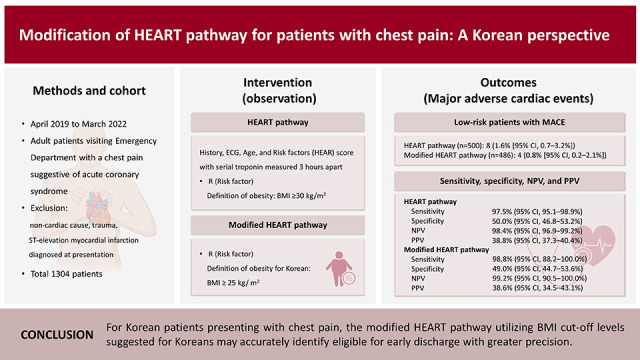
INTRODUCTION
Chest pain is one of the most common presenting symptoms in the emergency department (ED), always being a concern for both patients and physicians. It is essential to accurately risk stratify these patients because a missed diagnosis of an acute coronary syndrome (ACS) can lead to major adverse outcomes, including death and medico-legal exposure.
1) Scrutinizing these patients to rule out ACS is imperative; however, seeking tools to facilitate the safe discharge of low-risk patients is also crucial since overdiagnosis and unnecessary treatment could result in redundant patient burden and high medical costs.
2)3) The History, Electrocardiography, Age, Risk factors, and Troponin (HEART) pathway is a validated accelerated diagnostic protocol (ADP) designed to identify low-risk patients for early discharge without stress testing.
4) It incorporates History, Electrocardiography, Age, and Risk factors (HEAR) score with serial troponin levels measured 3 hours apart. Studies have demonstrated that the HEART pathway can reduce unnecessary testing and hospitalization up to 35–45% while maintaining a negative predictive value (NPV) for a major adverse cardiac event (MACE) rate of >99% at 30 days.
4) When calculating HEAR score, the risk “R” component includes hypertension, diabetes, hyperlipidemia, smoking, family history of coronary artery disease (CAD), and obesity defined with a body mass index (BMI) of ≥30 kg/m
2. Obesity is associated with a high risk of morbidity and mortality in the general population and is a significant independent risk factor for cardiovascular disease.
5) However, it is generally well known that the mean or median BMI of Asians is lower than that observed for non-Asian populations, shifting the BMI distribution to the left. Furthermore, the proportion of Asian people with a high risk of cardiovascular disease is substantial at BMIs lower than the existing World Health Organization (WHO) cut-off point.
6) Therefore, the Korean Society for the Study of Obesity proposed the BMI cut-off levels of 25 kg/m
2 and 23 kg/m
2, respectively, as diagnostic criteria for obesity and overweight (pre-obese) in Korean adults.
7)
In this study, we modified the R component by replacing the diagnostic criteria for obesity with cut-off levels of 25 kg/m2. The goal of this study was to perform an external validation of the original and modified HEART pathway for the prediction of MACE in Korean population.
METHODS
Ethical statement
This study was approved by the institutional review board (IRB No 2019-1130) of Asan Medical Center, and all participants provided written informed consent.
Study design
Adult patients (aged >18 years), who presented with chest pain suggestive of ACS to ED of Asan Medical Center from April 2019 to March 2022, were prospectively recruited in this observational study. Asan Medical Center is a tertiary medical center in Seoul, Korea, with an annual ED census of around 120,000 patients. Chest pain from an apparent non-cardiac cause, trauma, or ST-elevation myocardial infarction diagnosed at presentation was not included.
When a patient presents to our ED with chest pain suggestive of cardiac origin, electrocardiography (ECG) is performed along with a serial troponin assay at a 2-hour interval. We use a standardized chest pain evaluation form, including the patient's demographic data, height, weight, cardiovascular risk factors, family history, medical history, and current medication. Information on chest pain characteristics, including quality of pain, number of episodes, severity, location, radiation, duration, aggravating/relieving factors, and associated symptoms, are gathered. Based on the Diamond–Forrester prediction rule, including components of: 1) substernal chest pain, 2) worsening with physical activity, and 3) relief of symptoms with rest, chest pain was categorized into typical (all three present), atypical (two present), and non-anginal pain (one or none present).
