Children have generally experienced a relatively mild clinical manifestation of coronavirus disease 2019 (COVID-19) since the early phase of the pandemic. During delta and omicron variant circulation, the number of pediatric patients with COVID-19 greatly increased; subsequently, severe pediatric cases also increased.
12 Severe COVID-19 requires intensive care, ventilator or hemodynamic support, and can result in organ system complications or death.
3 Although the overall infection fatality rate of COVID-19 is low for children, most deaths have been reported in pediatric patients with comorbidities.
45
Several studies have explored the risk factors for severe pediatric COVID-19, and disease categories such as immunocompromised condition, cardiovascular disease, chronic lung disease, neurologic disease, diabetes, and obesity have been reported as pediatric high-risk comorbidities.
67 Because immunization with COVID-19 vaccines prevents progression to severe disease, children with high-risk comorbidities are a priority for COVID-19 vaccination in many countries, including Korea.
The Korea Disease Control and Prevention Agency (KDCA) recommended COVD-19 vaccination in pediatric patients with high-risk diseases including chronic lung disease, chronic heart disease, chronic liver disease, chronic kidney disease, neuro-muscular disease, diabetes mellitus, obesity, and immunocompromised condition.
8 KDCA recommended vaccination for all 12–17-year-old adolescents in mid-October 2021, while for high-risk 5–11-year-olds in late March 2022 at the middle of Omicron surge. Vaccination in healthy children of 5–11 years was left to parental choice. Third-shot and bivalent vaccine were recommended to high-risk 12–17-year-olds in mid-March 2022 and December 2022, respectively.
COVID-19 vaccination policies for children 5–11 years were differed by country, which were compared among four countries (United States, United Kingdome, Japan, and Korea) along with national vaccination rates in
Supplementary Table 1. The vaccination was implemented about one month before the omicron predominance in the US (early November 2021), one month after omicron in the UK (end of January 2022), and two months after omicron in Japan (end of February 2022) and Korea (end of March 2022). It was recommended in all children 5–11 years in the US, while it was recommended in high-risk group in the UK, Japan, and Korea. Of note, Japan expanded the recommendation to all children after six months, concerning for the low vaccination rate of 18.5% at the time.
9 As a result, in Korea, the two-dose vaccination rate for 5–11-year-olds remained at the lowest 1.1% as of January 2023 despite 10 months of implementation, compared to 19.1% in Japan after 11 months and 29.7% in the U.S. after 10 months.
101112 Meanwhile, among the US pediatric population, Asian children had the highest vaccination rate: 57.1% compared with 29.0% of white children.
12
In this study, we summarized overall COVID-19 vaccination status as of July 2022, in the Korean pediatric population (5–17 years) with comorbidities in addition to high-risk diseases for whom KDCA recommended COVID-19 vaccination and compared it to that of the general population in the same age group using the National Health Insurance Service database.
For comorbidity classification, a list of International Classification of Diseases and Related Health Problems, 10th Edition codes for systemic chronic diseases was created (
Supplementary Table 2). Diseases with a known risk for severe COVID-19 were included, and acute infection codes were excluded. Accordingly, 12 organ-specific comorbidity categories encompassing 45 individual diseases were identified.
Pediatric patients with chronic disease who had a history of at least three outpatient clinic visits or at least one hospitalization were identified from April 2021 to March 2022. Vaccination history in the patient population aged 5–17 years through July 2022 was analyzed. The population was divided into two groups: a 5–11 years age group and a 12–17 years age group. Vaccination rate data for the total pediatric populations of both age groups as of July 28, 2022, were collected from a KDCA press release.
13 For statistical analysis, binomial distribution was used to evaluate whether significant difference in vaccination rate exists between the specific diseases or comorbidity categories with total population.
