Abstract
Purpose
Surgeons have become increasingly interested in reduced-port gastrectomy to minimize trauma while maintaining oncologic safety. Although gastroduodenostomy has the benefits of better nutritional outcomes and fewer postoperative complications than other types of reconstruction, gastroduodenostomy is not a preferred option for reduced-port distal gastrectomy because of technical difficulties. In this study, we describe our intracorporeal modified delta-shaped gastroduodenostomy technique, which is easily applicable during 2-port distal gastrectomy.
Methods
We retrospectively reviewed our database of 30 consecutive patients with gastric cancer who underwent 2-port distal gastrectomy with intracorporeal modified delta-shaped gastroduodenostomy from October 2016 to May 2021. In this reduced-port approach, we used a Tropian Single port (TROPIAN TECH) via a 25-mm transumbilical incision and a 12-mm port at the right flank. All anastomoses were performed using a 60-mm endolinear stapler. We used 3 additional sutures to provide proper traction and support for the anastomosis.
Results
Mean ± standard deviation of operation time was 148.9 ± 34.7 minutes; reconstruction time was 13.2 ± 4.6 minutes; estimated blood loss was 29.3 ± 44.4 mL; and length of hospital stay was 4.5 ± 1.2 postoperative days. A total of 11 patients (36.7%) had a Clavien-Dindo grade I or grade II complication, and there were no grade IIIa or higher complications.
Laparoscopic gastrectomy has become a standard treatment option for gastric cancer, as it provides better short-term surgical outcomes while maintaining oncologic safety [12]. Conventional laparoscopic gastrectomy generally required the use of 5 ports to obtain adequate access and support from assistants [3]. Recently, there has been considerable interest in reducing the number of ports to enhance the benefits of minimally invasive surgery by minimizing surgical stress and reducing postoperative scarring [4].
For distal gastrectomy, gastroduodenostomy has advantages over other types of reconstructions, such as loop or Roux-en-Y gastrojejunostomy. Gastroduodenostomy allows food passage through the duodenum, providing a route for iron absorption [5]. Additionally, postoperative complications associated with intestinal obstruction are less frequent after gastroduodenostomy than after other types of anastomoses [6]. However, gastroduodenostomy is not the preferred reconstruction technique during reduced-port gastrectomy [7]. Technical difficulties associated with performing intracorporeal anastomosis in a limited working space and with a reduced number of accesses are major barriers to the use of gastroduodenostomy during reduced-port distal gastrectomy. In this study, we described an intracorporeal modified delta-shaped gastroduodenostomy technique that can be easily performed during 2-port distal gastrectomy. We also present our initial experience of 30 consecutive patients who underwent this anastomotic technique.
The Institutional Review Board of Severance Hospital, Yonsei University Health System approved the protocol (No. 4-2021-0942) and waived the requirement for informed consent because of the retrospective nature of the study. Written informed consent was obtained from the patients for the publication clinical image and video.
