1. Frassetto A, Breschi L, Turco G, Marchesi G, Di Lenarda R, Tay FR, Pashley DH, Cadenaro M. Mechanisms of degradation of the hybrid layer in adhesive dentistry and therapeutic agents to improve bond durability--A literature review. Dent Mater. 2016; 32:e41–e53. PMID:
26743967.

2. Spencer P, Wang Y. Adhesive phase separation at the dentin interface under wet bonding conditions. J Biomed Mater Res. 2002; 62:447–456. PMID:
12209931.

3. Tay FR, Pashley DH, Yoshiyama M. Two modes of nanoleakage expression in single-step adhesives. J Dent Res. 2002; 81:472–476. PMID:
12161459.

4. Tjäderhane L, Nascimento FD, Breschi L, Mazzoni A, Tersariol IL, Geraldeli S, Tezvergil-Mutluay A, Carrilho MR, Carvalho RM, Tay FR, Pashley DH. Optimizing dentin bond durability: control of collagen degradation by matrix metalloproteinases and cysteine cathepsins. Dent Mater. 2013; 29:116–135. PMID:
22901826.

5. Bedran-Russo AK, Pauli GF, Chen SN, McAlpine J, Castellan CS, Phansalkar RS, Aguiar TR, Vidal CM, Napotilano JG, Nam JW, Leme AA. Dentin biomodification: strategies, renewable resources and clinical applications. Dent Mater. 2014; 30:62–76. PMID:
24309436.

6. Van Meerbeek B, Yoshihara K, Van Landuyt K, Yoshida Y, Peumans M. From Buonocore’s pioneering acid-etch technique to self-adhering restoratives. a status perspective of rapidly advancing dental adhesive technology. J Adhes Dent. 2020; 22:7–34. PMID:
32030373.
7. Singh P, Nagpal R, Singh UP, Manuja N. Effect of carbodiimide on the structural stability of resin/dentin interface. J Conserv Dent. 2016; 19:501–509. PMID:
27994309.

8. Al-Ammar A, Drummond JL, Bedran-Russo AK. The use of collagen cross-linking agents to enhance dentin bond strength. J Biomed Mater Res B Appl Biomater. 2009; 91:419–424. PMID:
19507140.
9. Fawzy AS, Nitisusanta LI, Iqbal K, Daood U, Neo J. Riboflavin as a dentin crosslinking agent: ultraviolet A versus blue light. Dent Mater. 2012; 28:1284–1291. PMID:
23031483.

10. Daood U, Swee Heng C, Neo Chiew Lian J, Fawzy AS.
In vitro analysis of riboflavin-modified, experimental, two-step etch-and-rinse dentin adhesive: Fourier transform infrared spectroscopy and micro-Raman studies. Int J Oral Sci. 2015; 7:110–124. PMID:
25257880.

11. De-Paula DM, Lomonaco D, Ponte AM, Cordeiro KE, Moreira MM, Mazzetto SE, Feitosa VP. Influence of collagen cross-linkers addition in phosphoric acid on dentin biomodification and bonding of an etch-and-rinse adhesive. Dent Mater. 2020; 36:e1–e8. PMID:
31791738.