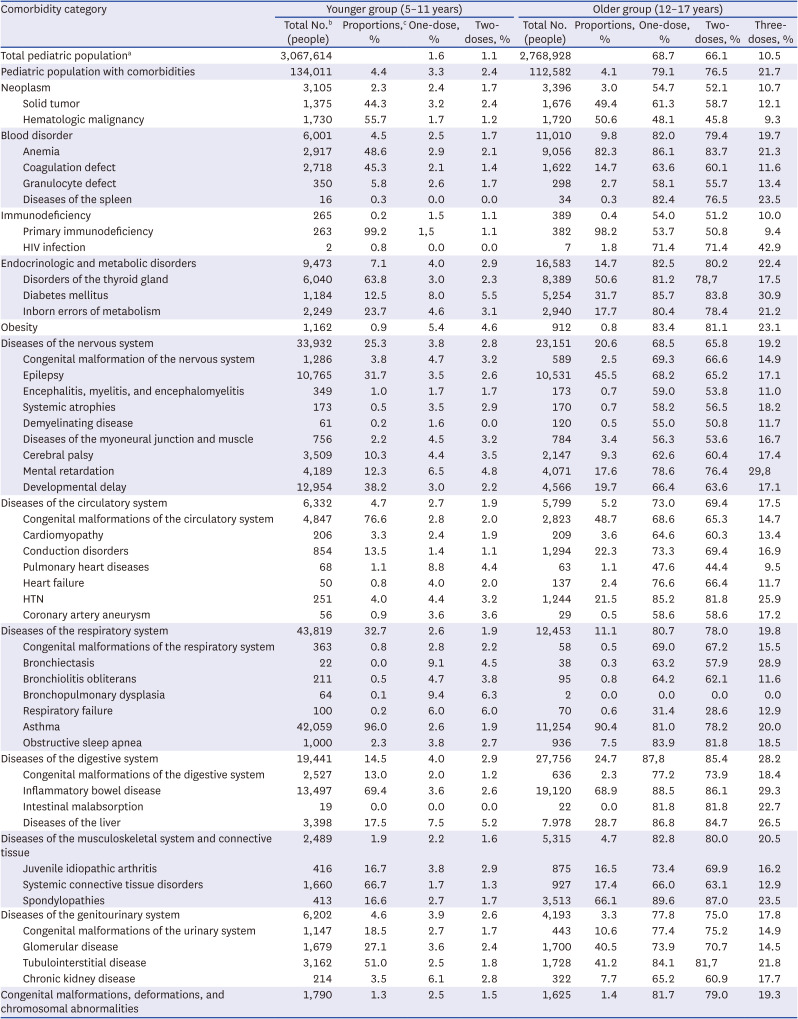
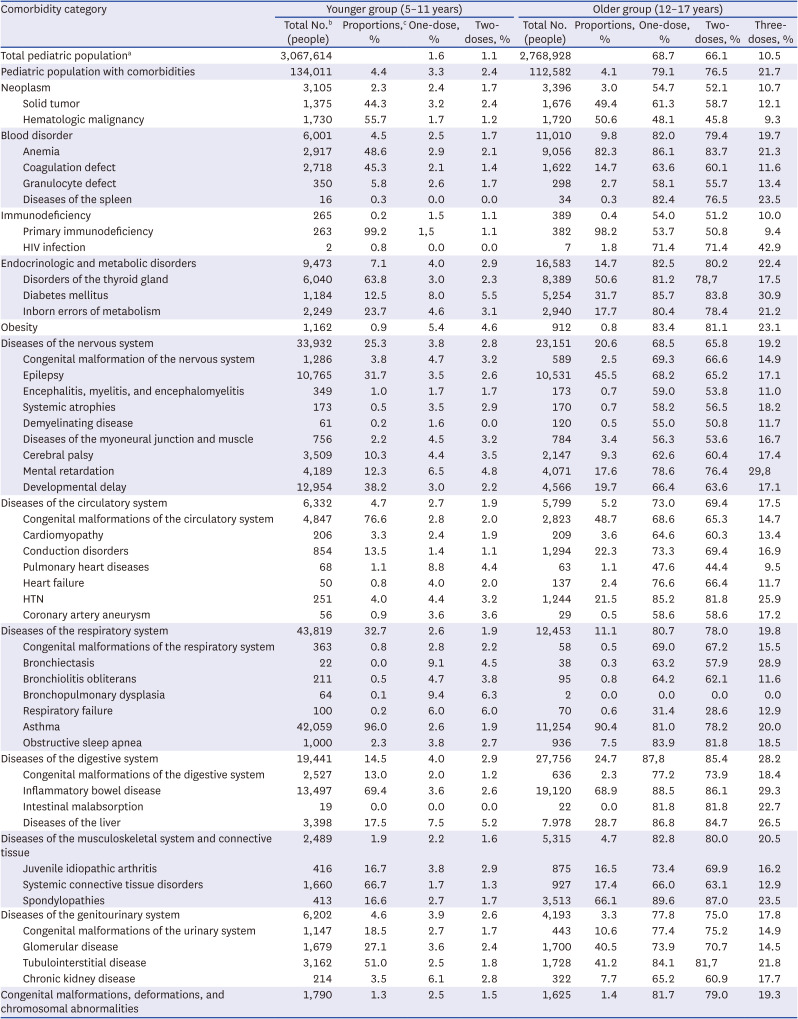
A total of 246,593 children was identified with comorbidities, which accounted for 4.2% of the total pediatric population (N = 5,836,542) in the 5–17-year age group in Korea. Detailed data on the proportions of comorbidity categories in each age group are summarized in
Table 1.