We retrospectively reviewed data from patients who underwent intracorporeal modified delta-shaped gastroduodenostomy during 2-port distal gastrectomy for gastric cancer at the Department of Surgery, Yonsei University College of Medicine. A total of 30 consecutive patients underwent this procedure from October 2016 to May 2021. All the operations included in this study were performed by a single surgeon who had experience with 150 cases of intracorporeal delta-shaped gastroduodenostomy in conventional laparoscopic distal gastrectomy by 2016. We analyzed clinicopathologic features and perioperative surgical outcomes, including demographic data, operative findings, pathologic results, and postoperative recovery details.
All patients underwent 2-port robot-assisted laparoscopic distal gastrectomy. Specifically, lymph node dissection was performed via a robotic approach, and transection of the stomach and reconstruction were performed via a laparoscopic approach. The detailed procedures for gastrectomy and lymph node dissection using 2 ports have been described previously [89].
After completion of robotic lymphadenectomy, the robot was undocked, and the surgeon performed laparoscopic intracorporeal modified delta-shaped gastroduodenostomy. The Single-Site port (Intuitive Surgical) at the umbilicus for robotic surgery was removed, and the Tropian Single port (TROPIAN TECH) was inserted into the transumbilical incision site. A 12-mm port was inserted in the right flank (Fig. 1). The anastomosis was performed using 60-mm endolinear staplers.
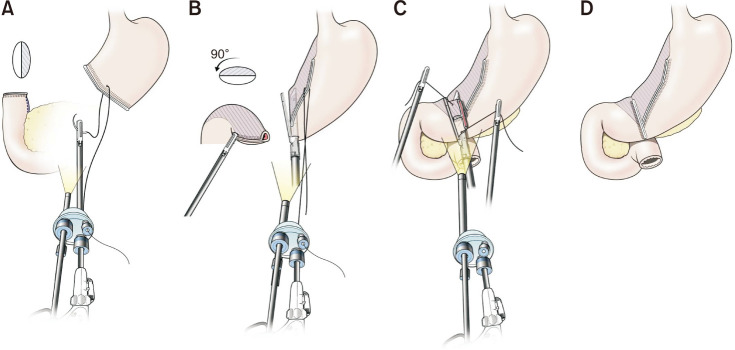
A traction suture was added at the middle of the artificial lesser curvature line, and the thread was pulled out of the abdomen through the transumbilical port (Fig. 2A). A small incision for insertion of the anvil was made on caudal side of the duodenum, and a small incision for insertion of the endolinear stapler cartridge was created on the edge of the greater curvature of the remnant stomach (Fig. 2B). Using traction with the thread and being guided by a grasper manipulated by the operator’s left hand through the 12-mm port at the right flank, we easily inserted the cartridge of the endolinear stapler into the remnant stomach. The linear stapler held the posterior side of the remnant stomach between the cartridge and anvil. Then the shaft was rotated clockwise to approximate the posterior wall of the stomach and duodenum. The anvil was inserted into the hole made at the duodenum, with the full length of the anvil being inserted to ensure a large anastomosis. Before performing the anastomosis, the loose connective tissue between the cephalic side of the duodenum and the pancreas was fully detached. The anvil was introduced into the duodenum while the tip was carefully inserted toward the luminal side, not the cephalic side, to avoid the possibility of the tip perforating the duodenal wall. When the stapler was fired after inserting the anvil, the traction suture at the stomach-maintained traction to prevent the cartridge from falling off the stomach. This traction suture was subsequently removed after firing the stapler. A multifilament absorbable 3-0 suture was used as traction sutures at both the anterior and posterior sides of the common entry hole. These 2 sutures were lifted toward the ventral side; one was lifted by the assistant through the transumbilical port, and the other was lifted by the operator’s left hand through the 12-mm port at the right flank. The entry hole was then closed using a 60-mm endolinear stapler (Fig. 2C). Thus, the intracorporeal modified delta-shaped gastroduodenostomy was completed, without a “dog ear” at the duodenum (Fig. 2D, Supplementary Video 1).
