1. Hargrave D, Bartels U, Bouffet E. Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol. 2006; 7:241–248. PMID:
16510333.
2. Jansen MH, van Vuurden DG, Vandertop WP, Kaspers GJ. Diffuse intrinsic pontine gliomas: a systematic update on clinical trials and biology. Cancer Treat Rev. 2012; 38:27–35. PMID:
21764221.
3. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID:
27157931.
4. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021; 23:1231–1251. PMID:
34185076.
5. Lassman LP, Arjona VE. Pontine gliomas of childhood. Lancet. 1967; 1:913–915. PMID:
4164397.
6. Langmoen IA, Lundar T, Storm-Mathisen I, Lie SO, Hovind KH. Management of pediatric pontine gliomas. Childs Nerv Syst. 1991; 7:13–15. PMID:
2054800.
7. Frazier JL, Lee J, Thomale UW, Noggle JC, Cohen KJ, Jallo GI. Treatment of diffuse intrinsic brainstem gliomas: failed approaches and future strategies. J Neurosurg Pediatr. 2009; 3:259–269. PMID:
19338403.
8. Jansen MH, Veldhuijzen van Zanten SE, Sanchez Aliaga E, Heymans MW, Warmuth-Metz M, Hargrave D, et al. Survival prediction model of children with diffuse intrinsic pontine glioma based on clinical and radiological criteria. Neuro Oncol. 2015; 17:160–166. PMID:
24903904.
9. Jenkin RD, Boesel C, Ertel I, Evans A, Hittle R, Ortega J, et al. Brainstem tumors in childhood: a prospective randomized trial of irradiation with and without adjuvant CCNU, VCR, and prednisone. A report of the childrens cancer study group. J Neurosurg. 1987; 66:227–233. PMID:
3806204.
10. Kim HJ, Lee JH, Kim Y, Lim DH, Park SH, Ahn SD, et al. Suggestions for escaping the dark ages for pediatric diffuse intrinsic pontine glioma treated with radiotherapy: analysis of prognostic factors from the national multicenter study. Cancer Res Treat. 2022; 03. 04. DOI:
10.4143/crt.2021.1514. [Epub].
11. Halperin EC. Pediatric brain stem tumors: patterns of treatment failure and their implications for radiotherapy. Int J Radiat Oncol Biol Phys. 1985; 11:1293–1298. PMID:
2989230.
12. Massimino M, Spreafico F, Biassoni V, Simonetti F, Riva D, Trecate G, et al. Diffuse pontine gliomas in children: changing strategies, changing results? A mono-institutional 20-year experience. J Neurooncol. 2008; 87:355–361. PMID:
18217208.
13. Chassot A, Canale S, Varlet P, Puget S, Roujeau T, Negretti L, et al. Radiotherapy with concurrent and adjuvant temozolomide in children with newly diagnosed diffuse intrinsic pontine glioma. J Neurooncol. 2012; 106:399–407. PMID:
21858607.
14. Gallitto M, Lazarev S, Wasserman I, Stafford JM, Wolden SL, Terezakis SA, et al. Role of radiation therapy in the management of diffuse intrinsic pontine glioma: a systematic review. Adv Radiat Oncol. 2019; 4:520–531. PMID:
31360809.
15. Hoffman LM, Veldhuijzen van Zanten SEM, Colditz N, Baugh J, Chaney B, et al. Clinical, radiologic, pathologic, and molecular characteristics of long-term survivors of diffuse intrinsic pontine glioma (DIPG): a collaborative report from the International and European Society for pediatric oncology DIPG registries. J Clin Oncol. 2018; 36:1963–1972. PMID:
29746225.
16. Robison NJ, Kieran MW. Diffuse intrinsic pontine glioma: a reassessment. J Neurooncol. 2014; 119:7–15. PMID:
24792486.
17. Rhodes A, Martin S, Toledo-Tamula MA, Loucas C, Glod J, Warren KE, et al. The neuropsychological profile of children with diffuse intrinsic pontine glioma (DIPG) before and after radiation therapy: a prospective longitudinal study. Child Neuropsychol. 2022; 11. 11. DOI:
10.1080/09297049.2022.2144189. [Epub].
