1. Cheung W. A review of the management of endodontically treated teeth. Post, core and the final restoration. J Am Dent Assoc. 2005; 136:611–619. PMID:
15966648.
2. Scotti N, Eruli C, Comba A, Paolino DS, Alovisi M, Pasqualini D, Berutti E. Longevity of class 2 direct restorations in root-filled teeth: a retrospective clinical study. J Dent. 2015; 43:499–505. PMID:
25701467.

3. Mosharraf R, Ranjbarian P. Effects of post surface conditioning before silanization on bond strength between fiber post and resin cement. J Adv Prosthodont. 2013; 5:126–132. PMID:
23755337.

4. Novais VR, Simamotos Júnior PC, Rontani RM, Correr-Sobrinho L, Soares CJ. Bond strength between fiber posts and composite resin core: influence of temperature on silane coupling agents. Braz Dent J. 2012; 23:8–14. PMID:
22460308.

5. Fernandes AS, Shetty S, Coutinho I. Factors determining post selection: a literature review. J Prosthet Dent. 2003; 90:556–562. PMID:
14668756.

6. Faria AC, Rodrigues RC, de Almeida Antunes RP, de Mattos MG, Ribeiro RF. Endodontically treated teeth: characteristics and considerations to restore them. J Prosthodont Res. 2011; 55:69–74. PMID:
20709618.

7. Sequeira-Byron P, Fedorowicz Z, Carter B, Nasser M, Alrowaili EF. Single crowns versus conventional fillings for the restoration of root-filled teeth. Cochrane Database Syst Rev. 2015; 2015:CD009109.

8. Liu C, Liu H, Qian YT, Zhu S, Zhao SQ. The influence of four dual-cure resin cements and surface treatment selection to bond strength of fiber post. Int J Oral Sci. 2014; 6:56–60. PMID:
24177170.

9. Murali Mohan S, Mahesh Gowda E, Shashidhar MP. Clinical evaluation of the fiber post and direct composite resin restoration for fixed single crowns on endodontically treated teeth. Med J Armed Forces India. 2015; 71:259–264. PMID:
26288494.

10. Naumann M, Blankenstein F, Dietrich T. Survival of glass fibre reinforced composite post restorations after 2 years—an observational clinical study. J Dent. 2005; 33:305–312. PMID:
15781138.

11. Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004; 30:289–301. PMID:
15107639.

12. Abduljabbar T, Sherfudhin H, AlSaleh SA, Al-Helal AA, Al-Orini SS, Al-Aql NA. Fracture resistance of three post and core systems in endodontically treated teeth restored with all-ceramic crowns. King Saud Univ J Dent Sci. 2012; 3:33–38.

13. Ree M, Schwartz RS. The endo-restorative interface: current concepts. Dent Clin North Am. 2010; 54:345–374. PMID:
20433982.

14. Naumann M, Blankenstein F, Kiessling S, Dietrich T. Risk factors for failure of glass fiber-reinforced composite post restorations: a prospective observational clinical study. Eur J Oral Sci. 2005; 113:519–524. PMID:
16324143.

15. Ghavamnasiri M, Maleknejad F, Ameri H, Moghaddas MJ, Farzaneh F, Chasteen JE. A retrospective clinical evaluation of success rate in endodontic-treated premolars restored with composite resin and fiber reinforced composite posts. J Conserv Dent. 2011; 14:378–382. PMID:
22144807.

16. Parisi C, Valandro LF, Ciocca L, Gatto MR, Baldissara P. Clinical outcomes and success rates of quartz fiber post restorations: a retrospective study. J Prosthet Dent. 2015; 114:367–372. PMID:
26013066.

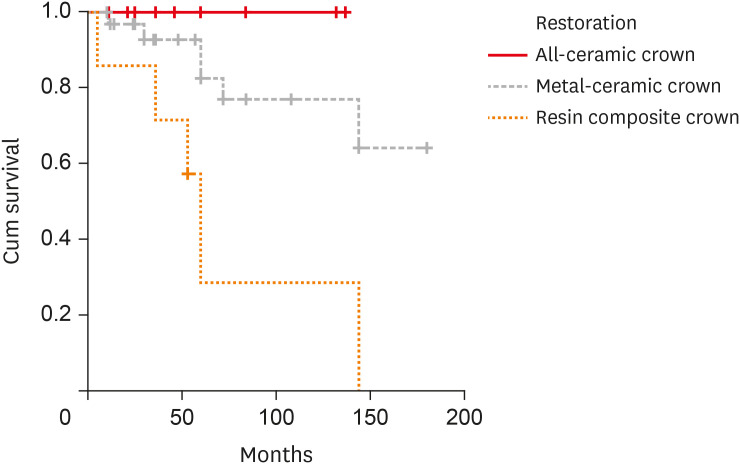
17. Skupien JA, Cenci MS, Opdam NJ, Kreulen CM, Huysmans MC, Pereira-Cenci T. Crown vs. composite for post-retained restorations: a randomized clinical trial. J Dent. 2016; 48:34–39. PMID:
26976553.

