Abstract
Purpose
This study aimed to compare the clinical performance of Medisonic (Daiwha Corp.) to that of Harmonic HD 1000i (Ethicon Endo-Surgery Inc.) and Sonicision (Medtronic) in patients undergoing gastrectomy for gastric cancer.
Methods
A total of 30 patients were enrolled in this prospective randomized study. The patients were randomly assigned to a Medisonic (M group, n = 10), Harmonic HD 1000i (H group, n = 10), or Sonicision (S group, n = 10) groups. Primary outcome was cutting speed and activation times during omentectomy. Other variables were visibility of surgical field, blade stickiness, and clinical outcomes, including operation-related complications.
Results
Clinicopathologic characteristics, including age, sex, body mass index, or stage were not different between the 3 groups. Operative outcomes, including operation time, estimated blood loss, and postoperative hospital stay were not different between the 3 groups. There was no significant difference in 30-day postoperative complications. The running time of omentectomy was 7.3, 9.2, and 8.7 minutes in the H, S, and M groups, respectively, with no statistical difference (P = 0.589). We also looked at the activation times during the omentectomy, and there was no statistical difference between the groups (52.6 times vs. 58.9 times vs. 56.2 times in the H, S, and M groups, respectively; P = 0.860).
Gastric cancer (GC) is one of the most common malignancies worldwide, and it is the third leading cause of cancer-related death [1]. Surgery is the only treatment of choice for GC, and appropriate lymph node dissection is crucial during the surgery [2]. With development of minimally invasive surgery, laparoscopic gastrectomy is now the standard treatment for early GC, and the indication has been recently expanded to advance cancer [3].
During laparoscopic gastrectomy, electrosurgical instruments have been developed for safe and effective hemostasis, vessel sealing, and tissue dissection. By using an energy device, it is very helpful to reduce the operation time when performing lymph node dissection during GC surgery, and as a result, improves the operation outcome [45]. The currently available energy devices used during laparoscopic gastrectomy are of 3 different energy-based methods: monopolar, bipolar, and ultrasonically activated electrosurgery.
Among them, ultrasonic coagulating shears (UCS) are made to perform cutting and attain hemostasis at once during operation. The ultrasonically activated scalpel works by generating high-frequency vibrations in a metallic rod, which denatures proteins [6]. It was proved that the introduction of UCS during laparoscopic gastrectomy significantly shortened the operating time, reduced the workload, and enabled stable surgery in terms of bleeding [789]. The most generally available ultrasonic energy devices in Korea are Sonicision (Medtronic) and Harmonic HD 1000i (Ethicon Endo-Surgery Inc.) from the United States.
Medisonic DU-3 series (Daiwha Corp.) is South Korea’s indigenously made ultrasonic energy device certified by the Ministry of Food and Drug Safety of the Republic of Korea (KFDA) and registered under the Korean Health Insurance System in 2018. Medisonic has a built-in transducer that allows the wheel to rotate 360° continuously without twisting the cable, which reduces the burden of medical expenses for patients without the need of purchasing a transducer separately (Fig. 1).
Although this device was approved by the KFDA, no clinical study has been performed to look at the efficacy and safety of Medisonic device for gastrectomy in patients with GC. Therefore, this study aimed to compare the utility and outcomes of Medisonic vs. Sonicision and Harmornic HD 1000i in radical gastrectomy for GC at a single Asian tertiary academic medical center.
This study was approved by the Institutional Review Board of The Catholic University of Korea, Seoul St. Mary’s Hospital. The study was conducted according to the relevant guideline regulations (No. KC21DNSS0333) and written informed consent was obtained from all the patients.
This was a pilot prospective randomized trial in a single tertiary academic institution. Between July and December 2021 at the Seoul St. Mary’s Hospital of the Catholic University of Korea, patients who were diagnosed with gastric adenocarcinoma, aged 20–75 years with Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, and anticipating laparoscopic surgery were included in this study after providing research informed consent. Patients with open surgery, previous abdominal surgeries, on anticoagulants prior to surgery, metastatic cancer, remnant GC, pregnant women, and those in whom the use of ultrasonic energy device is contraindicated were excluded from the study.