Table 1
COVID-19 vaccination rates among the pediatric population with comorbidities as of July 31, 2022
|
Comorbidity category |
Younger group (5–11 years) |
Older group (12–17 years) |
|
Total No.b (people) |
Proportions,c % |
One-dose, % |
Two-doses, % |
Total No. (people) |
Proportions, % |
One-dose, % |
Two-doses, % |
Three-doses, % |
|
Total pediatric populationa
|
3,067,614 |
|
1.6 |
1.1 |
2,768,928 |
|
68.7 |
66.1 |
10.5 |
|
Pediatric population with comorbidities |
134,011 |
4.4 |
3.3 |
2.4 |
112,582 |
4.1 |
79.1 |
76.5 |
21.7 |
|
Neoplasm |
3,105 |
2.3 |
2.4 |
1.7 |
3,396 |
3.0 |
54.7 |
52.1 |
10.7 |
|
Solid tumor |
1,375 |
44.3 |
3.2 |
2.4 |
1,676 |
49.4 |
61.3 |
58.7 |
12.1 |
|
Hematologic malignancy |
1,730 |
55.7 |
1.7 |
1.2 |
1,720 |
50.6 |
48.1 |
45.8 |
9.3 |
|
Blood disorder |
6,001 |
4.5 |
2.5 |
1.7 |
11,010 |
9.8 |
82.0 |
79.4 |
19.7 |
|
Anemia |
2,917 |
48.6 |
2.9 |
2.1 |
9,056 |
82.3 |
86.1 |
83.7 |
21.3 |
|
Coagulation defect |
2,718 |
45.3 |
2.1 |
1.4 |
1,622 |
14.7 |
63.6 |
60.1 |
11.6 |
|
Granulocyte defect |
350 |
5.8 |
2.6 |
1.7 |
298 |
2.7 |
58.1 |
55.7 |
13.4 |
|
Diseases of the spleen |
16 |
0.3 |
0.0 |
0.0 |
34 |
0.3 |
82.4 |
76.5 |
23.5 |
|
Immunodeficiency |
265 |
0.2 |
1.5 |
1.1 |
389 |
0.4 |
54.0 |
51.2 |
10.0 |
|
Primary immunodeficiency |
263 |
99.2 |
1,5 |
1.1 |
382 |
98.2 |
53.7 |
50.8 |
9.4 |
|
HIV infection |
2 |
0.8 |
0.0 |
0.0 |
7 |
1.8 |
71.4 |
71.4 |
42.9 |
|
Endocrinologic and metabolic disorders |
9,473 |
7.1 |
4.0 |
2.9 |
16,583 |
14.7 |
82.5 |
80.2 |
22.4 |
|
Disorders of the thyroid gland |
6,040 |
63.8 |
3.0 |
2.3 |
8,389 |
50.6 |
81.2 |
78,7 |
17.5 |
|
Diabetes mellitus |
1,184 |
12.5 |
8.0 |
5.5 |
5,254 |
31.7 |
85.7 |
83.8 |
30.9 |
|
Inborn errors of metabolism |
2,249 |
23.7 |
4.6 |
3.1 |
2,940 |
17.7 |
80.4 |
78.4 |
21.2 |
|
Obesity |
1,162 |
0.9 |
