INTRODUCTION
Apical constriction (AC) is defined as the apical part of a root canal that has the narrowest diameter, and it is usually located 0.5 to 1 mm coronal to the apical foramen (AF) [
1]. Earlier studies evaluating AC morphology were performed using destructive methods such as sectioning and grinding of teeth [
234], while more recent studies [
567] have used non-invasive micro-computed tomography (micro-CT) imaging as a more sensitive and accurate technique.
Furthermore, it has been reported that AC may not be present in all root canals [
8], and a relatively recent study with micro-CT imaging has reported that AC was present in only 35% of the root canals evaluated [
5]. Conversely, other micro-CT studies have noted the presence of AC in all samples evaluated [
67]. Moreover, narrowing of root canals [
4] and AC with increasing age has been reported [
6]. Clinically, it is important to evaluate the presence and size of AC in different age groups, which would help clinicians to choose the initial apical binding file for adequate root canal preparation.
The maxillary first molar is known to be one of the most complex teeth in the dental arch in terms of its root canal morphology [
9]. Apical root canal complexities such as apical ramifications, apical constriction morphotypes, the AC to AF distance, and the position of the AF and accessory canals can jeopardize successful endodontic outcomes [
5610]. Previous micro-CT studies [
5911] have evaluated maxillary molar root canal anatomy without providing the demographic data (age and sex) of the cohort, except ElAyouti
et al. [
6], who evaluated the root canal anatomy of teeth from individuals with a known age, but did not compare the first and second maxillary molars. To the best of our knowledge, no published studies in the English-language literature have evaluated the apical root canal anatomy of maxillary first and second molars from patients with known age and sex, using micro-CT imaging.
Therefore, this ex vivo study was undertaken to evaluate and compare the presence or absence, morphotype, dimensions, and profile (shape) of AC along with the apical root canal dimensions, AF position, AC-AF distance, and the presence of accessory canals in the maxillary first and second molars of patients with known age and sex using micro-CT. The null hypothesis tested was that there would be no difference in the anatomic parameters between maxillary first and second molars.
DISCUSSION
In the present study, there were no significant differences in any of the parameters evaluated between maxillary first and second molars and the null hypothesis was accepted.
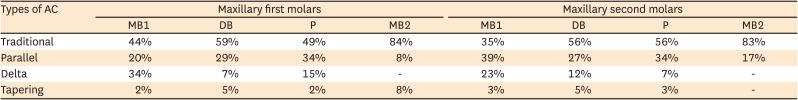
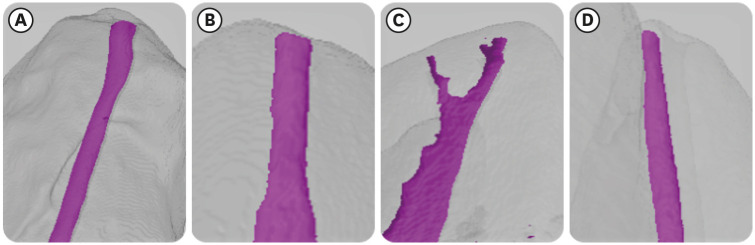
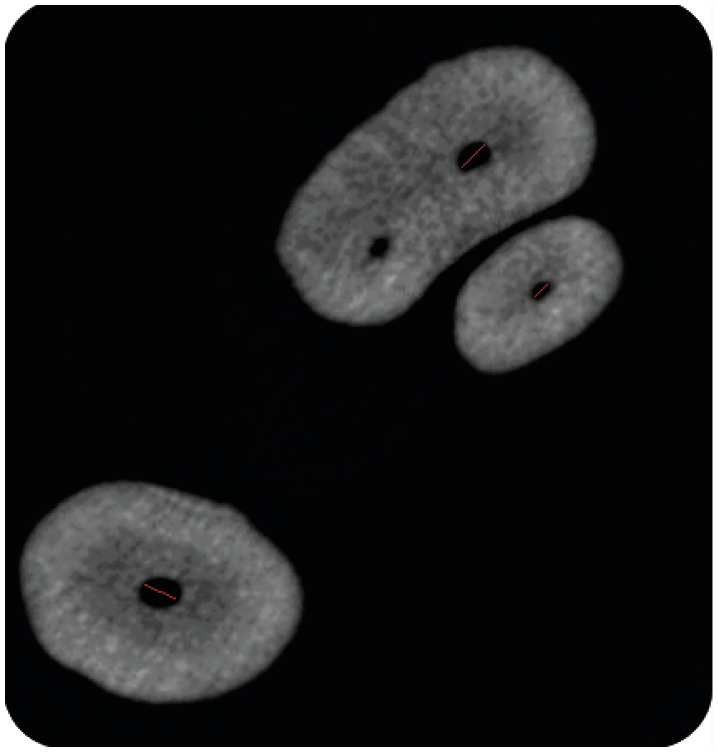
The initial research on AC and AF morphology was done by Kuttler [
2], who reported that AC can be present in the apical root dentin. The most prevalent morphotype of AC in the present study was the traditional constriction, followed by the parallel, delta, and tapering morphotypes. The multi-constriction type of AC, previously identified by Dummer
et al. [
3] and flared type [
5] of apical morphology were not identified in our study population. Apical morphotypes similar to ours have been reported by previous researchers in North America, with AC being identified in 35% [
5] and 23% [
11] of root canals evaluated. However, ElAyouti
et al. [
6] and Schell
et al. [
7], who included the parallel morphotype as a type of AC, reported the presence of AC in all root canals investigated. Based on micro-CT imaging, it was evident that achieving patency of the root canal may be difficult in delta-type constrictions.