A total of 30 patients undergoing laparoscopic radical distal gastrectomy were randomized with equal chances into 1 of 3 groups: group M, Medisonic, group H, Harmonic HD 1000i, and group S, Sonicision. Patient characteristics, operative data, perioperative outcomes, and postoperative complications were observed and compared. All surgery videos were recorded and analyzed to evaluate the efficacy and safety by 2 independent surgeons (AG and SJK).
The operation was performed by 1 surgeon (KYS) with UCS, depending on the randomized arm. For the laparoscopic imaging instruments, we used Visera Elite II video system and camera head (Olympus). For all the patients, standard total laparoscopic distal gastrectomy with D1+ or D2 lymphadenectomy according to the Korean Gastric Cancer Guideline was performed [10]. During the surgery, the greater omentum was divided proximally to approximately 4–5 cm from the gastroepiploic arcade towards the lower pole of the spleen using laparoscopic ultrasonic shears. After dissection of lymph nodes around the right gastroepiploic vessels, the duodenum was divided using laparoscopic stapler. For the D1+ or D2 lymphadenectomy, the suprapancreatic lymph nodes, including stations #7, 8a, 9, 11p, and 12a were dissected. After clearing the lymph nodes along the lesser curvature, the stomach was divided and a specimen was removed via an extended umbilical wound. Reconstruction was performed, with either gastroduodenostomy or gastrojejunostomy, using a laparoscopic stapler. Postoperatively, the patients were managed routinely based on a critical pathway of the hospital.
Primary outcome of this study was to observe the efficacy and safety of the instrument. Duration and activation times of omentectomy were recorded and measured via prerecorded video analysis. The omentectomy was defined from the start of omentectomy to the division of the left gastroepiploic vessels. Activation times were the number of times the tissue was sealed and energy delivered using an instrument. The time taken for each activation was assumed to be similar because a single surgeon performed the operations. Four major arteries, i.e., the right gastric, right gastroepiploic, left gastric, and left gastroepiploic arteries were cut with UCS, and the time taken to cut them was measured through the video analysis. To evaluate the safety of patients, operation-related outcomes, including operation time, estimated blood loss, postoperative hospital stay, and operation-related complications were compared.
Apart from the efficacy of the instrument, 3 characteristics considered to be factors that make the surgical team feel at ease during surgery are as follows: (1) visibility, (2) blade stickiness, and (3) number of times of lens cleansing. Visibility was defined as the degree to which the surgical fields were obscured by the fog/smoke caused by using UCS during omentectomy. If there is fog spreading all over the screen for <10 seconds, it was defined as moderate fogging. Severe fogging meant fog was maintained over 10 seconds and the number of times each fogging was measured (Fig. 2). The blade stickiness was defined as the degree of tissue attached to the blade of the instrument, which was classified as mild, moderate, and severe. If the tissue adherence to the blade is <50% of the length of the blade, it was defined as mild, while 50%–70% was moderate, and 70% or more was severe (Fig. 3). The number of measurements of mild, moderate, and severe was compared when 30 minutes had elapsed from the start of the operation. The times of cleansing defined the number of times the scope lens was removed from the body and cleaned for any reason during the omentectomy.
One-way analysis of variance with Bonferroni post hoc analysis or unpaired two-sample Student t-test was used to investigate the differences in continuous variables among different groups. Fisher exact test was used to compare categorical variables. The analysis was conducted using IBM SPSS Statistics for Windows (ver. 24, IBM Corp.), and statistical significance was accepted for P-values of <0.05.
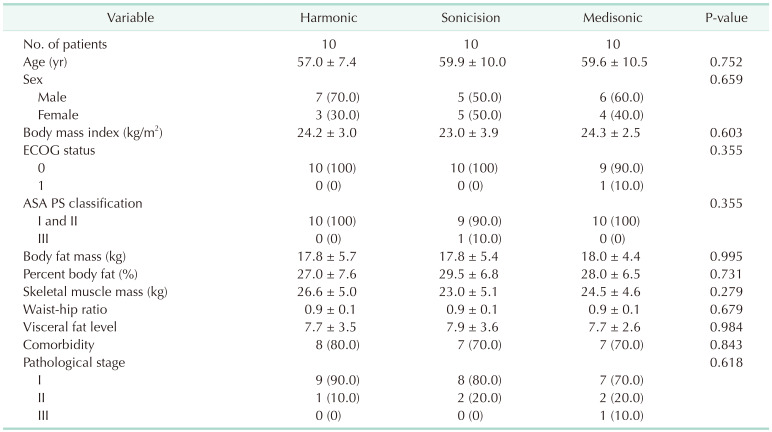
