One. 2023; 18(3):e0282518. PMID:
36930588.

50. Skafle I, Nordahl-Hansen A, Quintana DS, Wynn R, Gabarron E. Misinformation about COVID-19 vaccines on social media: rapid review. J Med Internet Res. 2022; 24(8):e37367. PMID:
35816685.

51. Mohamed K, Rzymski P, Islam MS, Makuku R, Mushtaq A, Khan A, et al. COVID-19 vaccinations: the unknowns, challenges, and hopes. J Med Virol. 2022; 94(4):1336–1349. PMID:
34845731.

52. Colosi E, Bassignana G, Contreras DA, Poirier C, Boëlle PY, Cauchemez S, et al. Screening and vaccination against COVID-19 to minimise school closure: a modelling study. Lancet Infect Dis. 2022; 22(7):977–989. PMID:
35378075.

53. Fontanet A, Cauchemez S. COVID-19 herd immunity: where are we? Nat Rev Immunol. 2020; 20(10):583–584. PMID:
32908300.

54. McDermott A. Core concept: Herd immunity is an important-and often misunderstood-public health phenomenon. Proc Natl Acad Sci U S A. 2021; 118(21):e2107692118. PMID:
34011611.

55. Wang CW, de Jong EP, Faure JA, Ellington JL, Chen CS, Chan CC. A matter of trust: a qualitative comparison of the determinants of COVID-19 vaccine hesitancy in Taiwan, the United States, the Netherlands, and Haiti. Hum Vaccin Immunother. 2022; 18(5):2050121. PMID:
35349382.

56. Geisen UM, Berner DK, Tran F, Sümbül M, Vullriede L, Ciripoi M, et al. Immunogenicity and safety of anti-SARS-CoV-2 mRNA vaccines in patients with chronic inflammatory conditions and immunosuppressive therapy in a monocentric cohort. Ann Rheum Dis. 2021; 80(10):1306–1311. PMID:
33762264.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download