1. Nair PNR, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99:231–252. PMID:
15660098.

2. Ricucci D, Siqueira JF Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod. 2010; 36:1277–1288. PMID:
20647081.

3. Machado MEDL, Sapia LAB, Cai S, Martins GHR, Nabeshima CK. Comparison of two rotary systems in root canal preparation regarding disinfection. J Endod. 2010; 36:1238–1240. PMID:
20630307.

4. Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014; 216:299–303. PMID:
24651335.

5. Gazzaneo I, Vieira GCS, Pérez AR, Alves FRF, Gonçalves LS, Mdala I, Siqueira JF Jr, Rôças IN. Root canal disinfection by single- and multiple-instrument systems: effects of sodium hypochlorite volume, concentration, and retention time. J Endod. 2019; 45:736–741. PMID:
30981431.

6. Ordinola-Zapata R, Bramante CM, Aprecio RM, Handysides R, Jaramillo DE. Biofilm removal by 6% sodium hypochlorite activated by different irrigation techniques. Int Endod J. 2014; 47:659–666. PMID:
24117881.

7. Wright PP, Scott S, Kahler B, Walsh LJ. Organic tissue dissolution in clodronate and etidronate mixtures with sodium hypochlorite. J Endod. 2020; 46:289–294. PMID:
31839410.

8. Coaguila-Llerena H, Stefanini da Silva V, Tanomaru-Filho M, Guerreiro Tanomaru JM, Faria G. Cleaning capacity of octenidine as root canal irrigant: a scanning electron microscopy study. Microsc Res Tech. 2018; 81:523–527. PMID:
29436057.

9. Chow TW. Mechanical effectiveness of root canal irrigation. J Endod. 1983; 9:475–479. PMID:
6586975.

10. Boutsioukis C, Lambrianidis T, Kastrinakis E, Bekiaroglou P. Measurement of pressure and flow rates during irrigation of a root canal
ex vivo with three endodontic needles. Int Endod J. 2007; 40:504–513. PMID:
17326784.

11. Neelakantan P, Devaraj S, Jagannathan N. Histologic assessment of debridement of the root canal isthmus of mandibular molars by irrigant activation techniques
ex vivo
. J Endod. 2016; 42:1268–1272. PMID:
27339632.

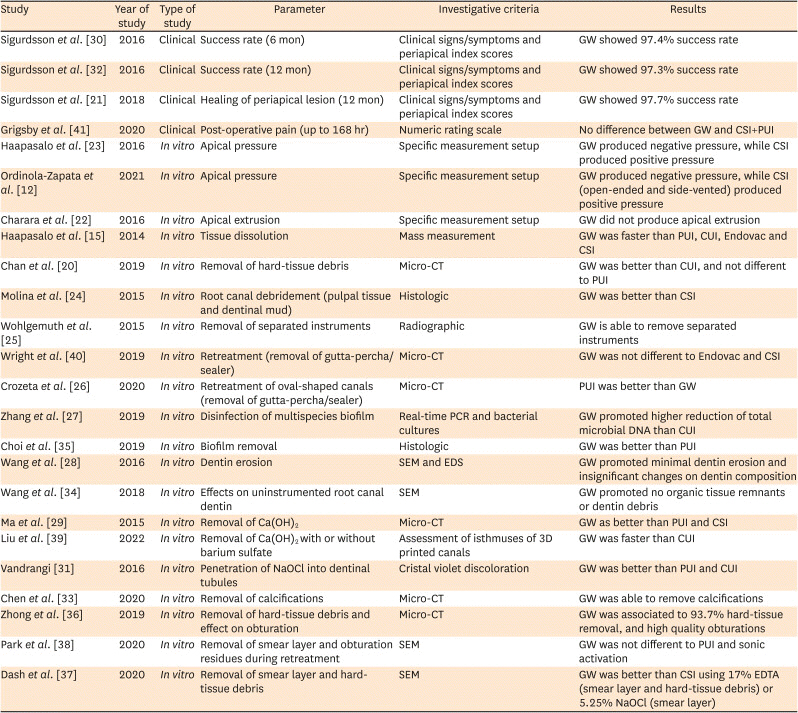
12. Ordinola-Zapata R, Crepps JT, Arias A, Lin F.
In vitro apical pressure created by 2 irrigation needles and a multisonic system in mandibular molars. Restor Dent Endod. 2021; 46:e14. PMID:
33680903.
13. Faria G, Viola KS, Coaguila-Llerena H, Oliveira LRA, Leonardo RT, Aranda-García AJ, Guerreiro-Tanomaru JM. Penetration of sodium hypochlorite into root canal dentine: effect of surfactants, gel form and passive ultrasonic irrigation. Int Endod J. 2019; 52:385–392. PMID:
30220093.
14. Faria G, Viola KS, Kuga MC, Garcia AJA, Daher VB, De Pasquali Leonardo MF, Tanomaru-Filho M. Effect of rotary instrument associated with different irrigation techniques on removing calcium hydroxide dressing. Microsc Res Tech. 2014; 77:642–646. PMID:
24844676.