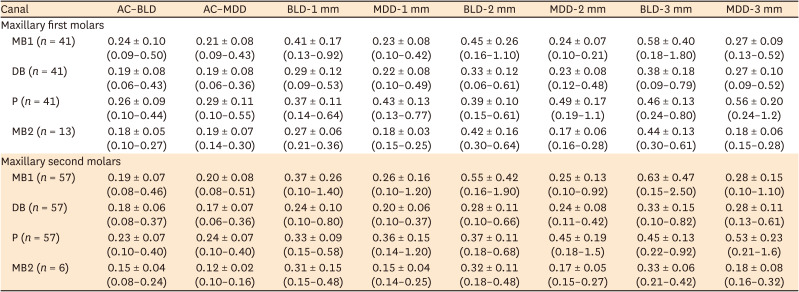
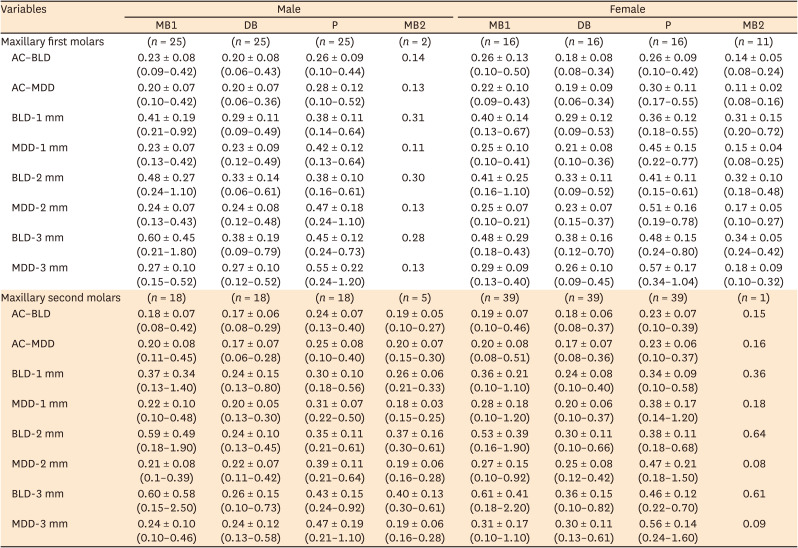
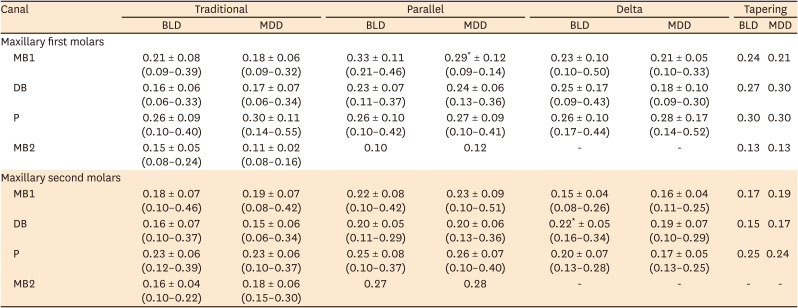
The mean AC dimensions in our study fall within the range reported in previous investigations [
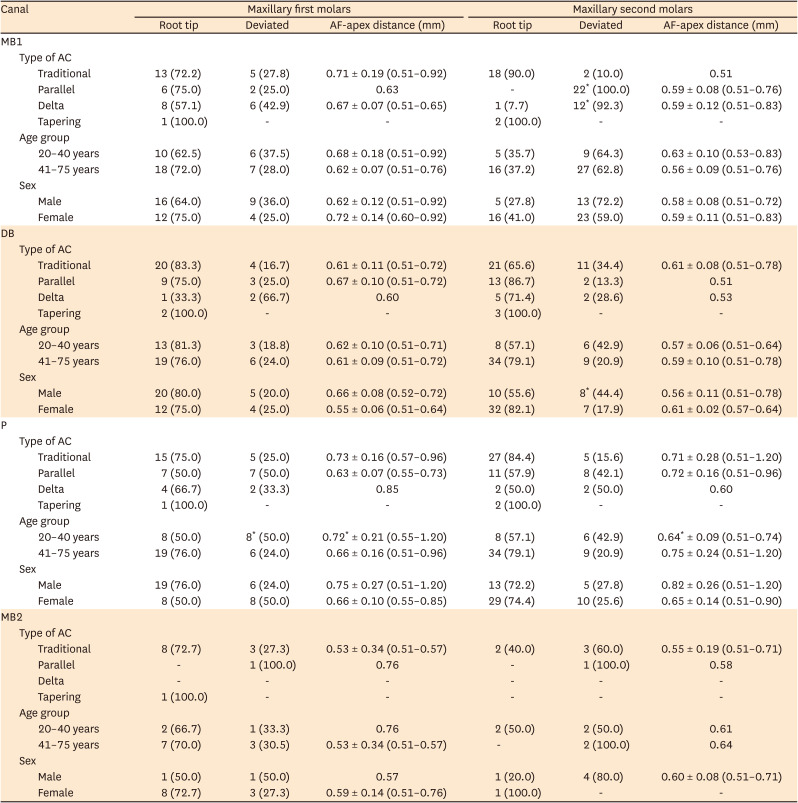
691115]. In clinical terms, the mean AC dimensions in MB1 canals of the maxillary first and second molars approximately corresponded to teeth #25 and #20 instrument tip sizes, respectively. The mean AC dimensions in DB canals of both the maxillary first and second molars approximately corresponded to a tooth #20 instrument tip size. The mean AC dimensions in palatal canals of the maxillary first and second molars approximately corresponded to teeth #30 and #25 instrument tip sizes, respectively, while the mean AC dimension of MB2 canals in the first and second maxillary molars corresponded approximately to teeth #20 and #15 instrument tip sizes, respectively. This information would be of clinical value for managing endodontic interventions of the first and second maxillary molars.
The tooth #40.04 instrument has been recommended for conservative preparations of maxillary molar palatal canals [