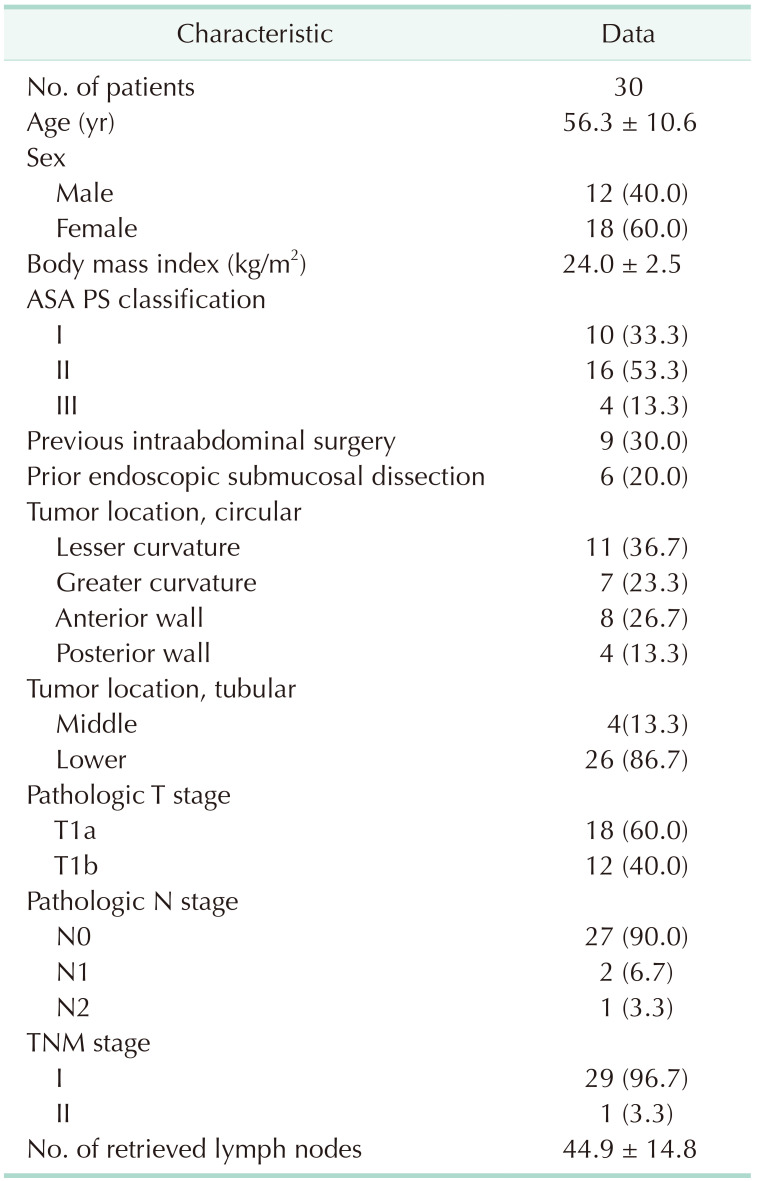
The mean patient age was 56.3 years (standard deviation [SD], 10.6), and the majority of patients were female (60.0%). The mean body mass index was 24.0 kg/m2 (SD, 2.5). Of the 30 patients in the study, 9 patients (30%) had prior intra-abdominal surgery, and 6 patients (20%) underwent endoscopic submucosal dissection before surgery. Most tumors (86.7%, 26 patients) were located in the lower third of the stomach, whereas 13.3% of tumors (4 patients) were in the middle third of the stomach. Depth of invasion of all tumors was T1 (60% were T1a, 40% were T1b), and 3 patients (10.0%) had lymph node metastasis. The mean number of retrieved lymph nodes was 44.9 (SD, 14.8) (Table 1).
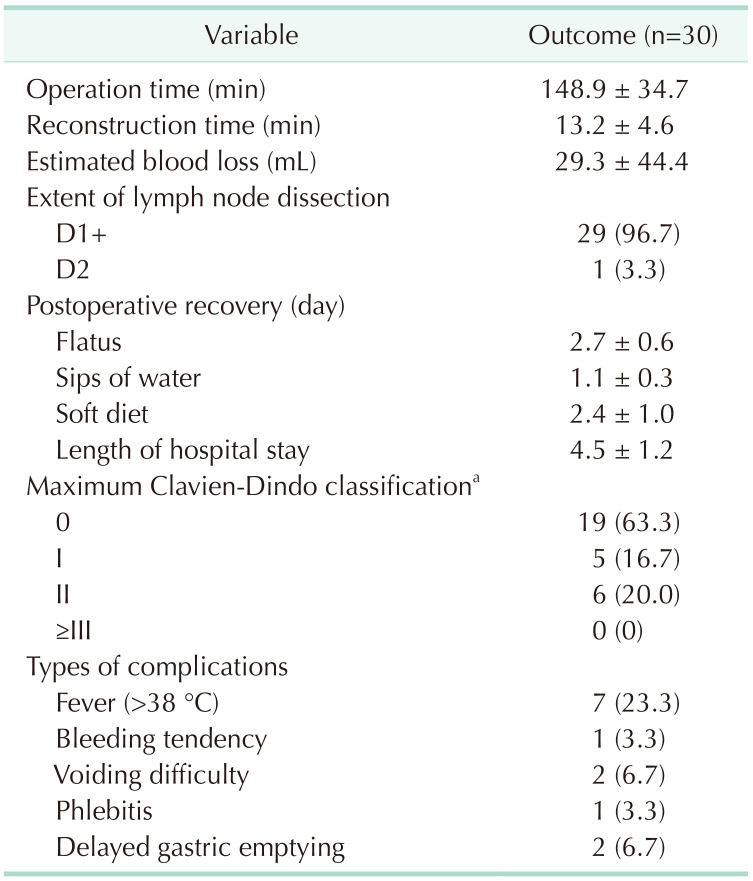
The mean operation time was 148.9 minutes (SD, 34.7), and the mean reconstruction time was 13.2 minutes (SD, 4.6). The mean estimated blood loss was 29.3 mL (SD, 44.4). We performed D1+ lymph node dissection in 29 patients (96.7%), while 1 patient (3.3%) underwent D2 lymph node dissection because of suspected lymph node metastasis during surgery. The time to first flatus after surgery was 2.7 postoperative days (SD, 0.6). The time to first water intake was 1.1 postoperative days (SD, 0.3), and the time to first soft diet was 2.4 postoperative days (SD, 1.0). The mean hospital length of hospital stay was 4.5 postoperative days (SD, 1.2).
A total of 11 patients (36.7%) had Clavien-Dindo grade I or grade II complications, and there was no grade IIIa or higher complication. The most common complication was fever (7 patients, 23.3%). One patient had a bleeding tendency during surgery and received tranexamic acid in the immediate postoperative period. Two patients (6.7%) had voiding difficulty, and one patient (3.3%) had phlebitis. Two patients had an unscheduled revisit of the hospital after discharge because of delayed gastric emptying and they returned home on the visit day as symptoms resolved spontaneously (Table 2).
In this study, we described a technique for intracorporeal modified delta-shaped gastroduodenostomy during 2-port distal gastrectomy. In our initial experience, this technique provided acceptable short-term surgical outcomes, in terms of operation time, reconstruction time, estimated blood loss, and hospital stay. There were no major complications, including anastomosis-related complications such as anastomotic leakage or stenosis. These results suggest that our intracorporeal modified delta-shaped gastroduodenostomy technique during 2-port distal gastrectomy would be safe and feasible.
Intracorporeal gastroduodenostomy, the so-called delta-shaped anastomosis, was first reported in Japan during conventional laparoscopic distal gastrectomy using 5 ports [3]. To perform delta-shaped anastomosis, multiple accesses for the operator and assistant were necessary because the duodenum and stomach required appropriate retraction from multiple directions at the same time. However, reduced-port gastrectomy has a restricted number of access points because of lower number of ports. Moreover, instrument collision occurs when an additional grasper is added through a transumbilical port. Thus, it is technically challenging to perform intracorporeal gastroduodenostomy in reduced-port gastrectomy. For these reasons, gastroduodenostomy was not preferred over loop or Roux-en-Y gastrojejunostomy in most previous studies of reduced-port gastrectomy [1011121314].