HEAR scores were computed twice from the collected data, first utilizing a BMI of ≥30 kg/m
2 to define obesity as a risk factor and second employing a BMI cut-off of 25 kg/m
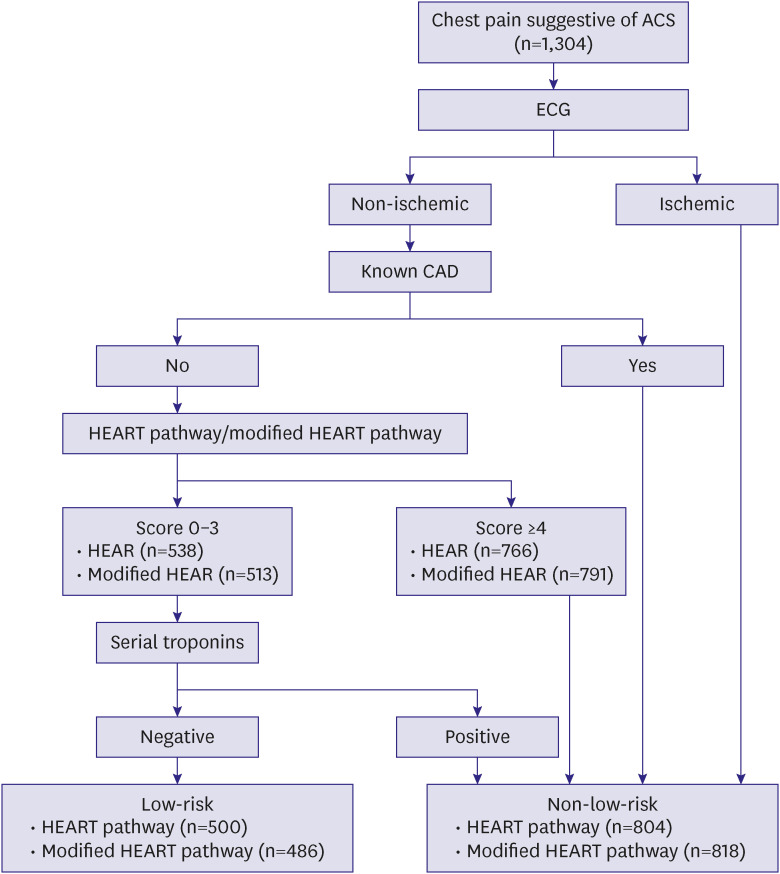
2. A HEAR score of 0 to 3 is consistent with a low-risk assessment, while a score of ≥4 is consistent with a high-risk one. HEART pathway and modified HEART pathway were calculated based on HEAR score combined with ECG findings and 0- and 2-hour troponin level measurements. (
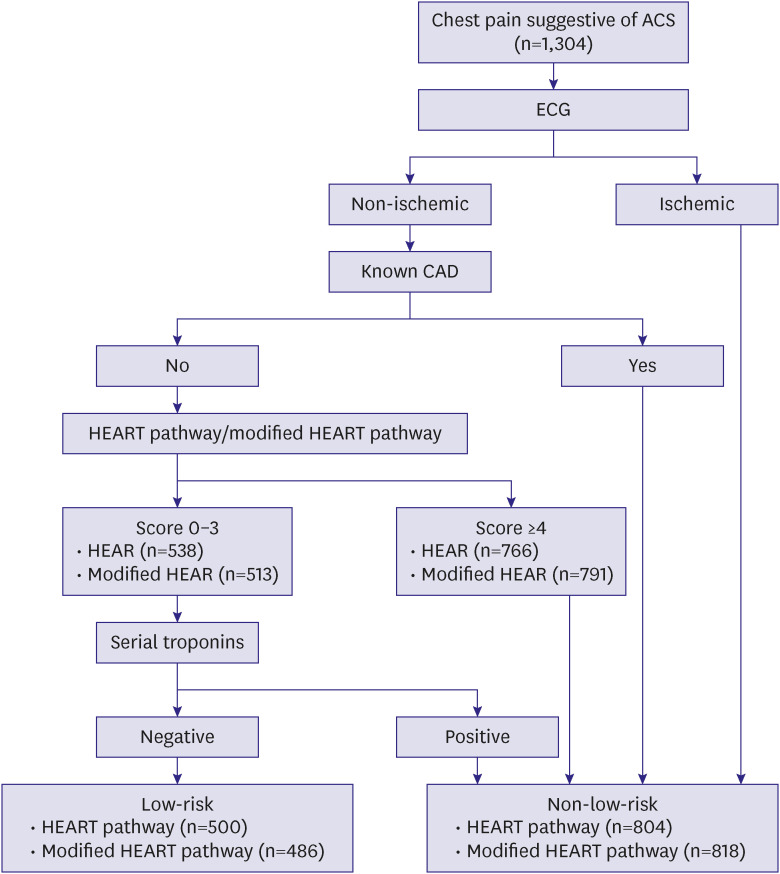
Supplementary Table 1). Patients with known CAD or acute ischemic changes on ECG (new T-wave inversion or ST-segment depression in contiguous leads) were classified as non-low-risk regardless of HEAR score (
Figure 1). CAD was defined as a previous episode of acute myocardial infarction (AMI), coronary artery bypass graft (CABG), or percutaneous coronary intervention (PCI). Cardiac high-sensitivity troponin I (hsTnI) was used for troponin measurement using the Atellica IM High-Sensitivity Troponin I assay (Atellica
® hsTnI; Siemens Healthineers, Erlangen, Germany; the 99th percentile URL 0.06 ng/mL). A MACE was defined as a diagnosis of AMI, receiving PCI, CABG surgery, and all-cause death. The primary outcome was MACE within 30 days of ED presentation. The definition of AMI was followed by the 4th universal definition of myocardial infarction.