The patient’s clinical characteristics are shown in Table 1. The mean patient age was 58.8 ± 9.2 years, and there was no difference between the groups. Sex, body mass index, body fat mass, and skeletal muscle mass were not different between groups. Patients’ ECOG performance status, American Society of Anesthesiologists physical status classification, and presence of comorbidity were also not different.
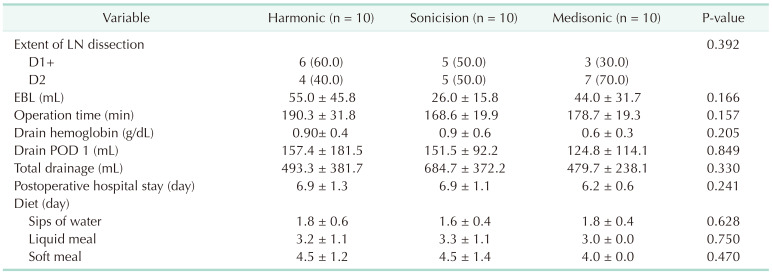
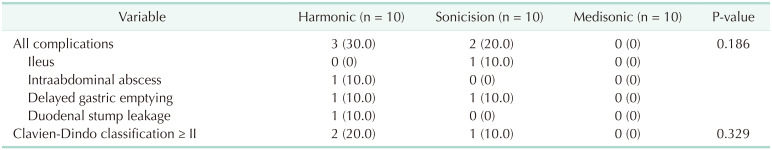
The extent of lymph node dissection and type of reconstruction were not different between the groups (Table 2). The operation times were not significantly different (178.7 ± 19.3 minutes in the M group, 190.3 ± 31.8 minutes in the H group, and 168.6 ± 19.9 minutes in the S group; P = 0.157). The estimated blood loss was also not significantly different between the groups (44.0 ± 31.7 mL in the M group, 55.0 ± 45.8 mL in the H group, and 26.0 ± 15.8 mL in the S group; P = 0.166). The postoperative hospital stay was also not significantly different between the groups. Intra- and postoperative complication rates were not different between the groups (Table 3).
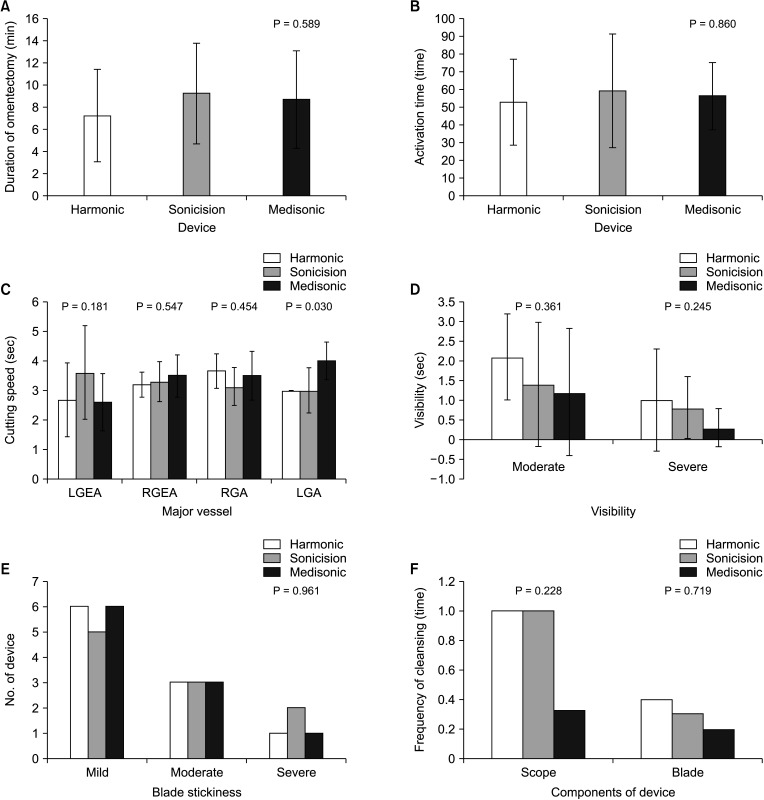
We measured the duration from the start of omentectomy to the division of the left gastroepiploic vessels to evaluate the cutting speed of each instrument. There were no significant differences between the groups (8.7 ± 4.4 minutes in the M group, 7.3 ± 4.2 minutes in the H group, and 9.2 ± 4.5 minutes in the S group; P = 0.589) (Fig. 4A). The activation times during the omentectomy were measured via the video analysis, and there were no significant differences between the groups (56.2 ± 19.0 times in the M group, 52.6 ± 24.1 times in the H group, and 58.9 ± 32.0 times in the S group; P = 0.860) (Fig. 4B).
We cut 4 major blood vessels around the stomach using UCS, and the time taken for the cutting was measured using the video analysis and compared for each group. Although the time to cut the other 3 arteries did not differ between the groups, the time to cut the left gastric artery was significantly longer in group M (4.0 ± 0.6 seconds in the M group, 3.0 ± 0.0 seconds in the H group, and 3.0 ± 0.8 seconds in the S group; P = 0.030) (Fig. 4C).
Visibility count showed a rather high trend in the H group but was not statistically significant (P = 0.361) (Fig. 4D). The blade stickiness and times of lens cleansing were not significantly different between the groups (P = 0.961 and P = 0.228, respectively) (Fig. 4E, F).
Lymph node dissection is a very important process that determines patient’s prognosis during gastrectomy in GC patients. Because GC metastasizes to the lymph node of D2 level, as well as the lymph nodes around the stomach, it is necessary to remove the lymph nodes safely and reliably in a very complex and dangerous area during the operation of patients with advanced GC [11]. In particular, the lymph nodes of the suprapancreatic area are technically challenging to completely resect because they are tightly attached to major blood vessels, such as the hepatic and splenic arteries, which are located above/behind the pancreas. Therefore, when the resection is excessive, it can cause complications, such as bleeding, and when it is insufficient, the R0 resection can fail due to improper dissection of the lymph node. In the past open surgery era, electrosurgery methods were mainly used, which was possible because the existing scalpel and scissors could be used and the blood vessels could be ligated with a thread [12].
Because laparoscopic surgery was introduced and popularized during GC surgeries, several tools to replace electrosurgery were developed. The most important and innovative device is the UCS. With the development of this instrument capable of cutting and securing hemostasis by sealing at the same time, laparoscopic surgery has become safer and faster, and the indications for more diverse patients are being expanded. In cancer surgery, lymph node dissection can cause postoperative ascites or lymphorrhea due to leakage of lymphatic fluid, and UCS helps prevent these complications with sealing action [13].
Representative UCS equipment are Harmornic HD 1000i (Ethicon Endo-Surgery Inc.) and Sonicision (Medtronic). These 2 devices produced in the United States are widely used all over the world, and the Thunderbeat made by Olypmpus of Japan is competing recently. Thunderbeat is a device that has a different mechanism from the above 2 by adding an advanced bipolar function compared to other UCS devices to strengthen hemostasis and sealing functions [14]. We conducted a pilot clinical trial to see if there was any difference in efficacy and safety of existing UCS devices compared to Medisonic, which was developed and used in Korea for the first time.
