1. Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010; 362:886–895. PMID:
20220183.

2. Jespersen L, Hvelplund A, Abildstrøm SZ, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012; 33:734–744. PMID:
21911339.

3. Feenstra RG, Boerhout CK, Woudstra J, et al. Presence of coronary endothelial dysfunction, coronary vasospasm, and adenosine-mediated vasodilatory disorders in patients with ischemia and nonobstructive coronary arteries. Circ Cardiovasc Interv. 2022; 15:e012017. PMID:
35904014.

4. Ford TJ, Stanley B, Good R, et al. Stratified medical therapy using invasive coronary function testing in angina: the CorMicA trial. J Am Coll Cardiol. 2018; 72:2841–2855. PMID:
30266608.

5. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI expert consensus document on ischaemia with non-obstructive coronary arteries in collaboration with European Society of Cardiology working group on coronary pathophysiology & microcirculation endorsed by coronary vasomotor disorders international. EuroIntervention. 2021; 16:1049–1069. PMID:
32624456.

6. Crea F, Camici PG, De Caterina R, Lanza GA. 17. Chronic ischaemic heart disease. Camm AJ, Lüscher TF, Serruys PW, editors. The ESC Textbook of Cardiovascular Medicine. 2nd ed. Oxford: Oxford University Press;2006.
7. Mosher P, Ross J Jr, McFate PA, Shaw RF. Control of coronary blood flow by an autoregulatory mechanism. Circ Res. 1964; 14:250–259. PMID:
14133952.

8. Deussen A, Ohanyan V, Jannasch A, Yin L, Chilian W. Mechanisms of metabolic coronary flow regulation. J Mol Cell Cardiol. 2012; 52:794–801. PMID:
22004900.

9. Chilian WM. Coronary microcirculation in health and disease. Summary of an NHLBI workshop. Circulation. 1997; 95:522–528. PMID:
9008472.
10. Kelm M, Schrader J. Control of coronary vascular tone by nitric oxide. Circ Res. 1990; 66:1561–1575. PMID:
2160870.

11. Layland J, Carrick D, Lee M, Oldroyd K, Berry C. Adenosine: physiology, pharmacology, and clinical applications. JACC Cardiovasc Interv. 2014; 7:581–591. PMID:
24835328.
12. Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur Heart J. 2014; 35:1101–1111. PMID:
24366916.

13. Rahman H, Demir OM, Khan F, et al. Physiological stratification of patients with angina due to coronary microvascular dysfunction. J Am Coll Cardiol. 2020; 75:2538–2549. PMID:
32439003.

14. Rahman H, Ryan M, Lumley M, et al. Coronary microvascular dysfunction is associated with myocardial ischemia and abnormal coronary perfusion during exercise. Circulation. 2019; 140:1805–1816. PMID:
31707835.

15. Boerhout CKM, de Waard GA, Lee JM, et al. Prognostic value of structural and functional coronary microvascular dysfunction in patients with non-obstructive coronary artery disease; from the multicentre international ILIAS registry. EuroIntervention. 2022; 18:719–728. PMID:
35694826.

16. van de Hoef TP, Bax M, Damman P, et al. Impaired coronary autoregulation is associated with long-term fatal events in patients with stable coronary artery disease. Circ Cardiovasc Interv. 2013; 6:329–335. PMID:
23899871.

17. Zeiher AM, Drexler H, Wollschläger H, Just H. Endothelial dysfunction of the coronary microvasculature is associated with coronary blood flow regulation in patients with early atherosclerosis. Circulation. 1991; 84:1984–1992. PMID:
1934373.

18. Suwaidi JA, Hamasaki S, Higano ST, Nishimura RA, Holmes DR Jr, Lerman A. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation. 2000; 101:948–954. PMID:
10704159.

19. Beltrame JF, Crea F, Kaski JC, et al. International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017; 38:2565–2568. PMID:
26245334.

20. Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation. 2011; 124:1774–1782. PMID:
22007100.