11]. ElAyouti
et al. [
6] recommended shaping maxillary and mandibular molars to sizes larger than tooth #25, while Versiani
et al. [
16] reported that apical debridement in 4-rooted maxillary molars should be done with instruments larger than ISO size 40. The wide range of constriction dimensions reported in this study indicates that it is important to assess the BLD and MDD of AC diameters and that apical shaping to smaller sizes [
6] would not be beneficial.
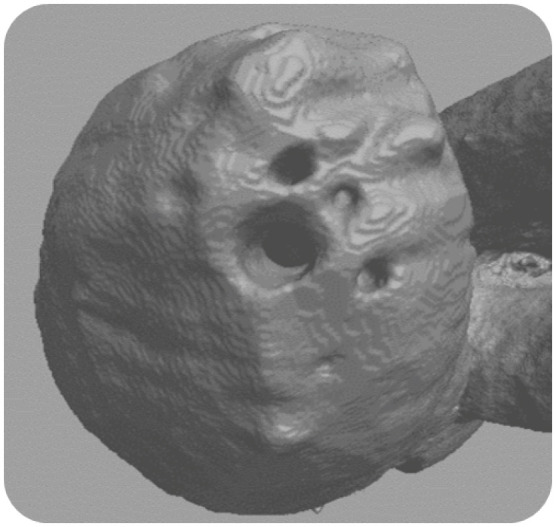
Additionally, previous researchers have classified AC dimensions as either major diameter/minor diameter or wide/narrow diameter morphotypes [
915]. The present study analyzed AC and apical root canal measurements in both the BLD and MDD, which may be of additional clinical utility. Our results demonstrated that MB1, MB2, and DB apical canals along with ACs were broader bucco-lingually, while palatal apical canals and Acs were broader mesio-distally in both maxillary molars. A similar mesio-distal ovoid form of palatal apical canals has been previously reported [
11].