5.4 |
4.6 |
912 |
0.8 |
83.4 |
81.1 |
23.1 |
|
Diseases of the nervous system |
33,932 |
25.3 |
3.8 |
2.8 |
23,151 |
20.6 |
68.5 |
65.8 |
19.2 |
|
Congenital malformation of the nervous system |
1,286 |
3.8 |
4.7 |
3.2 |
589 |
2.5 |
69.3 |
66.6 |
14.9 |
|
Epilepsy |
10,765 |
31.7 |
3.5 |
2.6 |
10,531 |
45.5 |
68.2 |
65.2 |
17.1 |
|
Encephalitis, myelitis, and encephalomyelitis |
349 |
1.0 |
1.7 |
1.7 |
173 |
0.7 |
59.0 |
53.8 |
11.0 |
|
Systemic atrophies |
173 |
0.5 |
3.5 |
2.9 |
170 |
0.7 |
58.2 |
56.5 |
18.2 |
|
Demyelinating disease |
61 |
0.2 |
1.6 |
0.0 |
120 |
0.5 |
55.0 |
50.8 |
11.7 |
|
Diseases of the myoneural junction and muscle |
756 |
2.2 |
4.5 |
3.2 |
784 |
3.4 |
56.3 |
53.6 |
16.7 |
|
Cerebral palsy |
3,509 |
10.3 |
4.4 |
3.5 |
2,147 |
9.3 |
62.6 |
60.4 |
17.4 |
|
Mental retardation |
4,189 |
12.3 |
6.5 |
4.8 |
4,071 |
17.6 |
78.6 |
76.4 |
29,8 |
|
Developmental delay |
12,954 |
38.2 |
3.0 |
2.2 |
4,566 |
19.7 |
66.4 |
63.6 |
17.1 |
|
Diseases of the circulatory system |
6,332 |
4.7 |
2.7 |
1.9 |
5,799 |
5.2 |
73.0 |
69.4 |
17.5 |
|
Congenital malformations of the circulatory system |
4,847 |
76.6 |
2.8 |
2.0 |
2,823 |
48.7 |
68.6 |
65.3 |
14.7 |
|
Cardiomyopathy |
206 |
3.3 |
2.4 |
1.9 |
209 |
3.6 |
64.6 |
60.3 |
13.4 |
|
Conduction disorders |
854 |
13.5 |
1.4 |
1.1 |
1,294 |
22.3 |
73.3 |
69.4 |
16.9 |
|
Pulmonary heart diseases |
68 |
1.1 |
8.8 |
4.4 |
63 |
1.1 |
47.6 |
44.4 |
9.5 |
|
Heart failure |
50 |
0.8 |
4.0 |
2.0 |
137 |
2.4 |
76.6 |
66.4 |
11.7 |
|
HTN |
251 |
4.0 |
4.4 |
3.2 |
1,244 |
21.5 |
85.2 |
81.8 |
25.9 |
|
Coronary artery aneurysm |
56 |
0.9 |
3.6 |
3.6 |
29 |
0.5 |
58.6 |
58.6 |
17.2 |
|
Diseases of the respiratory system |
43,819 |
32.7 |
2.6 |
1.9 |
12,453 |
11.1 |
80.7 |
78.0 |
19.8 |
|
Congenital malformations of the respiratory system |
363 |
0.8 |
2.8 |
2.2 |