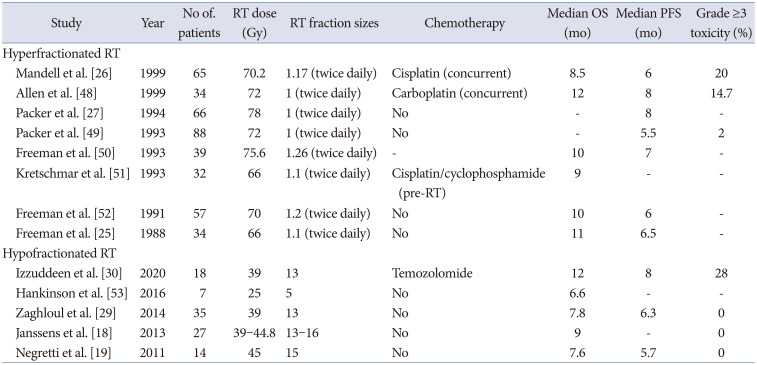
18. Janssens GO, Jansen MH, Lauwers SJ, Nowak PJ, Oldenburger FR, Bouffet E, et al. Hypofractionation vs conventional radiation therapy for newly diagnosed diffuse intrinsic pontine glioma: a matched-cohort analysis. Int J Radiat Oncol Biol Phys. 2013; 85:315–320. PMID:
22682807.
19. Negretti L, Bouchireb K, Levy-Piedbois C, Habrand JL, Dhermain F, Kalifa C, et al. Hypofractionated radiotherapy in the treatment of diffuse intrinsic pontine glioma in children: a single institution’s experience. J Neurooncol. 2011; 104:773–777. PMID:
21327862.
20. Cohen KJ, Heideman RL, Zhou T, Holmes EJ, Lavey RS, Bouffet E, et al. Temozolomide in the treatment of children with newly diagnosed diffuse intrinsic pontine gliomas: a report from the children’s oncology group. Neuro Oncol. 2011; 13:410–416. PMID:
21345842.
21. Baxter PA, Su JM, Onar-Thomas A, Billups CA, Li XN, Poussaint TY, et al. A phase I/II study of veliparib (ABT-888) with radiation and temozolomide in newly diagnosed diffuse pontine glioma: a pediatric brain tumor consortium study. Neuro Oncol. 2020; 22:875–885. PMID:
32009149.
22. Tinkle CL, Simone B, Chiang J, Li X, Campbell K, Han Y, et al. Defining optimal target volumes of conformal radiation therapy for diffuse intrinsic pontine glioma. Int J Radiat Oncol Biol Phys. 2020; 106:838–847. PMID:
31785339.
23. Salazar OM, Rubin P, Feldstein ML, Pizzutiello R. High dose radiation therapy in the treatment of malignant gliomas: final report. Int J Radiat Oncol Biol Phys. 1979; 5:1733–1740. PMID:
231023.
24. Thames HD Jr, Withers HR, Peters LJ, Fletcher GH. Changes in early and late radiation responses with altered dose fractionation: implications for dose-survival relationships. Int J Radiat Oncol Biol Phys. 1982; 8:219–226. PMID:
7085377.
25. Freeman CR, Krischer J, Sanford RA, Burger PC, Cohen M, Norris D. Hyperfractionated radiotherapy in brain stem tumors: results of a pediatric oncology group study. Int J Radiat Oncol Biol Phys. 1988; 15:311–318. PMID:
2841262.
26. Mandell LR, Kadota R, Freeman C, Douglass EC, Fontanesi J, Cohen ME, et al. There is no role for hyperfractionated radiotherapy in the management of children with newly diagnosed diffuse intrinsic brainstem tumors: results of a pediatric oncology group phase III trial comparing conventional vs. hyperfractionated radiotherapy. Int J Radiat Oncol Biol Phys. 1999; 43:959–964. PMID:
10192340.
27. Packer RJ, Boyett JM, Zimmerman RA, Albright AL, Kaplan AM, Rorke LB, et al. Outcome of children with brain stem gliomas after treatment with 7800 cGy of hyperfractionated radiotherapy. A childrens cancer group phase 1/11 trial. Cancer. 1994; 74:1827–1834. PMID:
8082086.
28. Hu X, Fang Y, Hui X, Jv Y, You C. Radiotherapy for diffuse brainstem glioma in children and young adults. Cochrane Database Syst Rev. 2016; 2016:CD010439. PMID:
27378212.