8) When there was no documentation of MACE in the patient’s follow-up medical records or record of death from a national health events search, we considered this case as MACE-negative.
Figure 1
Flow diagram of HEART and modified HEART pathway for chest pain patient.
Patients with known CAD or acute ischemic changes on ECG (new T-wave inversion or ST-segment depression in contiguous leads) were classified as non-low-risk regardless of HEAR score.
ACS = acute coronary syndrome; CAD = coronary artery disease; ECG = electrocardiography; HEAR = History, Electrocardiography, Age, and Risk factors; HEART = History, Electrocardiography, Age, Risk factors, and Troponin.
Statistical analysis
Continuous variables were expressed as mean ± standard deviations for normal distribution and compared using the Student’s t-test. Variables with a skewed distribution were expressed as medians with their interquartile range (IQR) and analyzed using the Mann–Whitney test. Categorical variables were calculated as absolute numbers with corresponding percentages and compared using the χ
2 test. Performances of the HEART and modified HEART pathway were compared in terms of sensitivity, specificity, positive predictive value (PPV), NPV, and the rate of low-risk classifications assigned by each method. The area under the receiver-operating characteristics curve (AUC) and the corresponding 95% confidence interval (CI) were examined to compare the HEAR and modified HEAR scores. The nonparametric method described by DeLong et al.
9) was used to compare the AUCs. We also performed a net reclassification analysis, a sum of the score’s ability to increase both the true proportions of high-risk and low-risk patients, to assess the appropriateness of the risk category change.
10) All statistical analyses were performed using IBM SPSS Statistics v 21.0 (IBM Corp., Armonk, NY, USA) and MedCalc
® Statistical Software version 20.111 (MedCalc Software Ltd., Ostend, Belgium;
https://www.medcalc.org; 2022). A p value of <0.05 was considered statistically significant.
RESULTS
From April 2019 to March 2022, 1,304 patients with symptoms suggestive of ACS were enrolled, and both HEART pathway and modified HEART pathway risk assessments were completed. Case selection for enrolled patients is depicted in a flow diagram (
