Abstract
Nontuberculous mycobacteria (NTM) is a type of bacteria that typically infects the pulmonary system, and NTM–central nervous system (CNS) infection, which occurs in the brain, is a very rare disease. A 64-year-old female patient presented with seizures as the main symptom and was found to have a mass of less than 1 cm in the right temporal lobe with accompanying edema. Although diseases such as tumor metastasis and parasitic cyst were suspected, the patient underwent a surgical resection, and NTM-CNS infection with abscess was diagnosed through biopsy. Antibiotic treatment was initiated after surgery, and the patient has been followed up without any significant symptoms. In this report, we review a rare case of NTM-CNS infection and discuss the understanding and treatment of this disease.
Infections caused by nontuberculous mycobacteria (NTM) can be divided into two groups based on their growth rate: slow-growing and rapid-growing. The most common type of infection is in the pulmonary system [1]. On the other hand, CNS infection is very rare and is mostly reported in immunocompromised patients, such as those with human immunodeficiency virus (HIV) infection, with a very poor prognosis [23]. Treatment requires the use of intravenous and oral antibiotics that can pass through the blood-brain and blood–cerebrospinal fluid (CSF) barriers for an extended period [4]. Here, we introduce a patient who had NTM-CNS infection with abscess but did not have any specific immunodeficiency disorder, and we hope that this report will be helpful in understanding and treating similar patients.
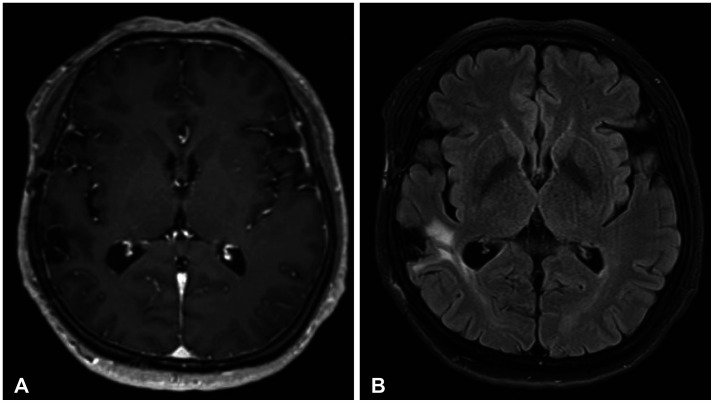
A 64-year-old female patient was admitted to the hospital as an outpatient through neurology department due to a generalized tonic-clonic type seizure that occurred the day before. Brain CT performed after admission revealed findings of edema in the surrounding area with a mass of about 1 cm in the right temporal lobe. Brain MRI was performed and the results were interpreted by the neurology and radiology departments, which showed findings most likely indicating metastasis, differential diagnosis of parasitic cyst or tuberculosis granuloma (Fig. 1). To confirm the presence of metastasis, chest and abdomen CT-enhance were performed, but no mass was found. Blood tests for tumor markers were also normal, confirming the absence of metastasis. Lumbar tapping was performed along with a parasite antibody test and CSF study and cytology to rule out the possibility of a non-tumor diagnosis. The parasite antibody test showed a negative result, and CSF study showed normal laboratory values for glucose and protein. The WBC count was checked and found to be 3 cells/mm3, but it was determined to be an insignificant value. Malignant cells were not detected in the cytology. Therefore, it was determined that surgical excision and biopsy would be necessary for the brain mass. The patient was referred to the neurosurgery department for navigation guided craniotomy with tumor removal. The surgery was successful, and the mass was completely removed. Postoperative CT and MRI showed no signs of residual mass (Fig. 2). The patient recovered in the intensive care unit with no neurological deficits and alert mental status. Biopsy results obtained 10 days after surgery showed granuloma with abscess, and the mycobacterium tuberculosis (MTB)-NTM polymerase chain reaction (PCR) test showed negative for MTB in PCR and positive for NTM in PCR. Fungus or acid-fast bacilli cannot be found on special staining (Fig. 3). After consultation with the infectious disease department, additional tests for species confirmation were not performed. However, it was suspected that the patient was infected with rapid-growing NTM, and treatment with clarithromycin, amikacin, and imipenem was initiated. PCR was not performed on the CSF sample. The patient underwent a serum test for HIV infection prior to the surgery, and it confirmed a negative result. Additionally, the patient was not taking any immunosuppressive medication and was not undergoing any anticancer treatment, indicating a non-immunocompromised condition. After approximately 2 weeks of treatment, the patient’s wound at the operation site had healed, and total stitch out was performed. The patient was then discharged and continued taking clarithromycin and moxifloxacin orally. About 2 weeks later, the patient visited the infectious disease department as an outpatient, reporting side effects of fever and diarrhea. The medication was changed to clarithromycin and levofloxacin, and there were no further side effects. The patient continued taking the medication for 12 months without any signs of recurrence, and follow-up appointments revealed no further issues (Fig. 4).