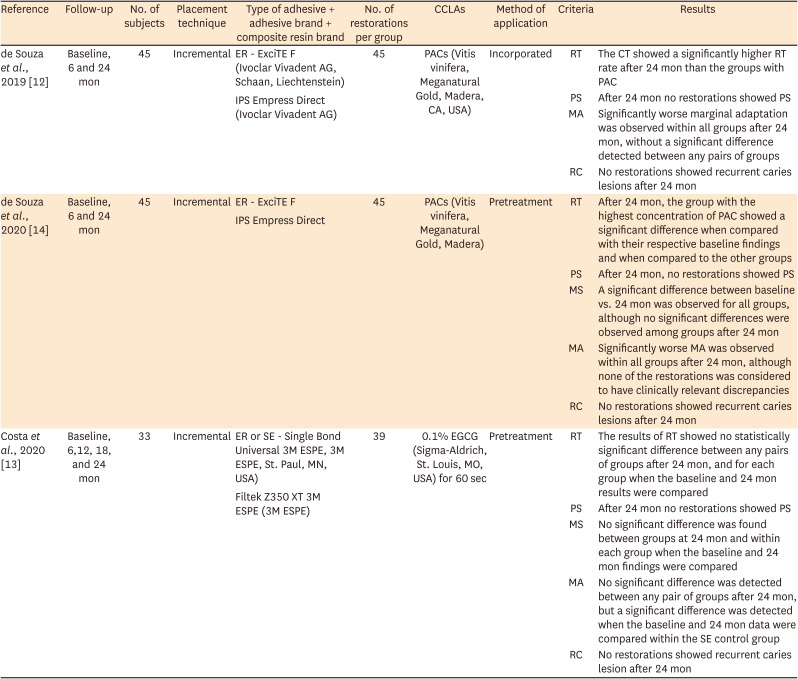
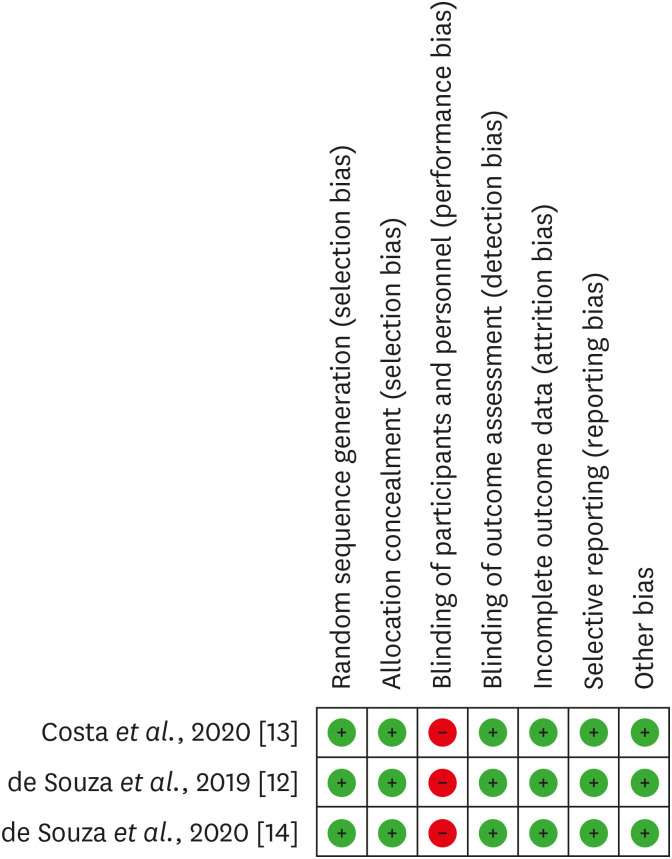
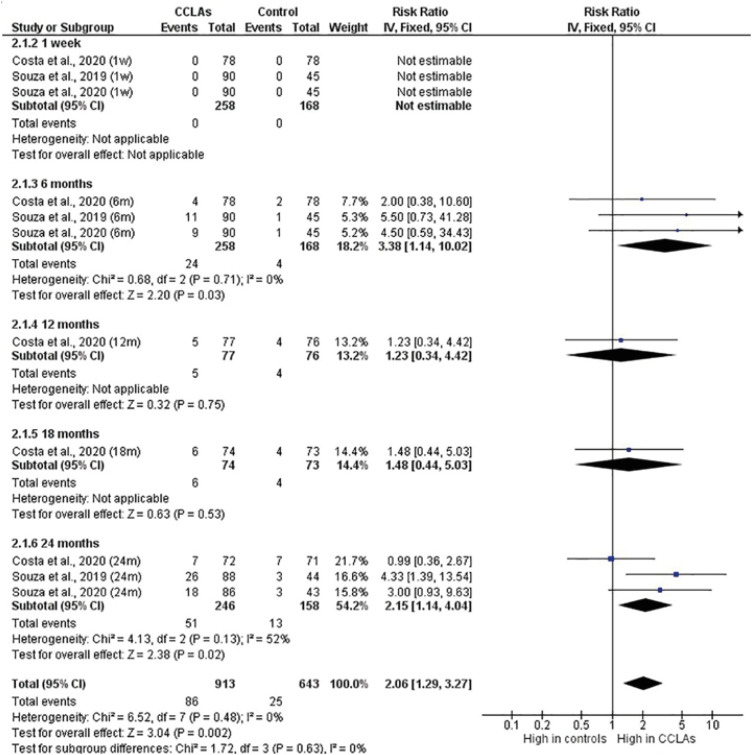
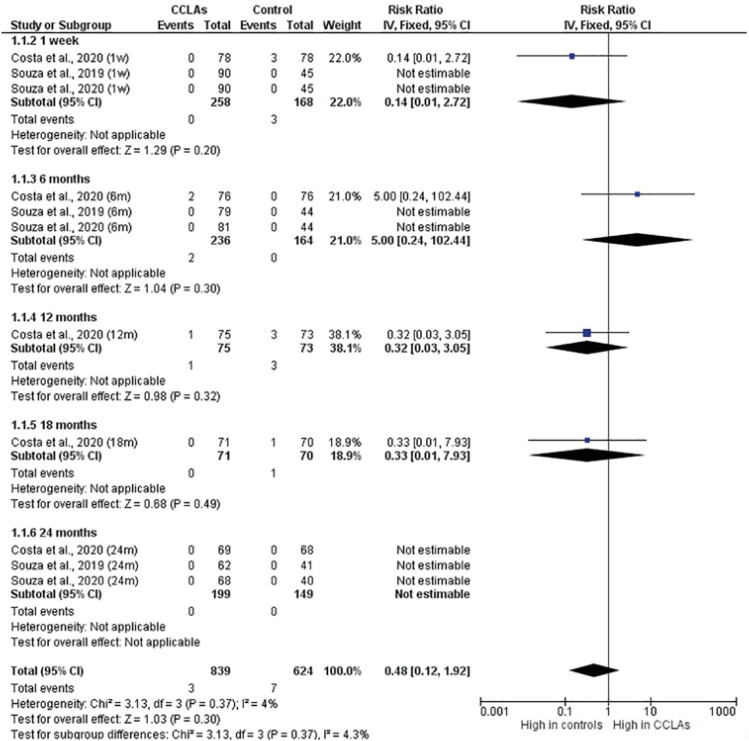