18. Barabanti N, Preti A, Vano M, Derchi G, Mangani F, Cerutti A. Indirect composite restorations luted with two different procedures: a ten years follow up clinical trial. J Clin Exp Dent. 2015; 7:e54–e59. PMID:
25810842.

19. Etman MK, Woolford MJ. Three-year clinical evaluation of two ceramic crown systems: a preliminary study. J Prosthet Dent. 2010; 103:80–90. PMID:
20141812.

20. Ryge G. Clinical criteria. Int Dent J. 1980; 30:347–358. PMID:
6935165.
21. Ferrari M, Vichi A, García-Godoy F. Clinical evaluation of fiber-reinforced epoxy resin posts and cast post and cores. Am J Dent. 2000; 13:15B–18B.
22. Ferrari M, Vichi A, Mannocci F, Mason PN. Retrospective study of the clinical performance of fiber posts. Am J Dent. 2000; 13:9B–13B.
23. Weigl P, Sander A, Wu Y, Felber R, Lauer HC, Rosentritt M.
In-vitro performance and fracture strength of thin monolithic zirconia crowns. J Adv Prosthodont. 2018; 10:79–84. PMID:
29713427.

24. Ferrari M, Cagidiaco MC, Goracci C, Vichi A, Mason PN, Radovic I, Tay F. Long-term retrospective study of the clinical performance of fiber posts. Am J Dent. 2007; 20:287–291. PMID:
17993023.
25. Schmitter M, Rammelsberg P, Gabbert O, Ohlmann B. Influence of clinical baseline findings on the survival of 2 post systems: a randomized clinical trial. Int J Prosthodont. 2007; 20:173–178. PMID:
17455439.
26. Gutmann JL. The dentin-root complex: anatomic and biologic considerations in restoring endodontically treated teeth. J Prosthet Dent. 1992; 67:458–467. PMID:
1507126.

27. Panitvisai P, Messer HH. Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod. 1995; 21:57–61. PMID:
7714437.

28. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992; 18:332–335. PMID:
1402595.

29. Figueiredo FE, Martins-Filho PR, Faria-E-Silva AL. Do metal post-retained restorations result in more root fractures than fiber post-retained restorations? A systematic review and meta-analysis. J Endod. 2015; 41:309–316. PMID:
25459568.

30. Elagra MI, Rayyan MR, Alhomaidhi MM, Alanaziy AA, Alnefaie MO. Color stability and marginal integrity of interim crowns: an
in vitro study. Eur J Dent. 2017; 11:330–334. PMID:
28932142.

31. Zenthöfer A, Rammelsberg P, Schmitt C, Ohlmann B. Wear of metal-free resin composite crowns after three years in service. Dent Mater J. 2013; 32:787–792. PMID:
24088835.

32. Lambrechts P, Braem M, Vuylsteke-Wauters M, Vanherle G. Quantitative
in vivo wear of human enamel. J Dent Res. 1989; 68:1752–1754. PMID:
2600255.
33. Ohlmann B, Trame JP, Dreyhaupt J, Gabbert O, Koob A, Rammelsberg P. Wear of posterior metal-free polymer crowns after 2 years. J Oral Rehabil. 2008; 35:782–788. PMID:
18482349.
34. Asghar S, Ali A, Rashid S, Hussain T. Replacement of resin-based composite restorations in permanent teeth. J Coll Physicians Surg Pak. 2010; 20:639–643. PMID:
20943103.
35. Manhart J, Chen H, Hamm G, Hickel R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004; 29:481–508. PMID:
15470871.
36. Wilder AD Jr, May KN Jr, Bayne SC, Taylor DF, Leinfelder KF. Seventeen-year clinical study of ultraviolet-cured posterior composite class I and II restorations. J Esthet Dent. 1999; 11:135–142. PMID:
10825870.

37. Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford TR. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J Prosthet Dent. 2002; 88:297–301. PMID:
12426500.

38. Rinke S, Schäfer S, Lange K, Gersdorff N, Roediger M. Practice-based clinical evaluation of metal-ceramic and zirconia molar crowns: 3-year results. J Oral Rehabil. 2013; 40:228–237. PMID:
23211063.

39. Cehreli MC, Kokat AM, Ozpay C, Karasoy D, Akca K. A randomized controlled clinical trial of feldspathic versus glass-infiltrated alumina all-ceramic crowns: a 3-year follow-up. Int J Prosthodont. 2011; 24:77–84. PMID:
21210009.
40. Jung RE, Holderegger C, Sailer I, Khraisat A, Suter A, Hämmerle CH. The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: a randomized controlled clinical trial. Int J Periodontics Restorative Dent. 2008; 28:357–365. PMID:
18717374.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download