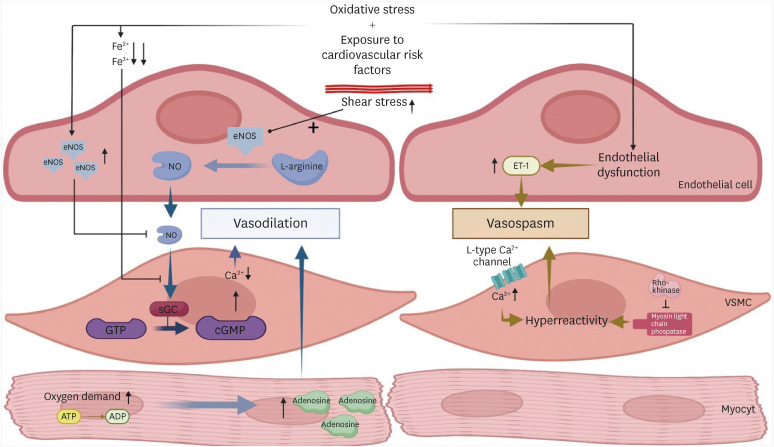
21. Hubert A, Seitz A, Pereyra VM, et al. Coronary artery spasm: the interplay between endothelial dysfunction and vascular smooth muscle cell hyperreactivity. Eur Cardiol. 2020; 15:e12. PMID:
32373185.

22. Kuga T, Shimokawa H, Hirakawa Y, et al. Increased expression of L-type calcium channels in vascular smooth muscle cells at spastic site in a porcine model of coronary artery spasm. J Cardiovasc Pharmacol. 2000; 35:822–828. PMID:
10813387.

23. Kandabashi T, Shimokawa H, Miyata K, et al. Inhibition of myosin phosphatase by upregulated rho-kinase plays a key role for coronary artery spasm in a porcine model with interleukin-1β. Circulation. 2000; 101:1319–1323. PMID:
10725293.

24. Konst RE, Meeder JG, Wittekoek ME, et al. Ischaemia with no obstructive coronary arteries. Neth Heart J. 2020; 28:66–72. PMID:
32780334.

25. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008; 51:2–17. PMID:
18522770.

26. Pepine CJ, Anderson RD, Sharaf BL, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the National Heart, Lung and Blood Institute WISE (Women’s Ischemia Syndrome Evaluation) study. J Am Coll Cardiol. 2010; 55:2825–2832. PMID:
20579539.

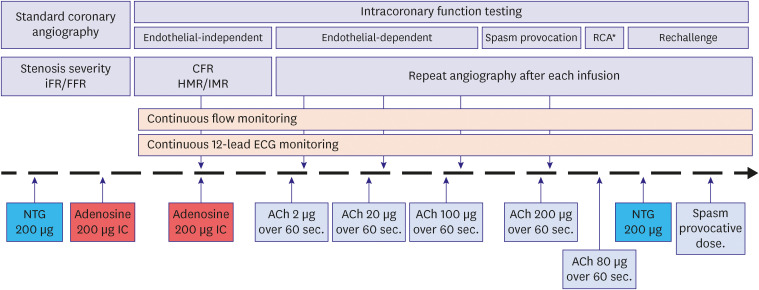
27. Feenstra R, Seitz A, Boerhout C, et al. Principles and pitfalls in coronary vasomotor function testing. EuroIntervention. 2022; 17:1271–1280. PMID:
34278990.

28. Hackett D, Larkin S, Chierchia S, Davies G, Kaski JC, Maseri A. Induction of coronary artery spasm by a direct local action of ergonovine. Circulation. 1987; 75:577–582. PMID:
3815770.

29. Sueda S, Kohno H, Ochi T, Uraoka T, Tsunemitsu K. Overview of the pharmacological spasm provocation test: comparisons between acetylcholine and ergonovine. J Cardiol. 2017; 69:57–65. PMID:
27856130.

30. JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2013). Circ J. 2014; 78:2779–2801. PMID:
25273915.
31. Seitz A, Feenstra R, Konst RE, et al. Acetylcholine rechallenge: a first step toward tailored treatment in patients with coronary artery spasm. JACC Cardiovasc Interv. 2022; 15:65–75. PMID:
34991826.
32. Gallinoro E, Candreva A, Colaiori I, et al. Thermodilution-derived volumetric resting coronary blood flow measurement in humans. EuroIntervention. 2021; 17:e672–e679. PMID:
33528358.