Medisonic is South Korea’s indigenously made ultrasonic energy device certified by the KFDA and registered under Korean Health Insurance System in 2018. The advantage of Korean products is that they do not feel heavy to Asian surgeons, especially to female surgeons, and the handpiece is compact compared to existing Western products. Medisonic is made up of lightweight materials; thus, it is much lighter than other competing products. Medisonic was designed ergonomically, thereby allowing Asian and female surgeons with relatively small hands as well as Western male surgeons to handle it easily.
In order to compare the efficacy and safety between instruments, the operation time, intraoperative blood loss, number of resected lymph nodes, postoperative hospital stay, and postoperative complications were compared as in a previous study [15]. The strength of this study is that we analyze more objective, specific, and direct factors through video analysis. We measured the cutting speed as the time taken from omentectomy to duodenal division. The reason for this was that UCS was used as a routine during omentectomy and comparison was possible under similar conditions during a certain procedure. Similarly, the number of activations of the UCS device was measured from the start of omentectomy to the division of the left gastroepiploic vessels. It was assumed that the higher the number of times, the lower the efficacy. In order to keep the time taken for each activation time to be same, only 1 surgeon activated it for each surgery.
Because the effect of the instrument was observed during the omentectomy, there was a possibility that the patient’s obesity, especially the proportion of abdominal fat, could affect the outcome. Therefore, in this study, body composition analysis was measured in all the patients using InBody 370s (InBody), including body fat mass, percent of body fat, and visceral fat level, and it was confirmed that there was no difference between the 3 groups. To reduce bias caused by the laparoscopic equipment, camera lens, and camera operator, 1 type of laparoscopic equipment and camera was used, and the same person (a surgical nurse) was also in charge of the camera operation.
There were no differences in the results that the instrument could affect, such as the operation time, amount of bleeding during the operation, and amount of drainage after the surgery. Additionally, there were no differences in the postoperative hospital stay, complication rate and time to start oral diet. There were no differences between the 3 groups either in the time taken for the omentectomy or in the activation time. The time required to cut the 4 major vessels was significantly longer in the Medisonic group, only in the left gastric artery.
In this study, the surgical video was analyzed to measure and compare the cutting and hemostasis, which are the most important functions of UCS. There are several important factors that cause complications when using UCS in practice: (1) how severe the smoke generated during surgery is; (2) the degree to which the tissue adheres to the blade and interferes with the operation; (3) and the degree to which foreign substances are splashed on the lens to be used. These factors do not directly affect the safety of the patient but have a great influence on the surgeon’s choice of instrument. There was no difference between the 3 instruments, but the Harmonic HD 1000i showed a tendency to generate more smoke.
This study has several limitations. First, the number of comparative study participants is small at 10 patients per instrument. Second, UCS is mainly used for cutting, sealing, and hemostasis, but it is now widely used for dissection. Among the characteristics of UCS, the cavitation effect and development of the instrument tip into a very sharp and curved shape is to facilitate such dissection. In this study, we did not compare the ease of such dissection.
In conclusion, Medisonic is safe and efficient to perform laparoscopic radical gastrectomy and is not inferior to Harmonic HD 1000i or Sonicision in terms of clinical outcomes and cutting/sealing function.
ACKNOWLEDGEMENTS
The authors thank Ha Neul Kim, the surgical nurse of Department of Gastrointestinal Surgery, for her assistant during operations.
Notes
References
1. Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020; 396:635–648. PMID: 32861308.