In our technique, we used 3 additional sutures to provide proper support for the anastomosis. The first suture at the artificial lesser curvature line of the remnant stomach-maintained traction toward the ventral side. Without this traction, the cartridge located in the stomach is displaced while opening the jaw to insert the anvil into the duodenum. The other 2 sutures provided the appropriate angle for closure of the common entry hole. The 3 traction sutures facilitated pulling of the stomach and duodenum in various directions, thereby allowing intracorporeal gastroduodenostomy to be performed with a limited number of ports.
Our technique can be applied to other types of reduced-port gastrectomy as well. A similar technique of intracorporeal gastroduodenostomy was reported previously in single-port distal gastrectomy, using 2 additional sutures for manipulation of the remnant stomach and the common entry hole [15]. However, in that technique, only the posterior suture lifted the common entry hole toward the ventral side, whereas the anterior suture just pulled the common entry hole in the direction of the stapler. We recommend lifting both the anterior and posterior side of the common entry hole toward the ventral side, as in our technique, to ensure easy and safe closure of the hole.
Besides, we used a 60-mm linear stapler for gastroduodenostomy and inserted the full length of the stapler into the stomach and duodenum to ensure a large anastomosis. In previous studies of intracorporeal gastroduodenostomy, a 45-mm linear stapler was usually used for gastroduodenal continuity [3]. No study has evaluated the most appropriate length of linear stapler for use during intracorporeal gastroduodenostomy. A longer linear stapler creates a wider anastomosis, which may reduce the likelihood of anastomotic stricture after gastroduodenostomy. Moreover, the stapling line on the duodenum is completely resected in our technique, which is of relevance because the remnant staple line could be a weak point because of tissue ischemia [16]. It is preferable to remove tissue with a high risk of ischemia to reduce the likelihood of anastomotic leakage.
The study had some limitations. The number of patients was relatively low, and all procedures were performed by a single surgeon. Further comparative studies are necessary to confirm the safety and benefits of this procedure.
In this study, we described a technique for intracorporeal modified delta-shaped gastroduodenostomy during 2-port distal gastrectomy. This technique provides appropriate traction of the stomach and duodenum in various directions despite the limited number of ports during intracorporeal gastroduodenostomy. In our analysis of 30 consecutive procedures, the technique was found to be feasible and safe, in terms of short-term surgical outcomes. These results suggest that using our technique, intracorporeal gastroduodenostomy can be considered more frequently during reduced-port distal gastrectomy.
Notes
References
1. Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg. 2016; 263:28–35. PMID: 26352529.