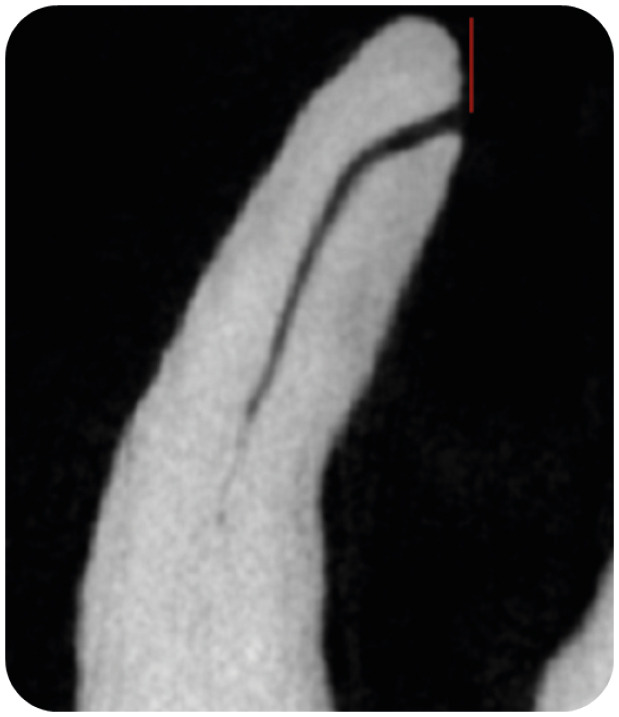
In the present study, the MDD of apical canals had 0.02 and 0.04 mm tapers in MB1 canal of the first and second molars, respectively, and a 0.04 mm taper in DB canals of both maxillary molars. The apical canal BLD presented a 0.07 mm taper in palatal canals of both maxillary molars. This finding indicates that conservative preparation of the MDD in MB1, MB2, and DB canals can be performed using 0.04–0.06 mm taper rotary instruments, and the BLD in palatal canals can be prepared using 0.06–0.08 mm taper rotary instruments with the tip size based on the initial apical binding file. Directing the files bucco-lingually in MB1, MB2, and DB canals and mesio-distally in palatal canals will ensure maximal contact between rotary instruments and root canal walls [
11]. Alternatively, the use of self-adjusting files or irrigation activation techniques using XP-endo finisher or passive ultrasonic irrigation can lead to enhanced debridement of oval canals [
1718].
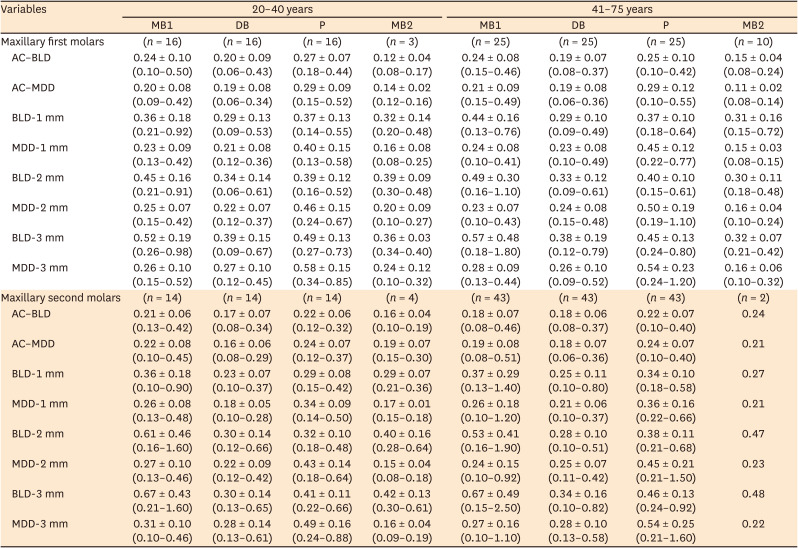
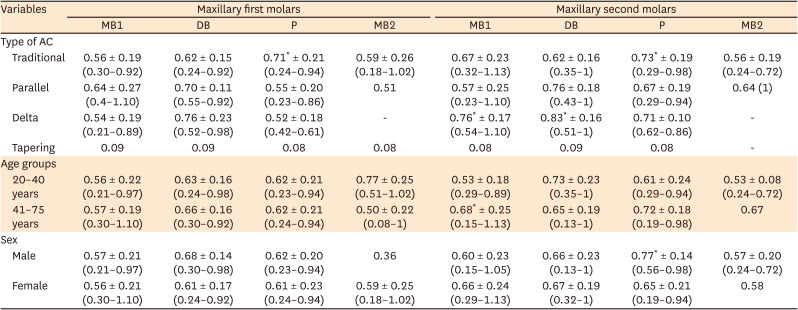
Among the previous micro-CT studies [
567911], only ElAyouti
et al. [
6] included samples with known age (15–60 years), while other studies [
57911] did not evaluate samples from individuals of known age. In the present study, AC dimensions were not significantly correlated with age (20–40 years vs. 41–75 years) or sex. There is some controversy in this regard, as ElAyouti
et al. [
6] reported that ACs became narrower with increasing age, while another study reported no significant dimensional changes with age [
19]. Yet another study reported significant canal narrowing (2 mm) from the apex with increasing age, especially in palatal and MB canals, but not in DB canals of maxillary molars [
4]. These varying results may reflect the difference in methodologies employed by various researchers, necessitating further micro-CT imaging research on the root canal anatomy of maxillary molars.
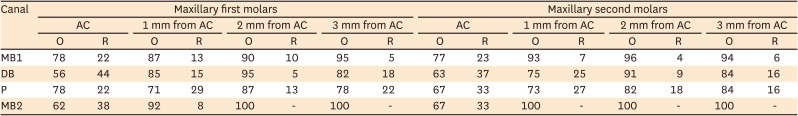
Our results also revealed that almost 70% of ACs were oval, and that more than 80% of apical root canals had an oval cross-section. A similar preponderance of oval forms in maxillary molars has been previously reported [