Figure 1). A total of 538 patients with HEAR and 516 with modified HEAR had scores of 0–3. Serial troponins, CAD history, and ECG findings were added for further risk stratification. Finally, 500 (38.3%) patients with HEART pathway and 486 (37.3%) with modified HEART pathway were classified as low-risk. Of the 1,304 enrolled patients, 1252 completed a follow-up of at least one month. For the remaining 52 patients who were discharged from the emergency department, information regarding MACE other than death was not available and they were assumed to have not experienced any adverse outcomes.
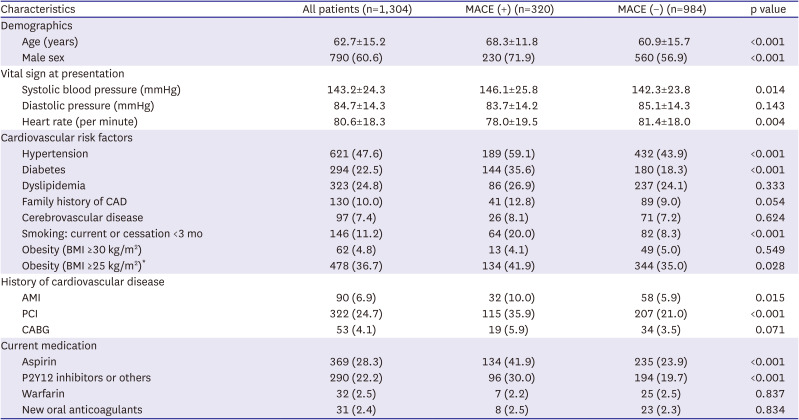
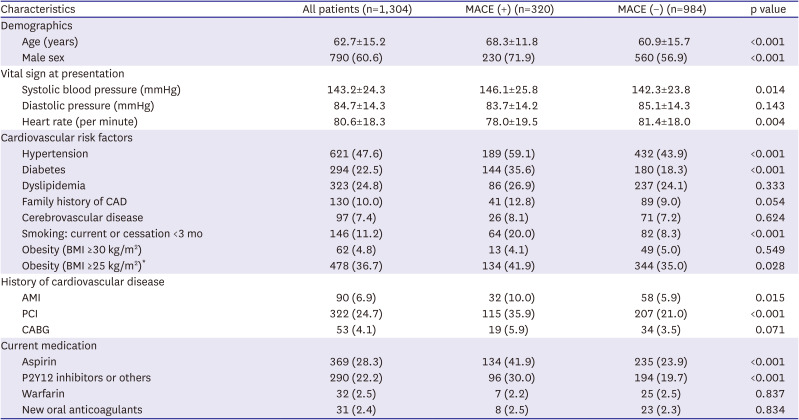
Table 1 summarizes the baseline characteristics of patients. The mean age was 62.7±15.2 years, and 790 (60.6%) were men. MACE at 30 days occurred in 320 (24.5%). In those who experienced MACE, patients were older (68.3±11.8 vs. 60.9±15.7, p<0.001), and men were more common (71.9% vs. 56.9%, p<0.001) compared with those who did not experience MACE. Among the cardiovascular risk factors, hypertension, diabetes, and smoking were also more common (all p<0.001) in patients with MACE. Regarding obesity, the traditional cut-off of BMI ≥30 kg/m
2 did not show a significant difference between the two groups; however, the difference was significant (41.9% vs. 35.0%, p=0.028) when the cut-off of ≥25 kg/m
2 was used.
Table 1
Baseline characteristics of patients
|
Characteristics |
All patients (n=1,304) |
MACE (+) (n=320) |
MACE (−) (n=984) |
p value |
|
Demographics |
|
|
|
|
|
Age (years) |
62.7±15.2 |
68.3±11.8 |
60.9±15.7 |
<0.001 |
|
Male sex |
790 (60.6) |
230 (71.9) |
560 (56.9) |
<0.001 |
|
Vital sign at presentation |
|
|
|
|
|
Systolic blood pressure (mmHg) |
143.2±24.3 |
146.1±25.8 |
142.3±23.8 |
0.014 |
|
Diastolic pressure (mmHg) |
84.7±14.3 |
83.7±14.2 |
85.1±14.3 |
0.143 |
|
Heart rate (per minute) |
80.6±18.3 |
78.0±19.5 |
81.4±18.0 |
0.004 |
|
Cardiovascular risk factors |
|
|
|
|
|
Hypertension |
621 (47.6) |
189 (59.1) |
432 (43.9) |
<0.001 |
|
Diabetes |
294 (22.5) |
144 (35.6) |
180 (18.3) |
<0.001 |
|
Dyslipidemia |
323 (24.8) |
86 (26.9) |
237 (24.1) |
0.333 |
|
Family history of CAD |
130 (10.0) |
41 (12.8) |
89 (9.0) |
0.054 |
|
Cerebrovascular disease |
97 (7.4) |
26 (8.1) |
71 (7.2) |
0.624 |
|
Smoking: current or cessation <3 mo |
146 (11.2) |
64 (20.0) |
82 (8.3) |
<0.001 |
|
Obesity (BMI ≥30 kg/m2) |
62 (4.8) |
13 (4.1) |