2. Kim HH, Han SU, Kim MC, Kim W, Lee HJ, Ryu SW, et al. Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol. 2019; 5:506–513. PMID: 30730546.

3. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002; 195:284–287. PMID: 12168979.

4. Inaki N, Tsuji T, Doden K, Sakimura Y, Tawara H, Matsui R, et al. Reduced port laparoscopic gastrectomy for gastric cancer. Transl Gastroenterol Hepatol. 2016; 1:38. PMID: 28138605.

5. Lee JH, Hyung WJ, Kim HI, Kim YM, Son T, Okumura N, et al. Method of reconstruction governs iron metabolism after gastrectomy for patients with gastric cancer. Ann Surg. 2013; 258:964–969. PMID: 23324857.

6. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005; 92:1099–1102. PMID: 15931657.

7. Information Committee of Korean Gastric Cancer Association. Korean Gastric Cancer Association Nationwide Survey on Gastric Cancer in 2014. J Gastric Cancer. 2016; 16:131–140. PMID: 27752390.
8. Lee S, Kim JK, Kim YN, Jang DS, Kim YM, Son T, et al. Safety and feasibility of reduced-port robotic distal gastrectomy for gastric cancer: a phase I/II clinical trial. Surg Endosc. 2017; 31:4002–4009. PMID: 28205030.

9. Roh CK, Choi S, Seo WJ, Cho M, Choi YY, Son T, et al. Comparison of surgical outcomes between integrated robotic and conventional laparoscopic surgery for distal gastrectomy: a propensity score matching analysis. Sci Rep. 2020; 10:485. PMID: 31949219.

10. Ahn SH, Son SY, Jung DH, Park DJ, Kim HH. Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg. 2014; 219:933–943. PMID: 25256369.

11. Usui S, Tashiro M, Haruki S, Matsumoto A. Triple-incision laparoscopic distal gastrectomy for the resection of gastric cancer: comparison with conventional laparoscopy-assisted distal gastrectomy. Asian J Endosc Surg. 2014; 7:197–205. PMID: 24767611.

12. Kim SM, Ha MH, Seo JE, Kim JE, Choi MG, Sohn TS, et al. Comparison of Reduced Port Totally Laparoscopic Distal Gastrectomy (Duet TLDG) and Conventional Laparoscopic-Assisted Distal Gastrectomy. Ann Surg Oncol. 2015; 22:2567–2572. PMID: 25564174.

13. Lee HH, Jeong O, Seo HS, Choi MG, Ryu SY, Sohn TS, et al. Long-term oncological outcomes of reduced three-port laparoscopic gastrectomy for early-stage gastric carcinoma: a retrospective large-scale multi-institutional study. J Gastric Cancer. 2021; 21:93–102. PMID: 33854817.

14. Lee B, Youn SI, Lee K, Won Y, Min S, Lee YT, et al. Comparing the short-term outcomes and cost between solo single-incision distal gastrectomy and conventional multiport totally laparoscopic distal gastrectomy for early gastric cancer: a propensity score-matched analysis. Ann Surg Treat Res. 2021; 100:67–75. PMID: 33585351.
15. Suh YS, Park JH, Kim TH, Huh YJ, Son YG, Yang JY, et al. Unaided stapling technique for pure single-incision distal gastrectomy in early gastric cancer: unaided delta-shaped anastomosis and uncut Roux-en-Y anastomosis. J Gastric Cancer. 2015; 15:105–112. PMID: 26161283.

16. Omori T, Masuzawa T, Akamatsu H, Nishida T. A simple and safe method for Billroth I reconstruction in single-incision laparoscopic gastrectomy using a novel intracorporeal triangular anastomotic technique. J Gastrointest Surg. 2014; 18:613–616. PMID: 24297650.

SUPPLEMENTARY MATERIALS
Supplementary Video 1 can be found via https://doi.org/10.4174/astr.2023.105.3.172.
Fig. 2
Intracorporeal modified delta-shaped gastroduodenostomy during 2-port distal gastrectomy. (A) A traction suture was added at the middle of artificial lesser curvature line, and the thread was pulled out of the abdomen through the transumbilical port. (B) The endolinear stapler cartridge was inserted into the stomach and rotated to approximate the posterior wall of the stomach and duodenum. (C) The common entry hole was closed while lifting the traction sutures at the anterior and posterior sides of the entry hole. (D) Completed intracorporeal modified delta-shaped gastroduodenostomy.




 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download