15]. Therefore, accurate AC size evaluation with a round instrument can be difficult clinically [
15].
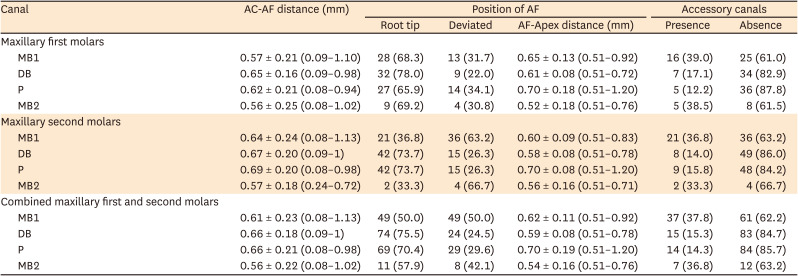
In the present study, the majority (60%) of AF were located within 0.5 mm from the anatomic apex in both maxillary molars. The distance between the AF and anatomic apex was less than 1 mm in MB and DB roots, while it was up to 1.2 mm in palatal roots of the first and second maxillary molars. These results are in contrast with Marceliano-Alves
et al. [
9], who reported that the AF did not coincide with the anatomic apex 95% of the time in palatal roots of maxillary molars, and ElAyouti
et al. [
6], who reported that the AF can be more than 2 mm short of the anatomic apex in molars.
Additionally, our data showed that the mean AC-AF distance was 0.60 and 0.64 mm in the maxillary first and second molars, respectively. This finding is not consistent with those of ElAyouti
et al. [
6], who reported a mean AC-to-AF distance of only 0.2 mm, and that AC coincided with the AF in 14% of canals. This discrepancy may be due to the varying reference points used to evaluate the AC-AF distance. However, Kuttler [
2] reported mean AC-AF distances of 0.5–0.6 mm, which is within the range reported in the present study. Furthermore, in the present study, the mean AC-AF distance was significantly greater in MB1 canals of the maxillary second molars in patients aged above 40 years. Overall, tapering-type constrictions had a mean AC-AF distance of 0.09 mm, as previously reported [
6], while traditional constriction, parallel and delta-type constrictions had mean AC-AF distances ranging from 0.21 to 1.13 mm. Furthermore, among constriction types in both MB1 and DB canals of the maxillary second molars, the delta type had a significantly greater mean AC-AF distance (0.76 and 0.83 mm, respectively). In palatal canals of both the first and second maxillary molars, the traditional constriction type had a significantly greater mean AC-AF distance (0.71 and 0.73 mm, respectively) than the other constriction types. Therefore, the type of constriction may be associated with the AC-AF distance.