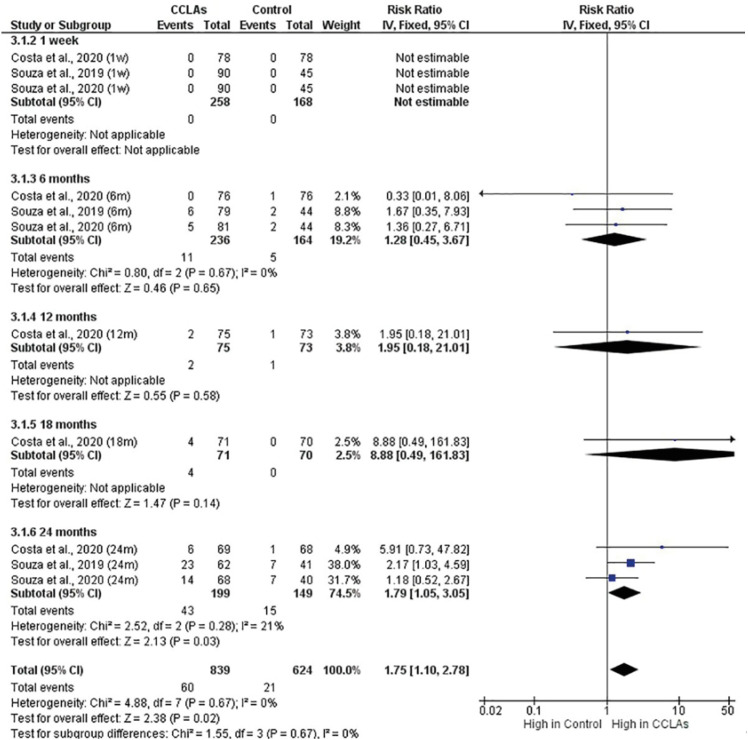
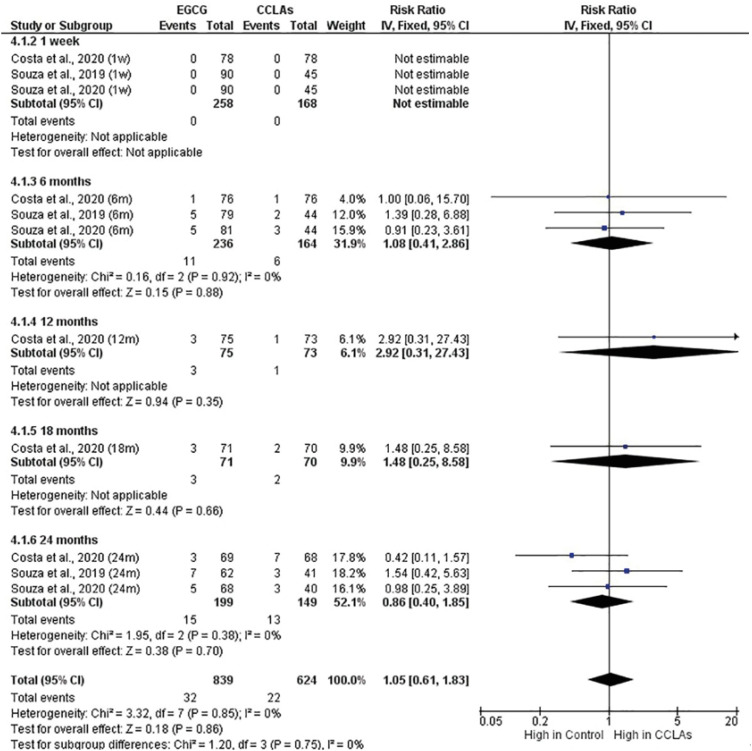
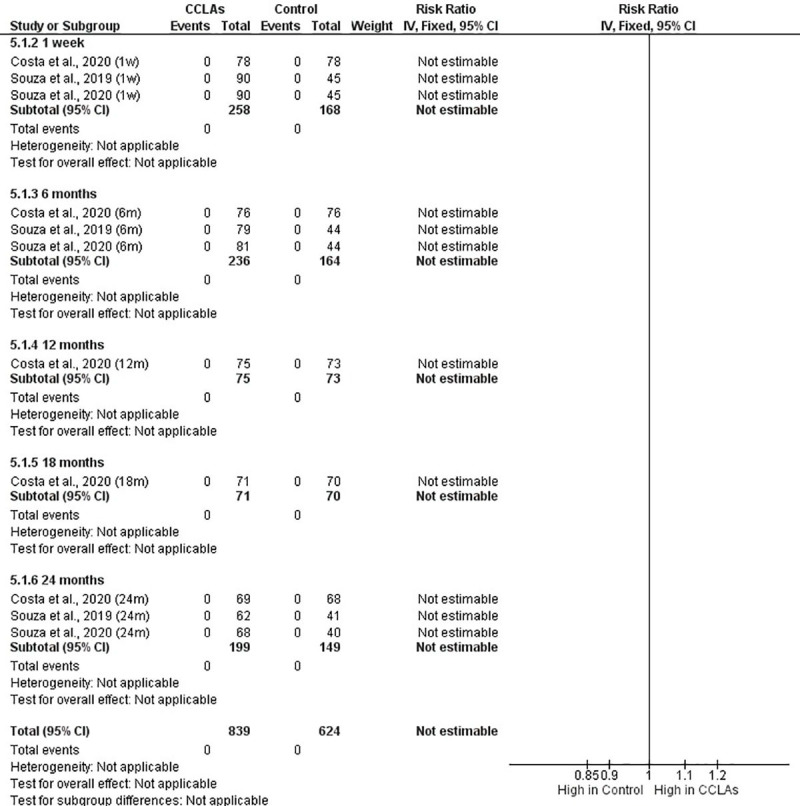
12. de Souza LC, Rodrigues NS, Cunha DA, Feitosa VP, Santiago SL, Reis A, Loguercio AD, Matos TP, Saboia VP, Perdigão J. Two-year clinical evaluation of proanthocyanidins added to a two-step etch-and-rinse adhesive. J Dent. 2019; 81:7–16. PMID:
30594631.