33. Camici PG, d’Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015; 12:48–62. PMID:
25311229.

34. Demir OM, Boerhout CK, de Waard GA, et al. Comparison of Doppler flow velocity and thermodilution derived indexes of coronary physiology. JACC Cardiovasc Interv. 2022; 15:1060–1070. PMID:
35589236.

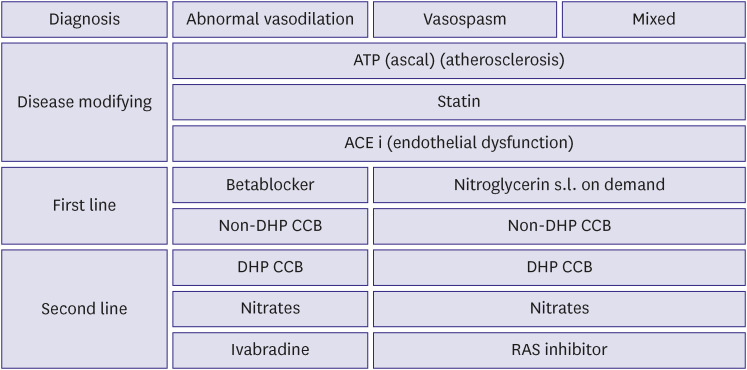
35. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020; 41:407–477. PMID:
31504439.
36. Boerhout CK, Feenstra RG, Somsen GA, et al. Coronary computed tomographic angiography as gatekeeper for new-onset stable angina. Neth Heart J. 2021; 29:551–556. PMID:
34676522.

37. Cha MJ, Kim WD, Won H, et al. Nationwide trends of gatekeeper to invasive coronary angiography in suspected coronary artery disease. Korean Circ J. 2022; 52:814–825. PMID:
36217588.

38. Dai N, Hwang D, Lee JM, et al. Association of quantitative flow ratio with lesion severity and its ability to discriminate myocardial ischemia. Korean Circ J. 2021; 51:126–139. PMID:
33525067.

39. Jansen TP, Konst RE, de Vos A, et al. Efficacy of diltiazem to improve coronary vasomotor dysfunction in ANOCA: the EDIT-CMD randomized clinical trial. JACC Cardiovasc Imaging. 2022; 15:1473–1484. PMID:
35466050.

40. de Waure C, Lauret GJ, Ricciardi W, et al. Lifestyle interventions in patients with coronary heart disease: a systematic review. Am J Prev Med. 2013; 45:207–216. PMID:
23867029.
41. Shahin Y, Khan JA, Samuel N, Chetter I. Angiotensin converting enzyme inhibitors effect on endothelial dysfunction: a meta-analysis of randomised controlled trials. Atherosclerosis. 2011; 216:7–16. PMID:
21411098.

42. Keller KB, Lemberg L. Prinzmetal’s angina. Am J Crit Care. 2004; 13:350–354. PMID:
15293589.

43. Nishigaki K, Inoue Y, Yamanouchi Y, et al. Prognostic effects of calcium channel blockers in patients with vasospastic angina--a meta-analysis. Circ J. 2010; 74:1943–1950. PMID:
20668353.

44. Cattaneo M, Porretta AP, Gallino A. Ranolazine: Drug overview and possible role in primary microvascular angina management. Int J Cardiol. 2015; 181:376–381. PMID:
25555283.

45. Leonardo F, Fragasso G, Rossetti E, et al. Comparison of trimetazidine with atenolol in patients with syndrome X: effects on diastolic function and exercise tolerance. Cardiologia. 1999; 44:1065–1069. PMID:
10687257.
46. Jia Q, Shi S, Yuan G, et al. The effect of nicorandil in patients with cardiac syndrome X: a meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020; 99:e22167. PMID:
32925783.
47. Crooijmans C, Jansen TP, Konst RE, et al. for NL-CFT. Design and rationale of the NetherLands registry of invasive Coronary vasomotor Function Testing (NL-CFT). Int J Cardiol. 2023; 379:1–8. PMID:
36863419.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download