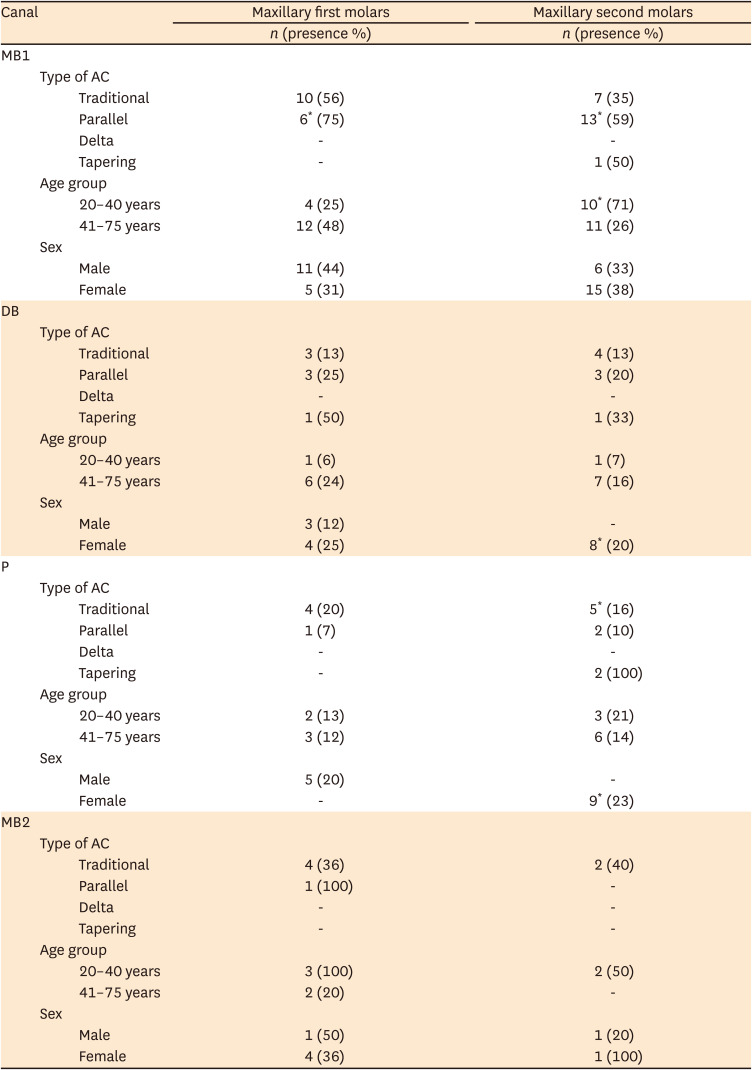
The presence of accessory canals in the apical 5 mm was evaluated, and it was found that accessory canals in the first and second maxillary molars were most frequently found in MB1 canals (39% and 37%, respectively) canals followed by MB2 canals (38% and 33%, respectively), DB canals (17% and 14%, respectively), and palatal canals (12% and 16%, respectively). Similarly, a previous micro-CT study by Briseno-Marroquin
et al. [
20], who evaluated maxillary molars from an Egyptian population, reported accessory canals in 31% of MB1 canals, 15% of DB canals, and 12% of palatal canals. Another micro-CT study that evaluated the MB roots of maxillary first molars reported that the majority of the accessory canals were found in the apical third of root canals [
15]. Fused maxillary second molars showed an increased frequency of apical delta and anatomical complexities [
21]. Clinically, these accessory canals and apical ramifications may be difficult to instrument and must be chemically debrided and disinfected [
22].
An extensive literature review by Cleghorn
et al. [
23] reported that maxillary first molars can have 2 canals (MB1 and MB2) in 57% of MB roots, of which 38% may have 2 exit portals. In the present study, 91% of MB roots had an MB2 canal. However, only 21% of the MB2 canals identified had a separate exit. Furthermore, none of the samples evaluated in our study had second disto-buccal (DB2) or other extra canals.
A major limitation of the current study is the relatively small sample size and the resolution (26.7 µm) of the micro-CT system used. Therefore, future research with a larger sample size and higher-resolution micro-CT imaging will have to be done to better evaluate the effect of age and sex on AC and apical root canal anatomy. In addition, samples from different racial populations need to be assessed.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download