2. Johnston FM, Beckman M. Updates on management of gastric cancer. Curr Oncol Rep. 2019; 21:67. PMID: 31236716.

3. Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, et al. Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol. 2020; 38:3304–3313. PMID: 32816629.

4. Kim YN, Yoo YC, Guner A, Cho I, Kwon IG, Kim YN, et al. Comparison of perioperative surgical outcomes between a bipolar device and an ultrasonic device during laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2015; 29:589–595. PMID: 25015523.

5. Tsimoyiannis EC, Jabarin M, Tsimoyiannis JC, Betzios JP, Tsilikatis C, Glantzounis G. Ultrasonically activated shears in extended lymphadenectomy for gastric cancer. World J Surg. 2002; 26:158–161. PMID: 11865342.
6. Lee SH, Nguyen TK, Ong WS, Haaland B, Tay GC, Tan NC, et al. Comparing the utility and surgical outcomes of harmonic focus ultrasonic scalpel with ligasure small jaw bipolar device in thyroidectomies: a prospective randomized controlled trial. Ann Surg Oncol. 2019; 26:4414–4422. PMID: 31512024.

7. Inoue K, Nakane Y, Michiura T, Yamada M, Mukaide H, Fukui J, et al. Ultrasonic scalpel for gastric cancer surgery: a prospective randomized study. J Gastrointest Surg. 2012; 16:1840–1846. PMID: 22833440.

8. Cheng H, Hsiao CW, Clymer JW, Schwiers ML, Tibensky BN, Patel L, et al. Gastrectomy and D2 lymphadenectomy for gastric cancer: a meta-analysis comparing the harmonic scalpel to conventional techniques. Int J Surg Oncol. 2015; 2015:397260. PMID: 26075090.