NTM is a ubiquitous environmental microorganism that can cause infection in humans while living in natural environments such as soil and water [5]. The most common strains are Mycobacterium avium complex (MAC) and Mycobacterium abscessus [6]. NTM infections are increasing worldwide and are known to occur in the respiratory system, lymphatic system, skin, and connective tissue. Respiratory infections are the most common, while CNS infections are very rare. In one study, only 15 out of 5,960 NTM-infected patients (0.25%) were reported to have NTM-CNS infections [7]. Furthermore, even in most cases, it is reported to occur in immunocompromised patients such as those with HIV infection, malignancy, etc. [389].
Symptoms of NTM-CNS infection can vary and include headache, fever, seizures, altered consciousness, etc. [7810]. They are nonspecific and difficult to distinguish from other CNS infections, making diagnosis challenging. Even if abscesses are seen in imaging tests, they may be small and not exhibit significant symptoms, making it easy to overlook the use of NTM targeted antibiotics when selecting drug therapy.
The treatment of NTM-CNS infection is based on antimicrobial therapy and requires prolonged and multidrug regimens. Clarithromycin, azithromycin, rifabutin, ethambutol, amikacin or streptomycin, and levofloxacin or moxifloxacin can be used [3]. The optimal duration and which drugs to use have not yet been established, and guidelines vary widely. Ultimately, it is important to determine which NTM strain is growing in the patient, and surgical intervention may be necessary to obtain a strain for culture. In addition to culture, surgical intervention may also be necessary to drain abscesses and remove infected tissue [11].
In this case report, we discussed a patient with NTM-CNS infection who was not immunocompromised, which is a very rare case. If we miss the diagnosis, it can be extremely fatal, and the patient may die. Through this case report, we aim to examine NTM-CNS infection cases and provide assistance in diagnosis and treatment.
Notes
Ethics Statement: The Institutional Review Board (IRB) exempted informed consent due to its retrospective descriptive nature (case report) and minimal risk for harm to the patient.
Availability of Data and Material
All data generated or analyzed during the study are included in this published article.
References
1. Wagner D, Young LS. Nontuberculous mycobacterial infections: a clinical review. Infection. 2004; 32:257–270. PMID: 15624889.
2. Flor A, Capdevila JA, Martin N, Gavaldà J, Pahissa A. Nontuberculous mycobacterial meningitis: report of two cases and review. Clin Infect Dis. 1996; 23:1266–1273. PMID: 8953070.
3. Cai R, Qi T, Lu H. Central nervous system infection with non-tuberculous mycobacteria: a report of that infection in two patients with AIDS. Drug Discov Ther. 2014; 8:276–279. PMID: 25639308.
4. Franco-Paredes C. Infections of the central nervous system caused by nontuberculous mycobacteria. Kon K, Rai M, editors. The microbiology of central nervous system infections. Cambridge, MA: Academic Press;2018. p. 141–147.
5. Falkinham JO III. Ecology of nontuberculous mycobacteria. Microorganisms. 2021; 9:2262. PMID: 34835388.
6. Shin SH, Jhun BW, Kim SY, Choe J, Jeon K, Huh HJ, et al. Nontuberculous mycobacterial lung diseases caused by mixed infection with Mycobacterium avium complex and Mycobacterium abscessus complex. Antimicrob Agents Chemother. 2018; 62:e01105–e01118. PMID: 30104265.
7. Lee MR, Cheng A, Lee YC, Yang CY, Lai CC, Huang YT, et al. CNS infections caused by Mycobacterium abscessus complex: clinical features and antimicrobial susceptibilities of isolates. J Antimicrob Chemother. 2012; 67:222–225. PMID: 21980068.