13. Costa C, Albuquerque N, Mendonça JS, Loguercio AD, Saboia V, Santiago SL. Catechin-based dentin pretreatment on the clinical performance of a universal adhesive: a two-year randomized clinical trial. Oper Dent. 2020; 45:473–483. PMID:
32352353.

14. de Souza LC, Rodrigues NS, Cunha DA, Feitosa VP, Santiago SL, Reis A, Loguercio AD, Perdigão J, Saboia VP. Two-year clinical evaluation of a proanthocyanidins-based primer in non-carious cervical lesions: a double-blind randomized clinical trial. J Dent. 2020; 96:103325. PMID:
32205201.

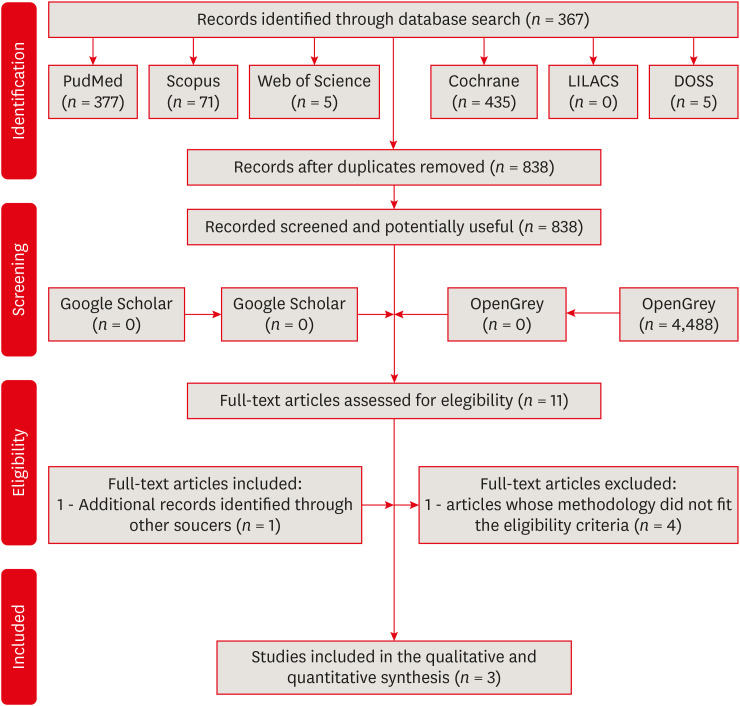
15. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097. PMID:
19621072.

16. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016; 5:210. PMID:
27919275.

17. Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of effectiveness. Aromataris E, Munn Z, editors. Joanna Briggs Institute reviewer’s manual. Adelaide: The Joanna Briggs Institute;2017.
18. Haas LF, Dutra K, Porporatti AL, Mezzomo LA, De Luca Canto G, Flores-Mir C, Corrêa M. Anatomical variations of mandibular canal detected by panoramic radiography and CT: a systematic review and meta-analysis. Dentomaxillofac Radiol. 2016; 45:20150310. PMID:
26576624.

19. Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations. place unknown: The GRADE Working Group;2013.
20. Dalton Bittencourt D, Ezecelevski IG, Reis A, Van Dijken JW, Loguercio AD. An 18-months’ evaluation of self-etch and etch & rinse adhesive in non-carious cervical lesions. Acta Odontol Scand. 2005; 63:173–178. PMID:
16191912.