9. Huang Y, Mu GC, Qin XG, Lin JL, Liu C, Chen ZB, et al. The application of ultrasonic harmonic scalpel in the radical surgery of gastric cancer. Clin Transl Oncol. 2013; 15:932–937. PMID: 23519537.

10. Guideline Committee of the Korean Gastric Cancer Association (KGCA). Development Working Group & Review Panel. Korean practice guideline for gastric cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019; 19:1–48. PMID: 30944757.
11. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021; 24:1–21. PMID: 32060757.
12. Chen XL, Chen XZ, Lu ZH, Wang L, Yang K, Hu JK, et al. Comparison of ultrasonic scalpel versus conventional techniques in open gastrectomy for gastric carcinoma patients: a systematic review and meta-analysis. PLoS One. 2014; 9:e103330. PMID: 25079780.

13. Matthey-Gié ML, Gié O, Deretti S, Demartines N, Matter M. Prospective randomized study to compare lymphocele and lymphorrhea control following inguinal and axillary therapeutic lymph node dissection with or without the use of an ultrasonic scalpel. Ann Surg Oncol. 2016; 23:1716–1720. PMID: 26714939.

14. Suzuki K, Shimizu M, Sakagami T, Yagi M, Fujisawa T, Sawada S, et al. A comparison of short-term outcomes of neck dissection for head and neck cancers using Thunderbeatκ, LigaSureκ or treatment without an energy-based device: a case controlled study. Int J Surg. 2018; 58:60–64. PMID: 30248411.

15. Kim WW, Cho J, Jeon YS, Kim I, Jeong YJ, Choi J, et al. Prospective, randomized, comparative, multicenter study of the hybrid ultrasonic advanced bipolar device and the ultrasonic coagulating shears in open thyroidectomy. Surg Innov. 2021; 28:41–47. PMID: 32757879.

Fig. 1
Medisonic DU-3 device (Daiwha Corp.) has a built-in transducer that allows the wheel to rotate 360° continuously without twisting the cable.

Fig. 2
Representative photos by the degree of visibility. Visibility was defined as the degree to which the surgical fields were obscured by the fog/smoke caused by using ultrasonic coagulating shears during the omentectomy. (A) Moderate, fog spreading all over the screen for <10 seconds; (B) severe, fog was maintained over 10 seconds.
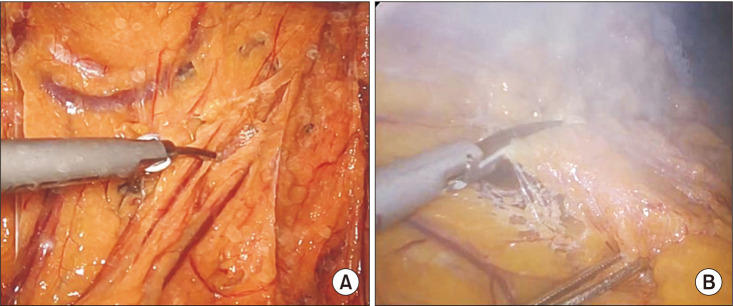
Fig. 3
Representative photos by the degree of stickiness. The blade stickiness was defined as the degree of tissue attached to the blade of the instrument and was classified as mild, moderate, and severe. (A) Mild, <50% of the blade; (B) moderate, between 50% and 70% of the blade; and (C) severe, >70% of the blade.
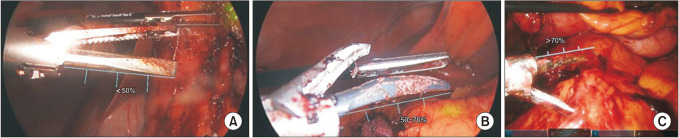
Fig. 4
Main outcomes. (A) Duration of omentectomy. (B) Activation times during the omentectomy. (C) Cutting speed for dividing the 4 major gastric arteries. (D) Visibility of the operation fields. (E) Blade stickiness after 30 minutes of operation. (F) Times of lens cleansing during the omentectomy. Harmonic, Ethicon Endo-Surgery Inc.; Sonicision, Medtronic; Medisonic, Daiwha Corp. The number of patients for each device is 10. LGEA, left gastroepiploic artery; RGEA, right gastroepiploic artery; RGA, right gastric artery; LGA, left gastric artery.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download