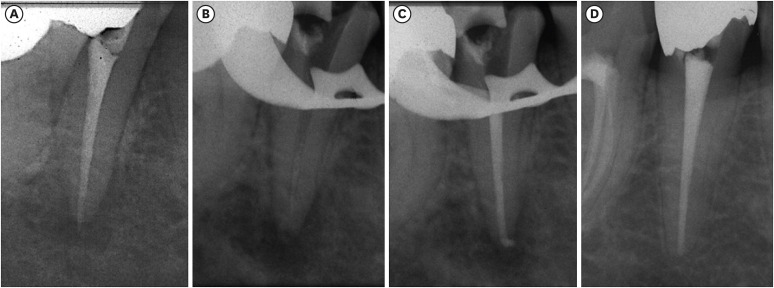
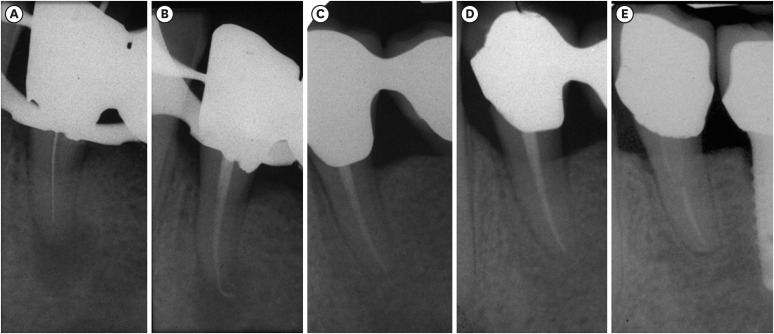
Four patients were referred for the evaluation and treatment of a lower right second premolar (
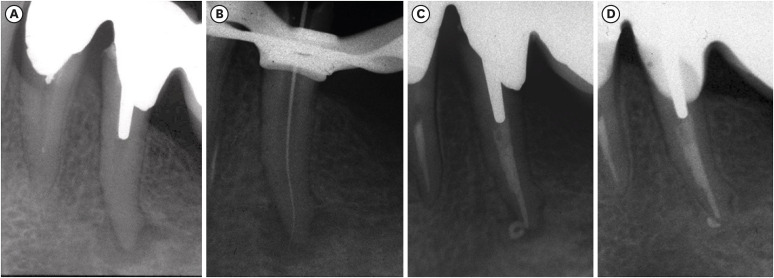
Figure 1A-1D), a lower left second premolar (
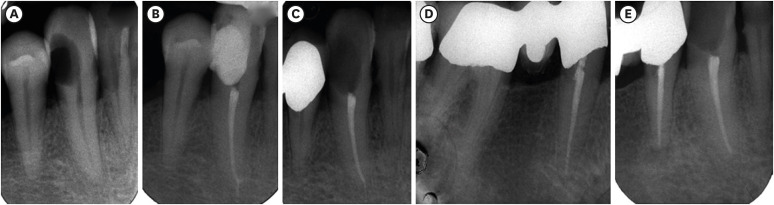
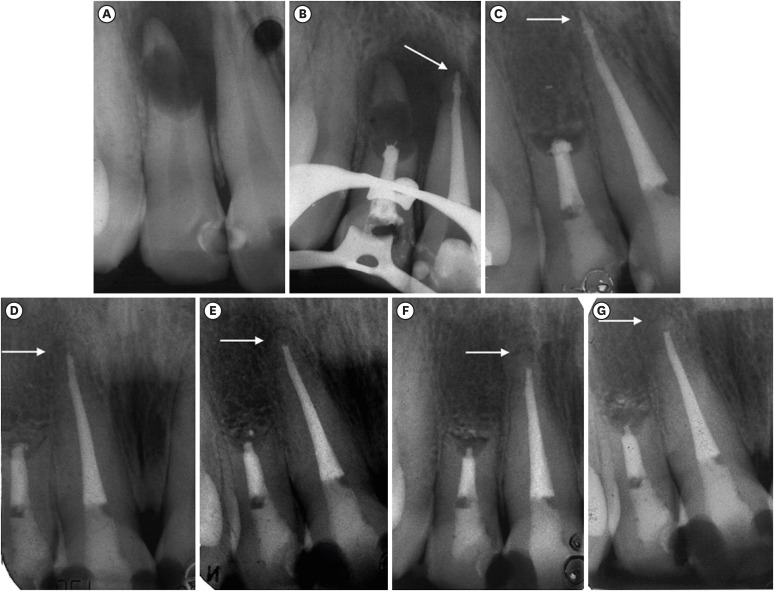
Figure 2A-2D), a lower right canine and first premolar (
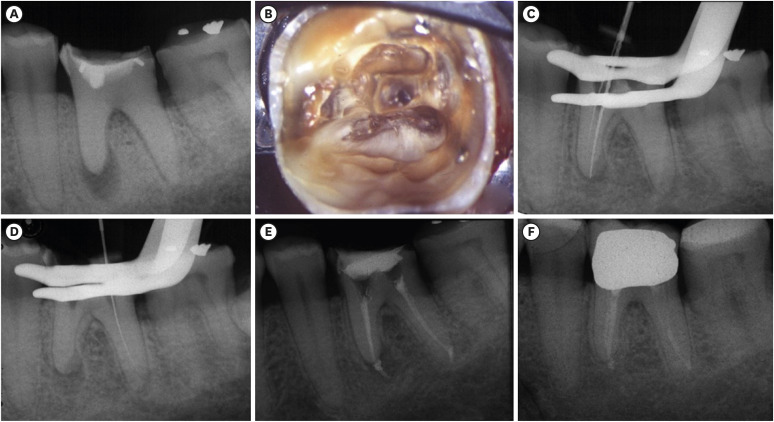
Figure 3A-3E), and a lower left first molar (
Figure 4A-4F), respectively. The preoperative radiographs of all cases (
Figures 1A,
2A, and
4A) showed the presence of a periapical radiolucency, except for 1 (
Figure 3A). It was re-treated in only 1 case (
Figure 1A). In all clinical cases, after rubber dam isolation, the old restorations and root canal filling materials, if present, were removed (
Figure 1B). The pulp chamber was opened using high-speed rotating diamond-coated burs and the root canal orifices were located using low-speed carbide burs and/or endodontic ultrasonic tips under magnification using a dental operating microscope (
Figure 4B). After the scouting phase and establishing the working length (
Figures 2B,
4C, and 4D), all root canals were shaped using Mtwo instruments (VDW, Munich, Germany) using the simultaneous technique, irrigated with 5% sodium hypochlorite (NaOCl) alternating with 17% ethylenediaminetetraacetic acid (EDTA) and finally obturated with warm preheated thermoplasticized gutta-percha (MicroFlow, Microseal system, Sybron Endo, Orange, CA, USA), and sealer corresponding to Rickert's formula (Pulp Canal Sealer, Sybron Endo) according to the hybrid Microseal/PacMac obturation technique refined by 1 of the authors of the presented cases [