49 (5.0) |
0.549 |
|
Obesity (BMI ≥25 kg/m2)*
|
478 (36.7) |
134 (41.9) |
344 (35.0) |
0.028 |
|
History of cardiovascular disease |
|
|
|
|
|
AMI |
90 (6.9) |
32 (10.0) |
58 (5.9) |
0.015 |
|
PCI |
322 (24.7) |
115 (35.9) |
207 (21.0) |
<0.001 |
|
CABG |
53 (4.1) |
19 (5.9) |
34 (3.5) |
0.071 |
|
Current medication |
|
|
|
|
|
Aspirin |
369 (28.3) |
134 (41.9) |
235 (23.9) |
<0.001 |
|
P2Y12 inhibitors or others |
290 (22.2) |
96 (30.0) |
194 (19.7) |
<0.001 |
|
Warfarin |
32 (2.5) |
7 (2.2) |
25 (2.5) |
0.837 |
|
New oral anticoagulants |
31 (2.4) |
8 (2.5) |
23 (2.3) |
0.834 |
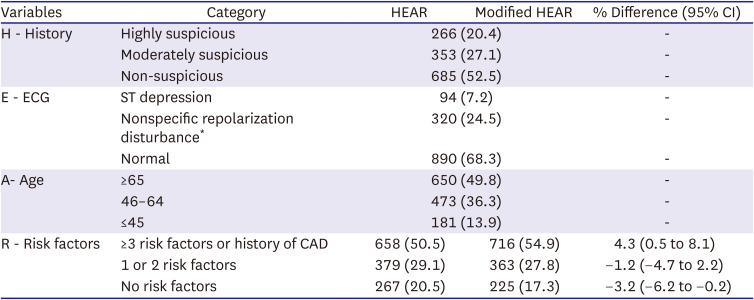
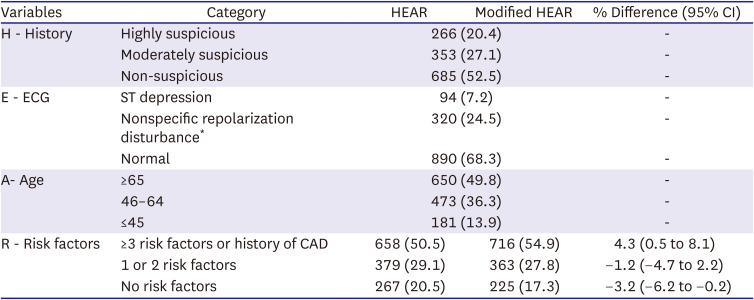
In the R component, patients with no-risk factor (−3.2% [95% CI, −6.2% to −0.2%]), and 1 or 2 risk factors (−1.2% [95% CI, −4.7% to 2.2%]) decreased while those with ≥3 risk factors or history of CAD increased (4.3% [95% CI, 0.5% to 8.1%]) after modification of cut-off for obesity (
Table 2). The change in the number of patients and MACE rates in the low, intermediate, and high-risk groups according to both the HEART score and the modified HEART score are shown in
Supplementary Table 2.
Table 2
Summary of HEAR and modified HEAR
|
Variables |
Category |
HEAR |
Modified HEAR |
% Difference (95% CI) |
|
H - History |
Highly suspicious |
266 (20.4) |
- |
|
Moderately suspicious |
353 (27.1) |
- |
|
Non-suspicious |
685 (52.5) |
- |
|
E - ECG |
ST depression |
94 (7.2) |
- |
|
Nonspecific repolarization disturbance*
|
320 (24.5) |
- |
|
Normal |
890 (68.3) |
- |
|
A- Age |
≥65 |
650 (49.8) |
- |
|
46–64 |
473 (36.3) |
- |
|
≤45 |
181 (13.9) |
- |
|
R - Risk factors |
≥3 risk factors or history of CAD |
658 (50.5) |
716 (54.9) |
4.3 (0.5 to 8.1) |
|
1 or 2 risk factors |
379 (29.1) |
363 (27.8) |
−1.2 (−4.7 to 2.2) |
|
No risk factors |
267 (20.5) |
225 (17.3) |
−3.2 (−6.2 to −0.2) |
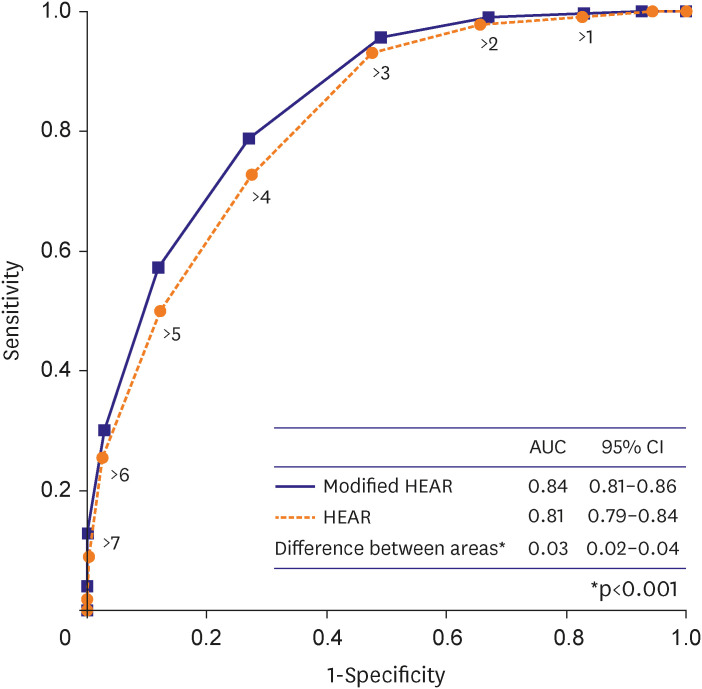
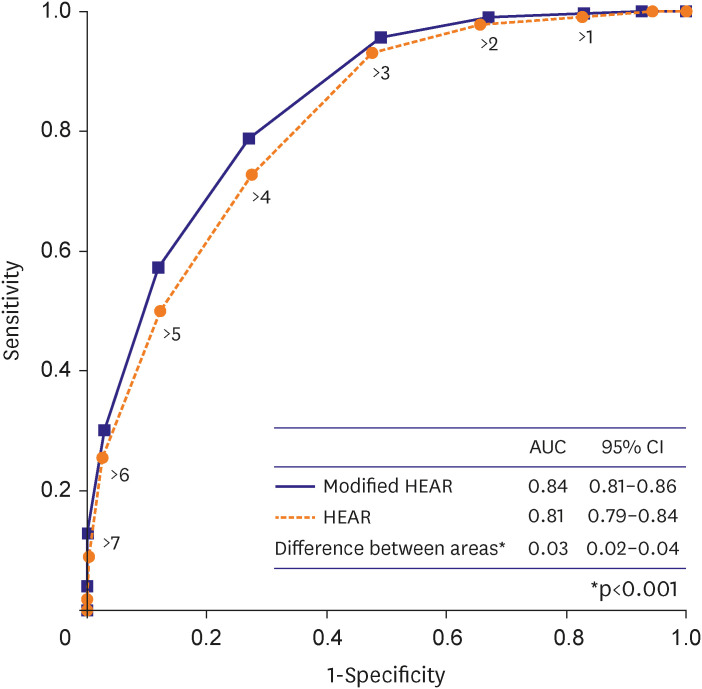
The AUC of the modified HEAR score for 30-day MACE was higher than that of HEAR score (0.84 [95% CI, 0.81 to 0.86] vs. 0.81 [95% CI, 0.79 to 0.84], p<0.001) (
Figure 2). A pairwise comparison was conducted to evaluate the improvement in reclassification of the risk category achieved by the modified HEART pathway compared to the original HEART pathway. The results of the net reclassification analysis indicated that the modified HEART pathway provided an improvement (net reclassification improvement of 0.24%, as shown in