8. Karne SS, Sangle SA, Kiyawat DS, Dharmashale SN, Kadam DB, Bhardwaj RS. Mycobacterium avium-intracellulare brain abscess in HIV-positive patient. Ann Indian Acad Neurol. 2012; 15:54–55. PMID: 22412276.
9. Lee KD, Park WB, Jung HS, Kang CI, Kim DM, Kim HB, et al. Mycobacterium avium-intracellularae meningoencephalitis in a patient with acquired immunodeficiency syndrome. Infect Chemother. 2003; 35:306–309.
10. Talati NJ, Rouphael N, Kuppalli K, Franco-Paredes C. Spectrum of CNS disease caused by rapidly growing mycobacteria. Lancet Infect Dis. 2008; 8:390–398. PMID: 18501854.
11. Jarzembowski JA, Young MB. Nontuberculous mycobacterial infections. Arch Pathol Lab Med. 2008; 132:1333–1341. PMID: 18684037.
Fig. 1
Preoperative MRI images showing a lesion in the right temporal lobe. A: A circular lesion of approximately 1 cm in size, which is strongly enhanced with contrast, can be seen on contrast-enhanced image. B: On the axial T2 fluid-attenuated inversion recovery image, mild edema is visible in the periphery of the lesion. C: Central diffusion restriction is shown in diffusion-weighted sequence.
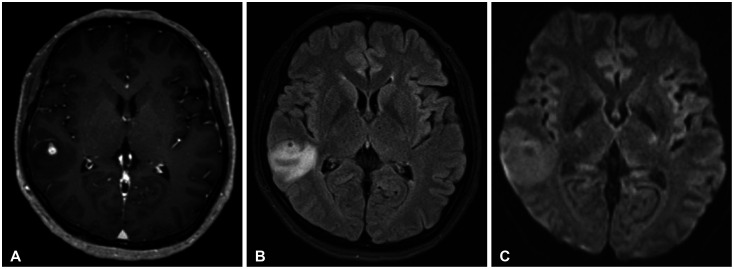
Fig. 2
Postoperative MRI images of the patient. A: The lesion that was enhanced with contrast before the surgery is not visible anymore. B: The surrounding area appears to have been resected on T2 fluid-attenuated inversion recovery image. C: No central diffusion restriction can be seen in diffusion-weighted image.
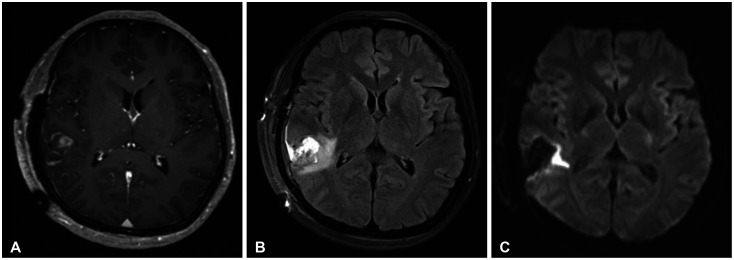
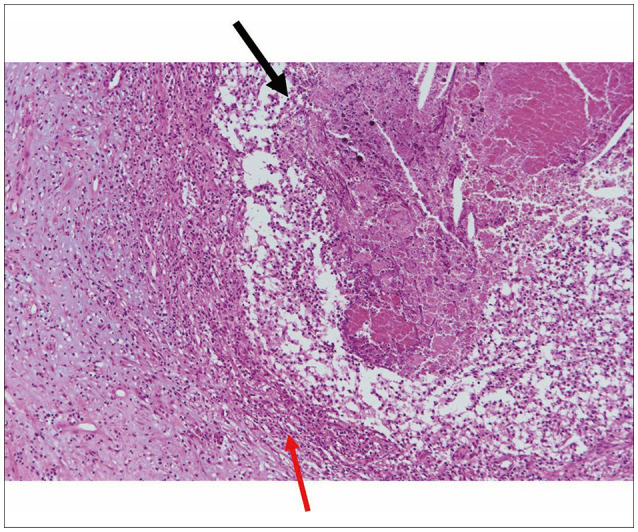
Fig. 3
A biopsy image stained with H&E at a magnification of ×100. The brain tissue shows abscess pockets containing cholesterol cleft, abscess, or fibrous wall (black arrow). Some of them show granulomatous inflammation in the abscess wall (red arrow). Fungus or acid fast bacilli cannot be found on special staining.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download