1. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109. PMID:
17618441.
2. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021; 23:1231–1251. PMID:
34185076.
3. Xiong L, Wang F, Qi Xie X. Advanced treatment in high-grade gliomas. J BUON. 2019; 24:424–430. PMID:
31127986.
4. Mehta S, Huillard E, Kesari S, Maire CL, Golebiowski D, Harrington EP, et al. The central nervous system-restricted transcription factor Olig2 opposes p53 responses to genotoxic damage in neural progenitors and malignant glioma. Cancer Cell. 2011; 19:359–371. PMID:
21397859.
5. Bock HC, Puchner MJ, Lohmann F, Schütze M, Koll S, Ketter R, et al. First-line treatment of malignant glioma with carmustine implants followed by concomitant radiochemotherapy: a multicenter experience. Neurosurg Rev. 2010; 33:441–449. PMID:
20706757.
6. Elena A, Melina C, Raffaele N, Carlo B, Vittoria N, Francesco A, et al. Extraneural metastases in glioblastoma patients: two cases with YKL-40-positive glioblastomas and a meta-analysis of the literature. Neurosurg Rev. 2016; 39:37–45. discussion 45-6. PMID:
26212701.
7. Santra A, Kumar R, Sharma P, Bal C, Julka PK, Malhotra A. Detection of recurrence in glioma: a comparative prospective study between Tc-99m GHA SPECT and F-18 FDG PET/CT. Clin Nucl Med. 2011; 36:650–655. PMID:
21716014.
8. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009; 10:459–466. PMID:
19269895.
9. Henriksson R, Asklund T, Poulsen HS. Impact of therapy on quality of life, neurocognitive function and their correlates in glioblastoma multiforme: a review. J Neurooncol. 2011; 104:639–646. PMID:
21468776.
10. Taphoorn MJ, Klein M. Cognitive deficits in adult patients with brain tumours. Lancet Neurol. 2004; 3:159–168. PMID:
14980531.
11. Mahalakshmi P, Vanisree AJ. Quality of life measures in glioma patients with different grades: a preliminary study. Indian J Cancer. 2015; 52:580–585. PMID:
26960484.
12. Acevedo-Vergara K, Perez-Florez M, Ramirez A, Torres-Bayona S, Dau A, Salva S, et al. Cognitive deficits in adult patients with high-grade glioma: a systematic review. Clin Neurol Neurosurg. 2022; 219:107296. PMID:
35662053.
13. van Kessel E, Baumfalk AE, van Zandvoort MJE, Robe PA, Snijders TJ. Tumor-related neurocognitive dysfunction in patients with diffuse glioma: a systematic review of neurocognitive functioning prior to anti-tumor treatment. J Neurooncol. 2017; 134:9–18. PMID:
28567586.
14. Sharma M, Juthani RG, Vogelbaum MA. Updated response assessment criteria for high-grade glioma: beyond the MacDonald criteria. Chin Clin Oncol. 2017; 6:37. PMID:
28841799.
15. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198. PMID:
1202204.
16. Bian Y, Meng L, Peng J, Li J, Wei R, Huo L, et al. Effect of radiochemotherapy on the cognitive function and diffusion tensor and perfusion weighted imaging for high-grade gliomas: a prospective study. Sci Rep. 2019; 9:5967. PMID:
30979930.
17. Weller M, van den Bent M, Preusser M, Le Rhun E, Tonn JC, Minniti G, et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol. 2021; 18:170–186. PMID:
33293629.
18. Niyazi M, Brada M, Chalmers AJ, Combs SE, Erridge SC, Fiorentino A, et al. ESTRO-ACROP guideline “target delineation of glioblastomas”. Radiother Oncol. 2016; 118:35–42. PMID:
26777122.
19. BDSS Corp. coGuide statistics software, version 1.0.3. : BDSS Corp. Bangalore: BDSS Corp.;2020. Accessed October 2 2022.
https://www.coguide.in
.
20. Lawrie TA, Gillespie D, Dowswell T, Evans J, Erridge S, Vale L, et al. Long-term neurocognitive and other side effects of radiotherapy, with or without chemotherapy, for glioma. Cochrane Database Syst Rev. 2019; 8:CD013047. PMID:
31425631.
21. Habets EJ, Taphoorn MJ, Nederend S, Klein M, Delgadillo D, Hoang-Xuan K, et al. Health-related quality of life and cognitive functioning in long-term anaplastic oligodendroglioma and oligoastrocytoma survivors. J Neurooncol. 2014; 116:161–168. PMID:
24162809.