Supplementary Table 3).
Figure 2
The area under the receiver operating characteristic curves for HEAR and modified HEAR score.
AUC = area under the receiver operating characteristic curve; CI = confidence interval; HEAR = History, Electrocardiography, Age, and Risk factors.
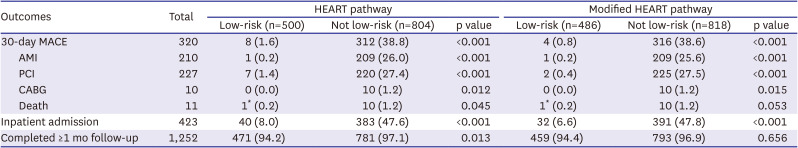
Of the 500 patients classified as low-risk using the HEART pathway, 8 patients (1.6% [95% CI, 0.7% to 3.2%]; 1 AMI, 7 PCI, and 1 death) experienced MACE, and of the 486 low-risk patients with modified HEART pathway, 4 patients (0.8% [95% CI, 0.2% to 2.1%]; 1 AMI, 2 PCI, and 1 death) experienced MACE (
Table 3). Of the low-risk patients classified by HEART and modified HEART pathway, 40 (8%) and 32 (6.6%) were admitted to inpatient unit, respectively. Final diagnosis of those hospitalized are described in
Supplementary Table 4.
Table 3
Outcome frequencies of low-risk patients according to the HEART and modified HEART pathway
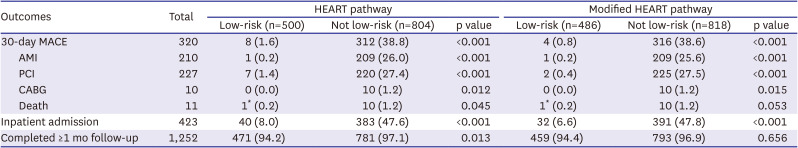
|
Outcomes |
Total |
HEART pathway |
Modified HEART pathway |
|
Low-risk (n=500) |
Not low-risk (n=804) |
p value |
Low-risk (n=486) |
Not low-risk (n=818) |
p value |
|
30-day MACE |
320 |
8 (1.6) |
312 (38.8) |
<0.001 |
4 (0.8) |
316 (38.6) |
<0.001 |
|
AMI |
210 |
1 (0.2) |
209 (26.0) |
<0.001 |
1 (0.2) |
209 (25.6) |
<0.001 |
|
PCI |
227 |
7 (1.4) |
220 (27.4) |
<0.001 |
2 (0.4) |
225 (27.5) |
<0.001 |
|
CABG |
10 |
0 (0.0) |
10 (1.2) |
0.012 |
0 (0.0) |
10 (1.2) |
0.015 |
|
Death |
11 |
1* (0.2) |
10 (1.2) |
0.045 |
1* (0.2) |
10 (1.2) |
0.053 |
|
Inpatient admission |
423 |
40 (8.0) |
383 (47.6) |
<0.001 |
32 (6.6) |
391 (47.8) |
<0.001 |
|
Completed ≥1 mo follow-up |
1,252 |
471 (94.2) |
781 (97.1) |
0.013 |
459 (94.4) |
793 (96.9) |
0.656 |
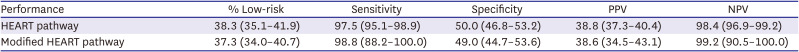
The performance characteristics for HEART and modified HEART pathway for 30-day MACE are summarized in
Tables 4 and
5. The modified HEART pathway identified 37.3% (486/1,304; 95% CI, 34.0% to 40.7%) of patients as low-risk compared with 38.3% (500/1,304; 95% CI, 35.7% to 41.0%) of the HEART pathway (p=0.746). The modified HEART pathway had a sensitivity of 98.8% (95% CI, 88.2% to 100.0%), a NPV of 99.2% (95% CI, 90.5% to 100.0%), a specificity of 49.0% (95% CI, 44.7% to 53.6%), and a PPV of 38.6% (95% CI, 34.5% to 43.1%), compared with a sensitivity of 97.5% (95% CI, 95.1% to 98.9%), a NPV of 98.4% (95% CI, 96.9% to 99.2%), a specificity of 50.0% (95% CI, 46.8% to 53.2%), and a PPV of 38.8% (95% CI, 37.3% to 40.4%) of the HEART pathway.