29. Zaghloul MS, Eldebawy E, Ahmed S, Mousa AG, Amin A, Refaat A, et al. Hypofractionated conformal radiotherapy for pediatric diffuse intrinsic pontine glioma (DIPG): a randomized controlled trial. Radiother Oncol. 2014; 111:35–40. PMID:
24560760.
30. Izzuddeen Y, Gupta S, Haresh KP, Sharma D, Giridhar P, Rath GK. Hypofractionated radiotherapy with temozolomide in diffuse intrinsic pontine gliomas: a randomized controlled trial. J Neurooncol. 2020; 146:91–95. PMID:
31728883.
31. Park J, Yea JW, Park JW. Hypofractionated radiotherapy versus conventional radiotherapy for diffuse intrinsic pontine glioma: a systematic review and meta-analysis. Medicine (Baltimore). 2020; 99:e22721. PMID:
33080729.
32. Zaghloul MS, Nasr A, Tolba M, Refaat A, Youssef A, Mosaab A, et al. Hypofractionated radiation therapy for diffuse intrinsic pontine glioma: a noninferiority randomized study including 253 children. Int J Radiat Oncol Biol Phys. 2022; 113:360–368. PMID:
35150788.
33. Muroi A, Mizumoto M, Ishikawa E, Ihara S, Fukushima H, Tsurubuchi T, et al. Proton therapy for newly diagnosed pediatric diffuse intrinsic pontine glioma. Childs Nerv Syst. 2020; 36:507–512. PMID:
31728705.
34. Indelicato DJ, Rotondo RL, Uezono H, Sandler ES, Aldana PR, Ranalli NJ, et al. Outcomes following proton therapy for pediatric low-grade glioma. Int J Radiat Oncol Biol Phys. 2019; 104:149–156. PMID:
30684665.
35. Indelicato DJ, Flampouri S, Rotondo RL, Bradley JA, Morris CG, Aldana PR, et al. Incidence and dosimetric parameters of pediatric brainstem toxicity following proton therapy. Acta Oncol. 2014; 53:1298–1304. PMID:
25279957.
36. Upadhyay R, Liao K, Grosshans DR, McGovern SL, Frances McAleer M, Zaky W, et al. Quantifying the risk and dosimetric variables of symptomatic brainstem injury after proton beam radiation in pediatric brain tumors. Neuro Oncol. 2022; 24:1571–1581. PMID:
35157767.
37. Yock TI, Constine LS, Mahajan A. Protons, the brainstem, and toxicity: ingredients for an emerging dialectic. Acta Oncol. 2014; 53:1279–1282. PMID:
25327262.
38. Haas-Kogan D, Indelicato D, Paganetti H, Esiashvili N, Mahajan A, Yock T, et al. National Cancer Institute workshop on proton therapy for children: considerations regarding brainstem injury. Int J Radiat Oncol Biol Phys. 2018; 101:152–168. PMID:
29619963.
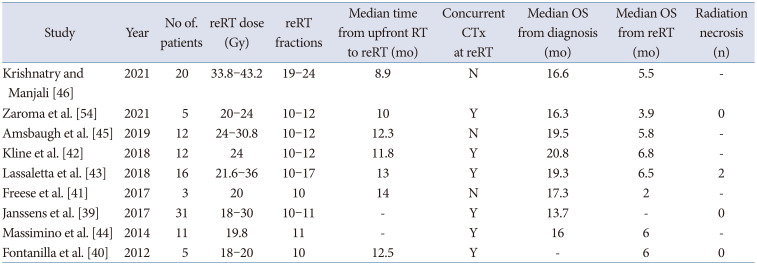
39. Janssens GO, Gandola L, Bolle S, Mandeville H, Ramos-Albiac M, van Beek K, et al. Survival benefit for patients with diffuse intrinsic pontine glioma (DIPG) undergoing re-irradiation at first progression: a matched-cohort analysis on behalf of the SIOP-E-HGG/DIPG working group. Eur J Cancer. 2017; 73:38–47. PMID:
28161497.
40. Fontanilla HP, Pinnix CC, Ketonen LM, Woo SY, Vats TS, Rytting ME, et al. Palliative reirradiation for progressive diffuse intrinsic pontine glioma. Am J Clin Oncol. 2012; 35:51–57. PMID:
21297433.