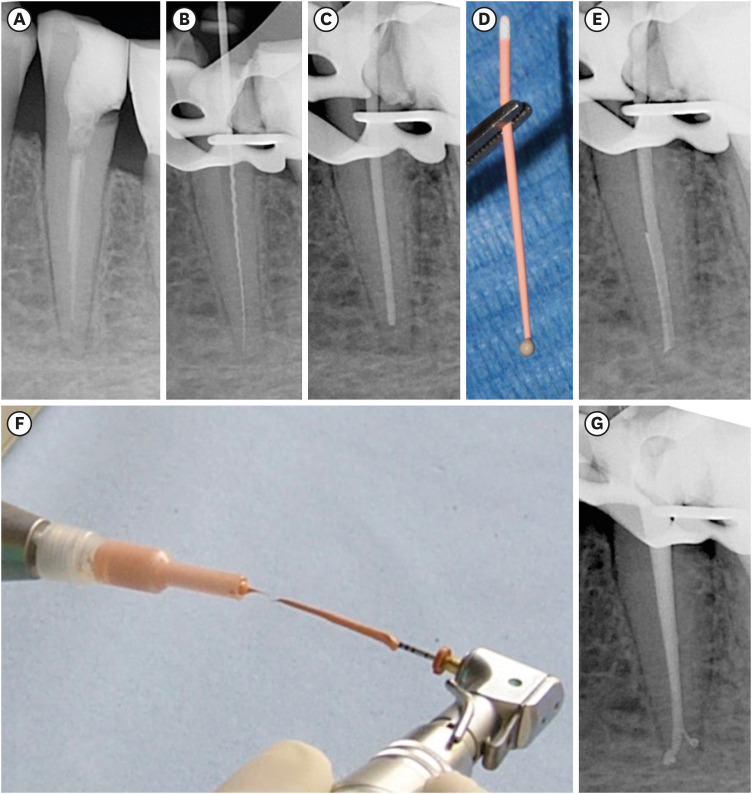
10]. The Microseal obturation technique involves the use of preheated gutta-percha inserted inside the root canal, applied on a conical ISO 25 0.04 PacMac (Sybron Endo) introduced up to 2–3 mm from the apex, and activated at 6,000–7,000 rpm (
Figure 5A-5G). The first to describe this technique in 1993 was John T. McSpadden [
11], who referred to it as the multiphase gutta-percha obturation technique. Since then, some modifications have been made to this technique, which was later named Microseal [
1213], such as the use of a 0.2 tapered gutta-percha master cone brought to 1 mm from the working length to limit overfilling [
10]. The quantity of sealer used in the Microseal technique is very minimal; the master cone of gutta-percha only gets dirty at the tip (
Figure 5D), and the canal is filled by the preheated preplasticized gutta-percha applied to the PacMac instrument (
Figure 5F-5G).
Overfilling occurred during obturation in all cases (
Figures 1C,
2C,
3B, and
4E), but the radiographic follow-up at 10 years showed complete or almost complete resorption of the filling material beyond the apex and healing of the periapical lesions or maintenance of healthy periapical status (
Figures 1D,
2D,
3E canine, and
4F). Radiographic follow-up (
Figure 3E) showed healing of the lower canine restored with radiolucent composite resin, but also a periapical lesion on the first lower right premolar contiguous to the canine, part of the porcelain-fused-to-metal (PFM) bridge, where 5 years earlier slightly short canal filling was performed (
Figure 3C and 3D).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download