58 |
0.5 |
69.0 |
67.2 |
15.5 |
|
Bronchiectasis |
22 |
0.0 |
9.1 |
4.5 |
38 |
0.3 |
63.2 |
57.9 |
28.9 |
|
Bronchiolitis obliterans |
211 |
0.5 |
4.7 |
3.8 |
95 |
0.8 |
64.2 |
62.1 |
11.6 |
|
Bronchopulmonary dysplasia |
64 |
0.1 |
9.4 |
6.3 |
2 |
0.0 |
0.0 |
0.0 |
0.0 |
|
Respiratory failure |
100 |
0.2 |
6.0 |
6.0 |
70 |
0.6 |
31.4 |
28.6 |
12.9 |
|
Asthma |
42,059 |
96.0 |
2.6 |
1.9 |
11,254 |
90.4 |
81.0 |
78.2 |
20.0 |
|
Obstructive sleep apnea |
1,000 |
2.3 |
3.8 |
2.7 |
936 |
7.5 |
83.9 |
81.8 |
18.5 |
|
Diseases of the digestive system |
19,441 |
14.5 |
4.0 |
2.9 |
27,756 |
24.7 |
87,8 |
85.4 |
28.2 |
|
Congenital malformations of the digestive system |
2,527 |
13.0 |
2.0 |
1.2 |
636 |
2.3 |
77.2 |
73.9 |
18.4 |
|
Inflammatory bowel disease |
13,497 |
69.4 |
3.6 |
2.6 |
19,120 |
68.9 |
88.5 |
86.1 |
29.3 |
|
Intestinal malabsorption |
19 |
0.0 |
0.0 |
0.0 |
22 |
0.0 |
81.8 |
81.8 |
22.7 |
|
Diseases of the liver |
3,398 |
17.5 |
7.5 |
5.2 |
7.978 |
28.7 |
86.8 |
84.7 |
26.5 |
|
Diseases of the musculoskeletal system and connective tissue |
2,489 |
1.9 |
2.2 |
1.6 |
5,315 |
4.7 |
82.8 |
80.0 |
20.5 |
|
Juvenile idiopathic arthritis |
416 |
16.7 |
3.8 |
2.9 |
875 |
16.5 |
73.4 |
69.9 |
16.2 |
|
Systemic connective tissue disorders |
1,660 |
66.7 |
1.7 |
1.3 |
927 |
17.4 |
66.0 |
63.1 |
12.9 |
|
Spondylopathies |
413 |
16.6 |
2.7 |
1.7 |
3,513 |
66.1 |
89.6 |
87.0 |
23.5 |
|
Diseases of the genitourinary system |
6,202 |
4.6 |
3.9 |
2.6 |
4,193 |
3.3 |
77.8 |
75.0 |
17.8 |
|
Congenital malformations of the urinary system |
1,147 |
18.5 |
2.7 |
1.7 |
443 |
10.6 |
77.4 |
75.2 |
14.9 |
|
Glomerular disease |
1,679 |
27.1 |
3.6 |
2.4 |
1,700 |
40.5 |
73.9 |
70.7 |
14.5 |
|
Tubulointerstitial disease |
3,162 |
51.0 |
2.5 |
1.8 |
1,728 |
41.2 |
84.1 |
81,7 |
21.8 |
|
Chronic kidney disease |
214 |
3.5 |