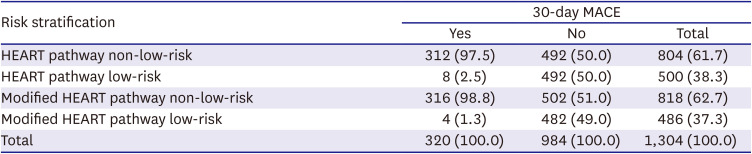
Table 4
Risk stratification of the HEART and modified HEART pathway for 30-day MACE
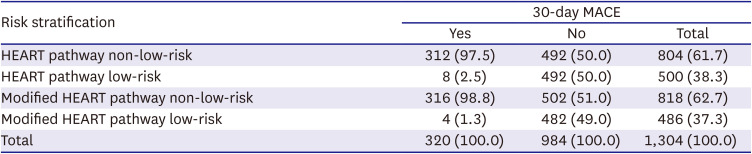
|
Risk stratification |
30-day MACE |
|
Yes |
No |
Total |
|
HEART pathway non-low-risk |
312 (97.5) |
492 (50.0) |
804 (61.7) |
|
HEART pathway low-risk |
8 (2.5) |
492 (50.0) |
500 (38.3) |
|
Modified HEART pathway non-low-risk |
316 (98.8) |
502 (51.0) |
818 (62.7) |
|
Modified HEART pathway low-risk |
4 (1.3) |
482 (49.0) |
486 (37.3) |
|
Total |
320 (100.0) |
984 (100.0) |
1,304 (100.0) |
Table 5
Performance characteristics of the HEART and modified HEART pathway for 30-day MACE
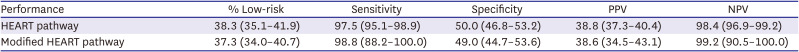
|
Performance |
% Low-risk |
Sensitivity |
Specificity |
PPV |
NPV |
|
HEART pathway |
38.3 (35.1–41.9) |
97.5 (95.1–98.9) |
50.0 (46.8–53.2) |
38.8 (37.3–40.4) |
98.4 (96.9–99.2) |
|
Modified HEART pathway |
37.3 (34.0–40.7) |
98.8 (88.2–100.0) |
49.0 (44.7–53.6) |
38.6 (34.5–43.1) |
99.2 (90.5–100.0) |
DISCUSSION
To the best of our knowledge, this was the first study to modify and validate the HEART pathway for predicting MACE in Korean population. The key finding of our study is that low-risk patients for MACE can be identified in patients evaluated for possible ACS by applying the HEART pathway as follows: adding serial hsTnI, history of CAD, and ECG findings to HEAR score ≤3. There were 500/1,304 (38.3%) low-risk patients with a 30-day MACE of 1.6% in our study population. More notable findings were that when applying the modified HEART pathway, the proportion of low-risk patients decreased to 486/1,304 (37.3%), and their 30-day MACE was 0.8%. While the HEART pathway identified more patients as low-risk, less patients with a low risk experienced MACE with the modified HEART pathway. Since a 2% pretest probability threshold is suggested for determining whether objective cardiac testing is required
11) and emergency physicians’ acceptable risk of MACE is <1% for patients discharged from ED,
12) the low-risk cohort of patients classified using the modified HEART pathway could be discharged from ED without further testing.