41. Freese C, Takiar V, Fouladi M, DeWire M, Breneman J, Pater L. Radiation and subsequent reirradiation outcomes in the treatment of diffuse intrinsic pontine glioma and a systematic review of the reirradiation literature. Pract Radiat Oncol. 2017; 7:86–92. PMID:
28274399.
42. Kline C, Liu SJ, Duriseti S, Banerjee A, Nicolaides T, Raber S, et al. Reirradiation and PD-1 inhibition with nivolumab for the treatment of recurrent diffuse intrinsic pontine glioma: a single-institution experience. J Neurooncol. 2018; 140:629–638. PMID:
30206764.
43. Lassaletta A, Strother D, Laperriere N, Hukin J, Vanan MI, Goddard K, et al. Reirradiation in patients with diffuse intrinsic pontine gliomas: the Canadian experience. Pediatr Blood Cancer. 2018; 65:e26988. PMID:
29369515.
44. Massimino M, Biassoni V, Miceli R, Schiavello E, Warmuth-Metz M, Modena P, et al. Results of nimotuzumab and vinorelbine, radiation and re-irradiation for diffuse pontine glioma in childhood. J Neurooncol. 2014; 118:305–312. PMID:
24696052.
45. Amsbaugh MJ, Mahajan A, Thall PF, McAleer MF, Paulino AC, Grosshans D, et al. A phase 1/2 trial of reirradiation for diffuse intrinsic pontine glioma. Int J Radiat Oncol Biol Phys. 2019; 104:144–148. PMID:
30610915.
46. Krishnatry R, Manjali JJ. Clinical approach to re-irradiation for recurrent diffuse intrinsic pontine glioma. Jpn J Clin Oncol. 2021; 51:762–768. PMID:
33521824.
47. Lu VM, Welby JP, Mahajan A, Laack NN, Daniels DJ. Reirradiation for diffuse intrinsic pontine glioma: a systematic review and meta-analysis. Childs Nerv Syst. 2019; 35:739–746. PMID:
30879125.
48. Allen J, Siffert J, Donahue B, Nirenberg A, Jakacki R, Robertson P, et al. A phase I/II study of carboplatin combined with hyperfractionated radiotherapy for brainstem gliomas. Cancer. 1999; 86:1064–1069. PMID:
10491535.
49. Packer RJ, Zimmerman RA, Kaplan A, Wara WM, Rorke LB, Selch M, et al. Early cystic/necrotic changes after hyperfractionated radiation therapy in children with brain stem gliomas. Data from the Childrens Cancer Group. Cancer. 1993; 71:2666–2674. PMID:
8453590.
50. Freeman CR, Krischer JP, Sanford RA, Cohen ME, Burger PC, del Carpio R, et al. Final results of a study of escalating doses of hyperfractionated radiotherapy in brain stem tumors in children: a Pediatric Oncology Group study. Int J Radiat Oncol Biol Phys. 1993; 27:197–206. PMID:
8407392.
51. Kretschmar CS, Tarbell NJ, Barnes PD, Krischer JP, Burger PC, Kun L. Pre-irradiation chemotherapy and hyperfractionated radiation therapy 66 Gy for children with brain stem tumors. A phase II study of the Pediatric Oncology Group, Protocol 8833. Cancer. 1993; 72:1404–1413. PMID:
8339231.
52. Freeman CR, Krischer J, Sanford RA, Cohen ME, Burger PC, Kun L, et al. Hyperfractionated radiation therapy in brain stem tumors. Results of treatment at the 7020 cGy dose level of Pediatric Oncology Group study #8495. Cancer. 1991; 68:474–481. PMID:
2065266.
53. Hankinson TC, Patibandla MR, Green A, Hemenway M, Foreman N, Handler M, et al. Hypofractionated radiotherapy for children with diffuse intrinsic pontine gliomas. Pediatr Blood Cancer. 2016; 63:716–718. PMID:
26544789.
54. Zamora PL, Miller SR, Kovoor JJ. Single institution experience in reirradiation of biopsy-proven diffuse intrinsic pontine gliomas. Childs Nerv Syst. 2021; 37:2539–2543. PMID:
33973056.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download