6.1 |
2.8 |
322 |
7.7 |
65.2 |
60.9 |
17.7 |
|
Congenital malformations, deformations, and chromosomal abnormalities |
1,790 |
1.3 |
2.5 |
1.5 |
1,625 |
1.4 |
81.7 |
79.0 |
19.3 |

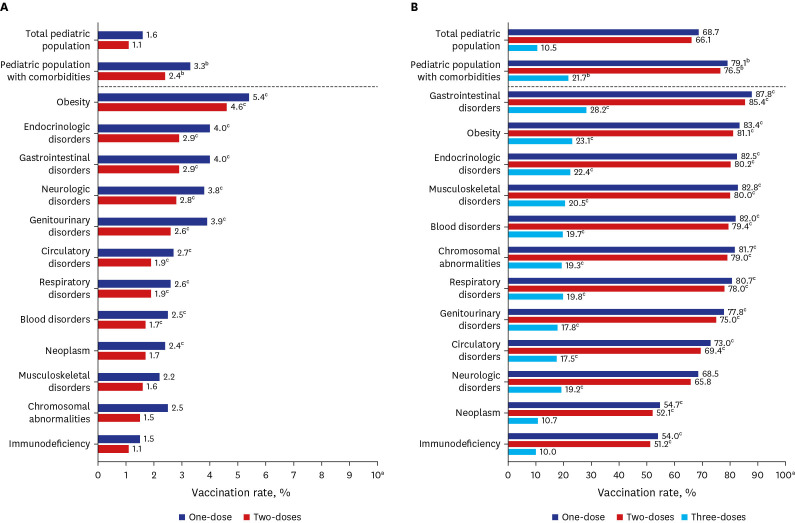
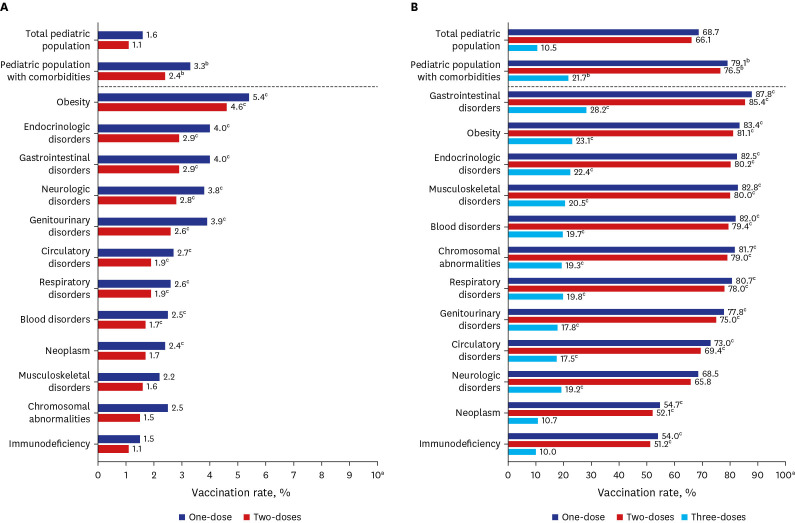
Overall vaccination rates among the pediatric population with comorbidities appeared to be higher than those of the general pediatric population regardless of age group and number of doses received (
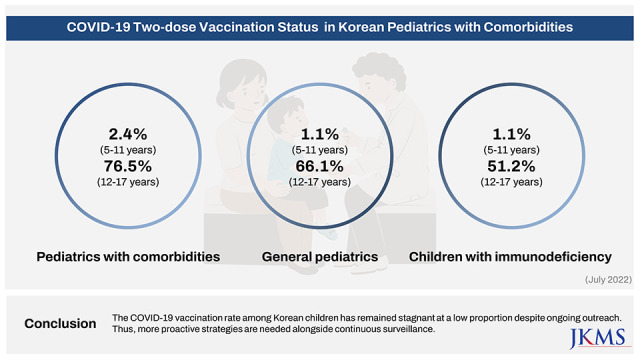
Fig. 1). Among the total 5–17-year-olds, two-dose vaccination rates were 36.2% in children with comorbidities and 32.0% in the general pediatric population. In the 5–11 years age group, 1.1% of all children and 2.4% of children with comorbidities received at least two vaccine doses (
P < 0.001). In the 12–17 years age group, 66.1% of all adolescents and 76.5% of adolescents with comorbidities received at least two COVID-19 vaccine doses (
P < 0.001). Of note, the third-dose vaccination rate for the 12–17 years age group was two times higher in the comorbidity group (21.7%) than in the general pediatric population (10.5%) (
P < 0.001). We organized comorbidity categories in descending order of two-dose vaccination rate for each age group (
Fig. 1). Pediatric patients with gastrointestinal disorders, obesity, and endocrinologic disorders showed the highest vaccination rates, while patients with immunodeficiency had the lowest vaccination rates in both age groups. For 12–17-year-olds, both immunodeficiency group (51.2% vs. 66.1%,
P < 0.001) and neoplasm group (51.2% vs. 66.1%,
P < 0.001) showed lower two-dose vaccination rate than the general population with a statistical difference.
Fig. 1
Differential tendency of COVID-19 vaccination rates for comorbidity categories.
(A) 5–11 years and (B) 12–17 years age groups.