21. Perdigão J, Dutra-Corrêa M, Saraceni CH, Ciaramicoli MT, Kiyan VH, Queiroz CS. Randomized clinical trial of four adhesion strategies: 18-month results. Oper Dent. 2012; 37:3–11. PMID:
21942235.

22. Aguiar TR, Vidal CM, Phansalkar RS, Todorova I, Napolitano JG, McAlpine JB, Chen SN, Pauli GF, Bedran-Russo AK. Dentin biomodification potential depends on polyphenol source. J Dent Res. 2014; 93:417–422. PMID:
24574140.

23. Bedran-Russo AK, Pashley DH, Agee K, Drummond JL, Miescke KJ. Changes in stiffness of demineralized dentin following application of collagen crosslinkers. J Biomed Mater Res B Appl Biomater. 2008; 86:330–334. PMID:
18161815.
24. Cova A, Breschi L, Nato F, Ruggeri A Jr, Carrilho M, Tjäderhane L, Prati C, Di Lenarda R, Tay FR, Pashley DH, Mazzoni A. Effect of UVA-activated riboflavin on dentin bonding. J Dent Res. 2011; 90:1439–1445. PMID:
21940521.

25. Cai J, Palamara JE, Burrow MF. Effects of collagen crosslinkers on dentine: a literature review. Calcif Tissue Int. 2018; 102:265–279. PMID:
29058055.

26. Yun JH, Pang EK, Kim CS, Yoo YJ, Cho KS, Chai JK, Kim CK, Choi SH. Inhibitory effects of green tea polyphenol (-)-epigallocatechin gallate on the expression of matrix metalloproteinase-9 and on the formation of osteoclasts. J Periodontal Res. 2004; 39:300–307. PMID:
15324350.

27. Jackson JK, Zhao J, Wong W, Burt HM. The inhibition of collagenase induced degradation of collagen by the galloyl-containing polyphenols tannic acid, epigallocatechin gallate and epicatechin gallate. J Mater Sci Mater Med. 2010; 21:1435–1443. PMID:
20162329.

28. Du X, Huang X, Huang C, Wang Y, Zhang Y. Epigallocatechin-3-gallate (EGCG) enhances the therapeutic activity of a dental adhesive. J Dent. 2012; 40:485–492. PMID:
22421091.

29. Yoshida Y, Yoshihara K, Nagaoka N, Hayakawa S, Torii Y, Ogawa T, Osaka A, Meerbeek BV. Self-assembled nano-layering at the adhesive interface. J Dent Res. 2012; 91:376–381. PMID:
22302145.

30. Mitra SB, Lee CY, Bui HT, Tantbirojn D, Rusin RP. Long-term adhesion and mechanism of bonding of a paste-liquid resin-modified glass-ionomer. Dent Mater. 2009; 25:459–466. PMID:
19041127.

31. Perdigão J, Kose C, Mena-Serrano AP, De Paula EA, Tay LY, Reis A, Loguercio AD. A new universal simplified adhesive: 18-month clinical evaluation. Oper Dent. 2014; 39:113–127. PMID:
23802645.

32. Lawson NC, Robles A, Fu CC, Lin CP, Sawlani K, Burgess JO. Two-year clinical trial of a universal adhesive in total-etch and self-etch mode in non-carious cervical lesions. J Dent. 2015; 43:1229–1234. PMID:
26231300.

33. Moreira MA, Souza NO, Sousa RS, Freitas DQ, Lemos MV, De Paula DM, Maia FJ, Lomonaco D, Mazzetto SE, Feitosa VP. Efficacy of new natural biomodification agents from
Anacardiaceae extracts on dentin collagen cross-linking. Dent Mater. 2017; 33:1103–1109. PMID:
28751073.

34. Scheffel DL, Hebling J, Scheffel RH, Agee K, Turco G, de Souza Costa CA, Pashley D. Inactivation of matrix-bound matrix metalloproteinases by cross-linking agents in acid-etched dentin. Oper Dent. 2014; 39:152–158. PMID:
23786610.