Obesity and related metabolic disorders have been deemed significant risk factors for cardiovascular diseases globally, including in East Asia.
13) Racial and ethnic differences exist in the prevalence of obesity and the risk for obesity-related illnesses. Asian populations typically have a different percentage of body fat related to BMI and have a higher risk for cardiovascular disease than Caucasians with the same BMI. Over two decades have passed since the WHO released additional BMI cut-off points for obesity for Asians.
6) Therefore, BMI criteria tailored for different ethnic groups could be used to measure the risk of obesity more accurately. However, this difference could highlight the difficulty in generalizing the results of risk stratification studies conducted in different ethnic groups. Moreover, information related to obesity is not accurate; most published studies do not consider different cut-offs between different ethnic groups. Even those performed in the Asian countries still adhere to recommended criteria for Caucasian populations. Furthermore, because BMI is not routinely calculated in many EDs, obesity was not considered one of the risk factors in several retrospective studies.
14)15) Our study modified the R component using the BMI cut-off suggested for Korean and compared the performance between original and modified HEAR scores. By doing so, the proportion of no risk factors was decreased, and ≥3 risk factors increased significantly.
Recent guidelines suggest that patients with <1% risk for 30-day MACE should be designated as low-risk, and it is reasonable to discharge them home without admission or urgent cardiac testing.
16) ADPs, such as the HEART pathway, have a dual purpose of identifying at-risk patients while minimizing unnecessary studies and inpatient admission. This study shows that the modified HEART pathway for Korean population could identify patients safe for early discharge more accurately (sensitivity 98.8%, and NPV 99.2%) than the HEART pathway (sensitivity 97.5%, and NPV 98.4%). An increase in R component through the modification contributed to an increase in total score count, which enabled more accurate detection of low-risk patients for MACE.
Several studies were conducted to validate the HEART pathway. Oliver et al.,
17) after implementing the outpatient disposition strategy using the HEART pathway, analyzed 449 patients presenting to ED. While 36.5% were considered low-risk and discharged for outpatient assessment, no one experienced MACE, showing a sensitivity of 100%. Stopyra et al.
15) analyzed 4,399 ED patients; 38.4% were considered low-risk from the HEART pathway, and 0.4% of low-risk patients had MACE. Mahler et al.
14) performed a randomized trial comparing the HEART pathway vs. usual care. Among 141 patients allocated to the HEART pathway, 46.8% were considered low-risk, and no one experienced MACE. The results from our study were comparable to these studies, with a high sensitivity of 98.8%, and similar proportions of patients were classified into the low-risk group. However, even with the modified HEART pathway in our study, 4 out of 486 (0.8%) experienced MACE. This was lower than 1% but still high compared to the above studies. This was probably related to more patients with higher severity being included in our study when considering the overall MACE of our cohort (24.5%) being higher than those of others (Oliver 5.6%, Stopyra 10.2%, and Mahler 6%). Even though patients had higher severity, showing sensitivity and NPV of 98.8% and 99.2%, respectively, could be translated as proof of the promising role of the modified HEART pathway in patients with chest pain.
This study has several limitations. This study was conducted at a single academic medical center ED with a background and ethnicity different from previous ones, which might limit its generalizability; the patients cannot be representative of the generalized population, implying that the obtained results should be interpreted considering the health care system. Comorbidities were established by patient self-reporting and were not corroborated through other objective means. Regarding serial troponin measurement, our institutional practice is a 2-hour interval follow-up rather than 3 hours chosen in most HEART pathways. Since we use high-sensitive troponin rather than contemporary ones, we thought this interval would not affect the performance of ADPs. However, as longer intervals could yield more positive results of troponin in the presence of myocardial injury, theoretically, our 2-hour interval could have influenced test results and, eventually, interpretation of the risk category in the pathway. Given that the most known MACE occurred during the index visit, the likelihood of MACE occurring right after discharge and not describing this issue during a follow-up visit, such as recurrent chest pain after discharge, appears low but possible. Additionally, it is possible that patients who did not complete at least one month of follow-up might have unconfirmed adverse outcomes, leading to misclassification. Some diseases not included in the definition of MACE could also be considered adverse events, although they are rarer than CAD and most of them were classified as not low-risk by the risk stratification tool (
Supplementary Table 4).
In conclusion, the modified HEART pathway for the Korean population, using the BMI cut-off levels suggested for Koreans, could help identify patients safe for early discharge more accurately. While the HEART pathway identified more patients as low-risk, fewer patients in the low-risk category experienced MACE with the modified HEART pathway.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download