15. Haapasalo M, Wang Z, Shen Y, Curtis A, Patel P, Khakpour M. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014; 40:1178–1181. PMID:
25069928.

16. GentleWave Datasheet [Internet]. Laguna Hills, CA: Sonendo, Inc.;2021. updated 2021. cited 2021 Mar 4. Available from:
https://www.sonendo.com.
17. Shon WJ. Introducing the GentleWave system. Restor Dent Endod. 2016; 41:235. PMID:
27508167.

18. Sabeti M, Kazem M, Dianat O, Bahrololumi N, Beglou A, Rahimipour K, Dehnavi F. Impact of access cavity design and root canal taper on fracture resistance of endodontically treated teeth: an
ex vivo investigation. J Endod. 2018; 44:1402–1406. PMID:
30049471.

19. Augusto CM, Barbosa AFA, Guimarães CC, Lima CO, Ferreira CM, Sassone LM, Silva EJNL. A laboratory study of the impact of ultraconservative access cavities and minimal root canal tapers on the ability to shape canals in extracted mandibular molars and their fracture resistance. Int Endod J. 2020; 53:1516–1529. PMID:
32683704.

20. Chan R, Versiani MA, Friedman S, Malkhassian G, Sousa-Neto MD, Leoni GB, Silva-Sousa YT, Basrani B. Efficacy of 3 supplementary irrigation protocols in the removal of hard tissue debris from the mesial root canal system of mandibular molars. J Endod. 2019; 45:923–929. PMID:
31104820.

21. Sigurdsson A, Garland RW, Le KT, Rassoulian SA. Healing of periapical lesions after endodontic treatment with the GentleWave procedure: a prospective multicenter clinical study. J Endod. 2018; 44:510–517. PMID:
29336878.

22. Charara K, Friedman S, Sherman A, Kishen A, Malkhassian G, Khakpour M, Basrani B. Assessment of apical extrusion during root canal irrigation with the novel GentleWave system in a simulated apical environment. J Endod. 2016; 42:135–139. PMID:
26547720.
23. Haapasalo M, Shen Y, Wang Z, Park E, Curtis A, Patel P, Vandrangi P. Apical pressure created during irrigation with the GentleWave™ system compared to conventional syringe irrigation. Clin Oral Investig. 2016; 20:1525–1534.

24. Molina B, Glickman G, Vandrangi P, Khakpour M. Evaluation of root canal debridement of human molars using the GentleWave system. J Endod. 2015; 41:1701–1705. PMID:
26275599.

25. Wohlgemuth P, Cuocolo D, Vandrangi P, Sigurdsson A. Effectiveness of the GentleWave system in removing separated instruments. J Endod. 2015; 41:1895–1898. PMID:
26409807.

26. Crozeta BM, Chaves de Souza L, Correa Silva-Sousa YT, Sousa-Neto MD, Jaramillo DE, Silva RM. Evaluation of passive ultrasonic irrigation and GentleWave system as adjuvants in endodontic retreatment. J Endod. 2020; 46:1279–1285. PMID:
32553874.

27. Zhang D, Shen Y, de la Fuente-Núñez C, Haapasalo M.
In vitro evaluation by quantitative real-time PCR and culturing of the effectiveness of disinfection of multispecies biofilms in root canals by two irrigation systems. Clin Oral Investig. 2019; 23:913–920.