22. Wang M, Cairncross G, Shaw E, Jenkins R, Scheithauer B, Brachman D, et al. Cognition and quality of life after chemotherapy plus radiotherapy (RT) vs. RT for pure and mixed anaplastic oligodendrogliomas: radiation therapy oncology group trial 9402. Int J Radiat Oncol Biol Phys. 2010; 77:662–669. PMID:
19783377.
23. Miotto EC, Junior AS, Silva CC, Cabrera HN, Machado MA, Benute GR, et al. Cognitive impairments in patients with low grade gliomas and high grade gliomas. Arq Neuropsiquiatr. 2011; 69:596–601. PMID:
21877026.
24. Wang Q, Qi F, Song X, Di J, Zhang L, Zhou Y, et al. A prospective longitudinal evaluation of cognition and depression in postoperative patients with high-grade glioma following radiotherapy and chemotherapy. J Cancer Res Ther. 2018; 14(Suppl 5):S1048–S1051. PMID:
30539844.
25. Hilverda K, Bosma I, Heimans JJ, Postma TJ, Peter Vandertop W, Slotman BJ, et al. Cognitive functioning in glioblastoma patients during radiotherapy and temozolomide treatment: initial findings. J Neurooncol. 2010; 97:89–94. PMID:
19718545.
26. Meyers CA, Wefel JS. The use of the mini-mental state examination to assess cognitive functioning in cancer trials: no ifs, ands, buts, or sensitivity. J Clin Oncol. 2003; 21:3557–3558. PMID:
12913103.
27. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005; 53:695–699. PMID:
15817019.
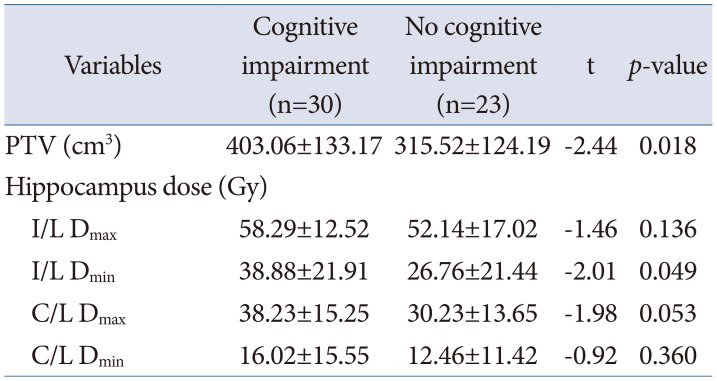
28. Wang Q, Xiao F, Qi F, Song X, Yu Y. Risk factors for cognitive impairment in high-grade glioma patients treated with postoperative radiochemotherapy. Cancer Res Treat. 2020; 52:586–593. PMID:
32019288.
29. Nagai R, Tsunoda S, Hori Y, Asada H. Selective vulnerability to radiation in the hippocampal dentate granule cells. Surg Neurol. 2000; 53:503–506. discussion 506-7. PMID:
10874152.
30. Diaz AZ, Choi M. Radiation-associated toxicities in the treatment of high-grade gliomas. Semin Oncol. 2014; 41:532–540. PMID:
25173145.
31. Madsen TM, Kristjansen PE, Bolwig TG, Wörtwein G. Arrested neuronal proliferation and impaired hippocampal function following fractionated brain irradiation in the adult rat. Neuroscience. 2003; 119:635–642. PMID:
12809684.
32. Rydelius A, Lätt J, Kinhult S, Engelholm S, Van Westen D, Pihlsgård M, et al. Longitudinal study of cognitive function in glioma patients treated with modern radiotherapy techniques and standard chemotherapy. Acta Oncol. 2020; 59:1091–1097. PMID:
32847475.
33. Binabaj MM, Bahrami A, ShahidSales S, Joodi M, Joudi Mashhad M, Hassanian SM, et al. The prognostic value of MGMT promoter methylation in glioblastoma: a meta-analysis of clinical trials. J Cell Physiol. 2018; 233:378–386. PMID:
28266716.
34. Waitkus MS, Diplas BH, Yan H. Isocitrate dehydrogenase mutations in gliomas. Neuro Oncol. 2016; 18:16–26. PMID:
26188014.
35. Bunevicius A, Miller J, Parsons M. Isocitrate dehydrogenase, patient-reported outcomes, and cognitive functioning of glioma patients: a systematic review. Curr Oncol Rep. 2020; 22:120. PMID:
32965568.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download