35. Machado AC, Dezan Junior E, Gomes-Filho JE, Cintra LT, Ruviére DB, Zoccal R, Damante CA, Jardim Junior EG. Evaluation of tissue reaction to Aroeira (
Myracrodruon urundeuva) extracts: a histologic and edemogenic study. J Appl Oral Sci. 2012; 20:414–418. PMID:
23032202.

36. Santiago SL, Osorio R, Neri JR, Carvalho RM, Toledano M. Effect of the flavonoid epigallocatechin-3-gallate on resin-dentin bond strength. J Adhes Dent. 2013; 15:535–540. PMID:
23560257.
37. Neri JR, Yamauti M, Da Silveira F, Mendonça JS, Carvalho RM, Santiago SL. Influence of dentin biomodification with epigallocatechin-3-gallate on the bond strength of self-etch adhesive: twelve-month results. Int J Adhes Adhes. 2016; 71:81–86.

38. Zheng P, Chen H. Evaluate the effect of different MMPs inhibitors on adhesive physical properties of dental adhesives, bond strength and MMP substarte activity. Sci Rep. 2017; 7:4975–4980. PMID:
28694471.

39. Liu Y, Wang Y. Effect of proanthocyanidins and photo-initiators on photo-polymerization of a dental adhesive. J Dent. 2013; 41:71–79. PMID:
23079281.

40. Epasinghe DJ, Yiu CK, Burrow MF, Tay FR, King NM. Effect of proanthocyanidin incorporation into dental adhesive resin on resin-dentine bond strength. J Dent. 2012; 40:173–180. PMID:
22155037.

41. Epasinghe DJ, Yiu CK, Burrow MF. Mechanical properties, water sorption characteristics, and compound release of grape seed extract-incorporated resins. J Appl Oral Sci. 2017; 25:412–419. PMID:
28877280.

42. Pallan S, Furtado Araujo MV, Cilli R, Prakki A. Mechanical properties and characteristics of developmental copolymers incorporating catechin or chlorhexidine. Dent Mater. 2012; 28:687–694. PMID:
22460187.

43. Innes NP, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, Van Landuyt K, Banerjee A, Campus G, Doméjean S, Fontana M, Leal S, Lo E, Machiulskiene V, Schulte A, Splieth C, Zandona A, Schwendicke F. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res. 2016; 28:49–57. PMID:
27099357.

44. Perdigão J, Reis A, Loguercio AD. Dentin adhesion and MMPs: a comprehensive review. J Esthet Restor Dent. 2013; 25:219–241. PMID:
23910180.
45. Hörsted-Bindslev P, Knudsen J, Baelum V. 3-year clinical evaluation of modified Gluma adhesive systems in cervical abrasion/erosion lesions. Am J Dent. 1996; 9:22–26. PMID:
9002810.
46. Gallo JR, Burgess JO, Ripps AH, Walker RS, Winkler MM, Mercante DE, Davidson JM. Two-year clinical evaluation of a posterior resin composite using a fourth- and fifth-generation bonding agent. Oper Dent. 2005; 30:290–296. PMID:
15986947.
47. Oz FD, Ergin E, Canatan S. Twenty-four-month clinical performance of different universal adhesives in etch-and-rinse, selective etching and self-etch application modes in NCCL - a randomized controlled clinical trial. J Appl Oral Sci. 2019; 27:e20180358. PMID:
30994773.

48. Chermont AB, Carneiro KK, Lobato MF, Machado SM, Silva e Souza Junior MH. Clinical evaluation of postoperative sensitivity using self-etching adhesives containing glutaraldehyde. Braz Oral Res. 2010; 24:349–354. PMID:
20877974.

49. Çakır NN, Demirbuga S. The effect of five different universal adhesives on the clinical success of class I restorations: 24-month clinical follow-up. Clin Oral Investig. 2019; 23:2767–2776.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download