28. Wang Z, Maezono H, Shen Y, Haapasalo M. Evaluation of root canal dentin erosion after different irrigation methods using energy-dispersive X-ray spectroscopy. J Endod. 2016; 42:1834–1839. PMID:
27769680.

29. Ma J, Shen Y, Yang Y, Gao Y, Wan P, Gan Y, Patel P, Curtis A, Khakpour M, Haapasalo M.
In vitro study of calcium hydroxide removal from mandibular molar root canals. J Endod. 2015; 41:553–558. PMID:
25596727.
30. Sigurdsson A, Le KT, Woo SM, Rassoulian SA, McLachlan K, Abbassi F, Garland RW. Six-month healing success rates after endodontic treatment using the novel GentleWave™ System: the pure prospective multi-center clinical study. J Clin Exp Dent. 2016; 8:e290–e298. PMID:
27398180.

31. Vandrangi P. Evaluating penetration depth of treatment fluids into dentinal tubules using the GentleWave system. Dentistry (Loma Linda). 2016; 06:3–7.

32. Sigurdsson A, Garland RW, Le KT, Woo SM. 12-month healing rates after endodontic therapy using the novel GentleWave system: a prospective multicenter clinical study. J Endod. 2016; 42:1040–1048. PMID:
27325455.

33. Chen B, Szabo D, Shen Y, Zhang D, Li X, Ma J, Haapasalo M. Removal of calcifications from distal canals of mandibular molars by a non-instrumentational cleaning system: a micro-CT study. Aust Endod J. 2020; 46:11–16. PMID:
31605428.

34. Wang Z, Shen Y, Haapasalo M. Root canal wall dentin structure in uninstrumented but cleaned human premolars: a scanning electron microscopic study. J Endod. 2018; 44:842–848. PMID:
29550004.

35. Choi HW, Park SY, Kang MK, Shon WJ. Comparative analysis of biofilm removal efficacy by multisonic ultracleaning system and passive ultrasonic activation. Materials (Basel). 2019; 12:3492.

36. Zhong X, Shen Y, Ma J, Chen WX, Haapasalo M. Quality of root filling after obturation with gutta-percha and 3 different sealers of minimally instrumented root canals of the maxillary first molar. J Endod. 2019; 45:1030–1035. PMID:
31182216.

37. Dash S, Ismail PM, Singh J, Agwan MA, Ravikumar K, Annadurai T. Assessment of effectiveness of erbium:yttrium–aluminum–garnet laser, GentleWave irradiation, photodynamic therapy, and sodium hypochlorite in smear layer removal. J Contemp Dent Pract. 2020; 21:1266–1269. PMID:
33850073.

38. Park SY, Kang MK, Choi HW, Shon WJ. Comparative analysis of root canal filling debris and smear layer removal efficacy using various root canal activation systems during endodontic retreatment. Medicina (Kaunas). 2020; 56:615.

39. Liu H, Shen Y, Wang Z, Haapasalo M. The ability of different irrigation methods to remove mixtures of calcium hydroxide and barium sulphate from isthmuses in 3D printed transparent root canal models. Odontology. 2022; 110:27–34. PMID:
34143348.

40. Wright CR, Glickman GN, Jalali P, Umorin M. Effectiveness of gutta-percha/sealer removal during retreatment of extracted human molars using the GentleWave system. J Endod. 2019; 45:808–812. PMID:
30935619.

41. Grigsby D Jr, Ordinola-Zapata R, McClanahan SB, Fok A. Postoperative pain after treatment using the GentleWave system: a randomized controlled trial. J Endod. 2020; 46:1017–1022. PMID:
32553417.

42. Spencer HR, Ike V, Brennan PA. Review: the use of sodium hypochlorite in endodontics--potential complications and their management. Br Dent J. 2007; 202:555–559. PMID:
17496870.

43. Wong DTS, Cheung GSP. Extension of bactericidal effect of sodium hypochlorite into dentinal tubules. J Endod. 2014; 40:825–829. PMID:
24862710.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download