1. Bonnal J, Thibaut A, Brotchi J, Born J. Invading meningiomas of the sphenoid ridge. J Neurosurg. 1980; 53:587–599. PMID:
7431070.

2. Castellano F, Guidetti B, Olivecrona H. Pterional meningiomas en plaque. J Neurosurg. 1952; 9:188–196. PMID:
14908653.

3. Honeybul S, Neil-Dwyer G, Lang DA, Evans BT, Ellison DW. Sphenoid wing meningioma en plaque: a clinical review. Acta Neurochir (Wien). 2001; 143:749–757. discussion 758. PMID:
11678395.

4. Bikmaz K, Mrak R, Al-Mefty O. Management of bone-invasive, hyperostotic sphenoid wing meningiomas. J Neurosurg. 2007; 107:905–912. PMID:
17977259.

5. Elder TA, Yokoi H, Chugh AJ, Lagman C, Wu O, Wright CH, et al. En plaque meningiomas: a narrative review. J Neurol Surg B Skull Base. 2021; 82(Suppl 3):e33–e44. PMID:
34306915.

6. Muhsen BA, Aljariri AI, Hashem H, Alzoubi Q, Sarhan N, Al-Hussaini M, et al. En-plaque sphenoid wing grade II meningioma: case report and review of literature. Ann Med Surg (Lond). 2022; 74:103322. PMID:
35145681.

7. Fariselli L, Biroli A, Signorelli A, Broggi M, Marchetti M, Biroli F. The cavernous sinus meningiomas’ dilemma: surgery or stereotactic radiosurgery? Rep Pract Oncol Radiother. 2016; 21:379–385. PMID:
27330423.

8. Maroon JC, Kennerdell JS, Vidovich DV, Abla A, Sternau L. Recurrent spheno-orbital meningioma. J Neurosurg. 1994; 80:202–208. PMID:
8283257.

9. Li Y, Shi JT, An YZ, Zhang TM, Fu JD, Zhang JL, et al. Sphenoid wing meningioma en plaque: report of 37 cases. Chin Med J (Engl). 2009; 122:2423–2427. PMID:
20079153.
10. Boari N, Gagliardi F, Spina A, Bailo M, Franzin A, Mortini P. Management of spheno-orbital en plaque meningiomas: clinical outcome in a consecutive series of 40 patients. Br J Neurosurg. 2013; 27:84–90. PMID:
22905887.

11. Kashimura H, Beppu T, Wada T, Yoshida Y, Suzuki M, Ogawa A. [A case of meningioma en plaque: review of 73 cases]. No Shinkei Geka. 1997; 25:1097–1100. Japanese. PMID:
9430144.
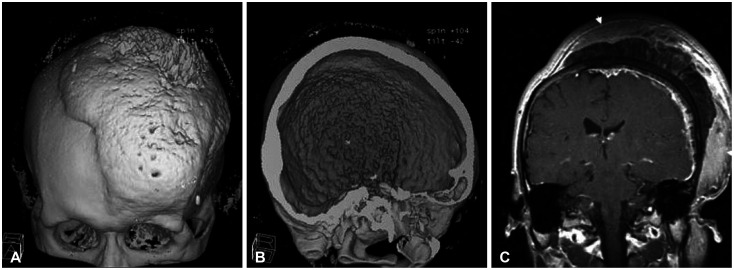
12. Akutsu H, Sugita K, Sonobe M, Matsumura A. Parasagittal meningioma en plaque with extracranial extension presenting diffuse massive hyperostosis of the skull. Surg Neurol. 2004; 61:165–169. discussion 169. PMID:
14751632.

13. Kim SM, Jang KS, Kim MC, Joo WI. Convexity meningioma en plaque presenting with diffuse hyperostosis of the skull. J Korean Neurosurg Soc. 2006; 39:159–161.
14. Leeds N, Seaman WB. Fibrous dysplasia of the skull and its differential diagnosis. A clinical and roentgenographic study of 46 cases. Radiology. 1962; 78:570–582. PMID:
14463598.

15. Pérez-Santonja JJ, Bueno JL, Serrano de la Iglesia JM, Zato MA, Queimadelos V, Ibarburen C. [Sphenoidal hyperostosis. Problems of differential diagnosis: report of a case]. Rev Clin Esp. 1992; 191:422–425. Spanish. PMID:
1336861.
16. Kim KS, Rogers LF, Lee C. The dural lucent line: characteristic sign of hyperostosing meningioma en plaque. AJR Am J Roentgenol. 1983; 141:1217–1221. PMID:
6606319.

17. Pieper DR, Al-Mefty O, Hanada Y, Buechner D. Hyperostosis associated with meningioma of the cranial base: secondary changes or tumor invasion. Neurosurgery. 1999; 44:742–746. discussion 746-7. PMID:
10201298.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download