COVID-19 = coronavirus disease 2019.
aThere is a significant difference between the maximum values of the graphs (10% vs. 100%).
bThis indicates a significant difference between vaccination rates of pediatric population with comorbidities compared to that of total pediatric population in age groups via binomial distribution (P < 0.001).
cThis indicates a significant difference between vaccination rates of each comorbidity category compared to that of total pediatric population in age groups via binomial distribution (P < 0.001).

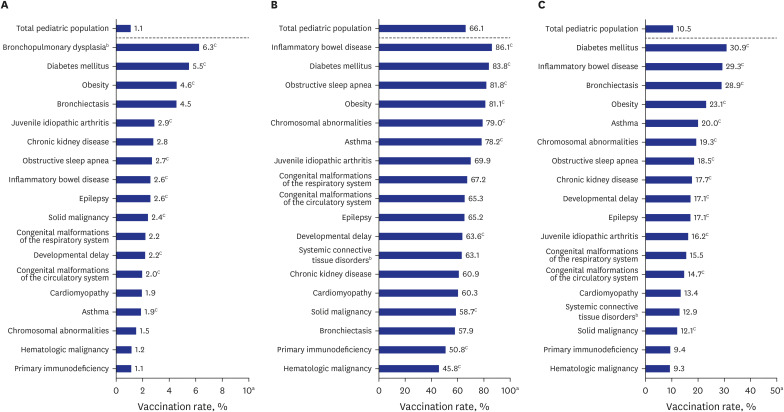
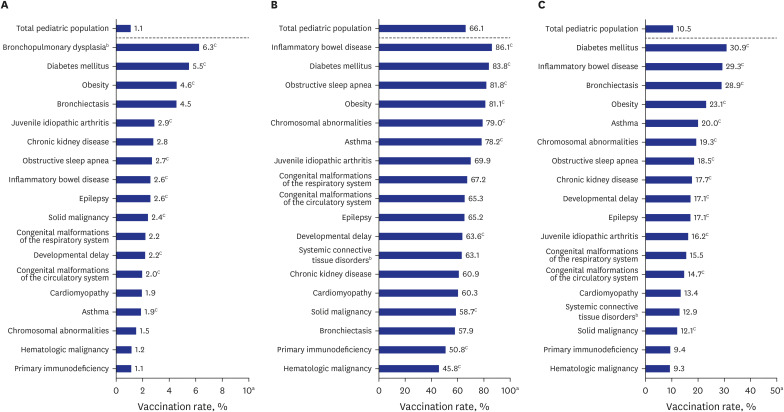
Vaccination rates at the individual disease level were further analyzed (
Fig. 2). Interestingly, respiratory diseases such as bronchopulmonary dysplasia in the 5–11-year-old group (two-dose), obstructive sleep apnea in the 12–17-year-old group (two-dose), and bronchiectasis in the 12–17-year-old group (three-dose) ranked high. Similarly, the lowest vaccination tendency was found among children with primary immunodeficiencies or hematologic malignancies. For 12–17-year-olds, primary immunodeficiency (50.8% vs. 66.1%,
P < 0.001) and hematologic malignancy (45.8% vs. 66.1%,
P < 0.001) showed a lower two-dose vaccination rate than the general population with a statistical difference.
Fig. 2
Differential tendency of COVID-19 vaccination rates for individual diseases including high-risk disorders.
(A) Two-dose vaccination rates in 5–11 years. (B) Two-dose vaccination rates in 12–17 years. (C) Three-dose vaccination rates in 12–17 years.
COVID-19 = coronavirus disease 2019.
aThere are significant differences between the maximum values of the graphs (10% vs. 100% vs. 50%).
bBronchopulmonary dysplasia was included for the 5–11-year-olds but was excluded for the 12–17-year-olds considering the disease epidemiology. In the same context, systemic connective tissue disorders were included in the 12–17-year-olds but were excluded for the 5–11-year-olds.
cThis indicates a significant difference between vaccination rates of patients with each individual disease compared to that of total pediatric population in age groups via binomial distribution (P < 0.001).

In summary, despite the overall low COVID-19 vaccination rate among Korean children, the vaccination rate of children with comorbidities was higher than that of the general pediatric population. However, there was a substantial difference as large as 30% in the rate among comorbidity categories. Children with immunodeficiencies or hematologic malignancies, who are high-risk for severe COVID-19, had the lowest vaccination rate.
14
Pediatric COVID-19 vaccine hesitancy, a delay in acceptance of vaccines despite availability, has become a global phenomenon. A recent study found that parents who are hesitant toward general childhood vaccines are more likely to be hesitant toward the COVID-19 vaccine.
15 In Korea, even considering the difference in the level of recommendation, the low COVID-19 vaccination rate in children 5–11-year-olds is in sharp contrast to the traditionally high acceptance rate for National Immunization Program (NIP), although comparing the vaccination rates between the COVID-19 vaccine (recommended for high-risk children) and the NIP vaccine (recommended for all children) may not be fair.
1617
Since the COVID-19 vaccination in children 5–11 years is recommended only in high-risk group and remained a choice among most healthy children in Korea, whether to get COVID-19 vaccination largely depends on their parents’ autonomy. Therefore, parental value judgement weighing the pros and cons of the pediatric vaccination for COVID-19 ever became more important and it appeared to be skewed to conclude not getting a vaccination for their final decision among most Korean parents. One explanation might be the ‘infodemic’ of common digital rumors which cause misunderstanding to parents to defer COVID-19 vaccination of children.
181920
In this context, consistent and proactive recommendations from pediatricians are crucial to promote parental motivation toward pediatric COVID-19 vaccination. For instance, pediatricians who encounter immunocompromised children in their clinics should offer proactive vaccinations and recommendations.
1421 Additionally, customized consultation to address individual concerns about COVID-19 vaccination from the family of high-risk children would be ideal. However, considering the reality of the limited time pediatricians have at a busy clinic, a simple scale assessing the influence of comorbidity on COVID-19 vaccine acceptance can be introduced as a point-of-care tool for targeted counseling.
22 Currently, COVID-19 vaccination in children 5–17 years old is only provided at primary care facilities, while most children with comorbidities within this age group are followed up at tertiary care centers that do not provide COVID-19 vaccines as part of their routine health care services.
Beginning in February 2023, COVID-19 vaccination for children 6 months and older has been implemented in Korea. Unlike prior implementations, COVID-19 vaccination service was provided at tertiary hospitals as well as primary clinics, which may be helpful to overcome the current COVID-19 vaccine hesitancy for the Korean pediatric population with comorbidities.
Meanwhile, the cumulative number of COVID-19 patients aged 0–19 years in Korea was 6,876,624 as of February 19th, 2023, representing 83.7% of the population in this age group.
23 Thus, the majority of the pediatric population acquired immunity against COVID-19 through natural infection rather than vaccination, as reflected by their high severe acute respiratory syndrome coronavirus 2 nucleocapsid protein seropositivity rate compared with other age groups (5–9 years [90.0%] vs. total [70.0%]) as of January 2023.
24 However, as immunity wanes over time, pediatricians should remain alert to the importance of continuous vaccination of high-risk children including immunocompromised children, even in the post-pandemic era.
This study has several limitations. First, since the disease codes used for data collection were not validated systematically, this could be the limitation to estimate the individual vaccination rates comprehensively. In addition, patients with multiple underlying diseases were accounted for the single main diagnosis. Second, we could only define the high-risk group according to underlying disease categories, although recent studies suggest that COVID-19 risk assignment should be stratified according to disease severity and treatment status.
25 Third, patients receiving immunosuppressive drugs for systemic conditions such as organ-transplant status could not be accounted for separately in the study.
In conclusion, COVID-19 vaccination rates among pediatric population with comorbidities were low, especially in the younger age group (5–11 years). Rates also differed substantially according to underlying disease and were particularly low among children with immunocompromised conditions in all age groups (5–17 years). Because the COVID-19 vaccination rate among Korean children with high-risk disorders is stagnant within a significantly low range despite continuing implementation efforts, more proactive strategies are needed with continuous surveillance.
Ethics statement
This study was approved by the Institutional Review Board of the Gil Medical Center (GCIRB2023-113). Participant consent was waived by the ethics committee because the data involved routinely collected medical data that was processed anonymously at all stages. The study methods were carried out based on the Declaration of Helsinki.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download