ABSTRACT
Recurrent colonic perforation in patients already having colostomy is extremely rare and only a few cases had been reported. Herein, we report 2 cases of recurrent colonic perforation at the proximal part of the colostomy in geriatric patients resulting from different causes, which might be caused by stercoral perforation and recurrent colonic ischemia, respectively. Based on our experience, surgeons should consider correcting chronic constipation even in patients who already have a colostomy. Additionally, transverse colostomy should be considered as a surgical treatment in patients with sigmoid colostomy for recurrent perforation due to colonic ischemia.
Go to : 
Sigmoid colon perforations are usually treated using the Hartmann procedure with end colostomy. Recurrent colonic perforation in patients undergoing colostomy is extremely rare, with only a few cases reported. Previous studies have reported recurrent colon perforation due to fecalomas in patients with sigmoid colostomy [1-3]. Herein, we report two cases of recurrent colon perforation in geriatric patients with sigmoid colostomy. The first case was thought to be due to stercoral perforation, as previously reported, but the second case was thought to be due to ischemic colitis, considering the patient’s history and operative findings. To the best of our knowledge, there have been no reports of recurrent colonic perforation due to colonic ischemia in patients with colostomy.
Go to : 
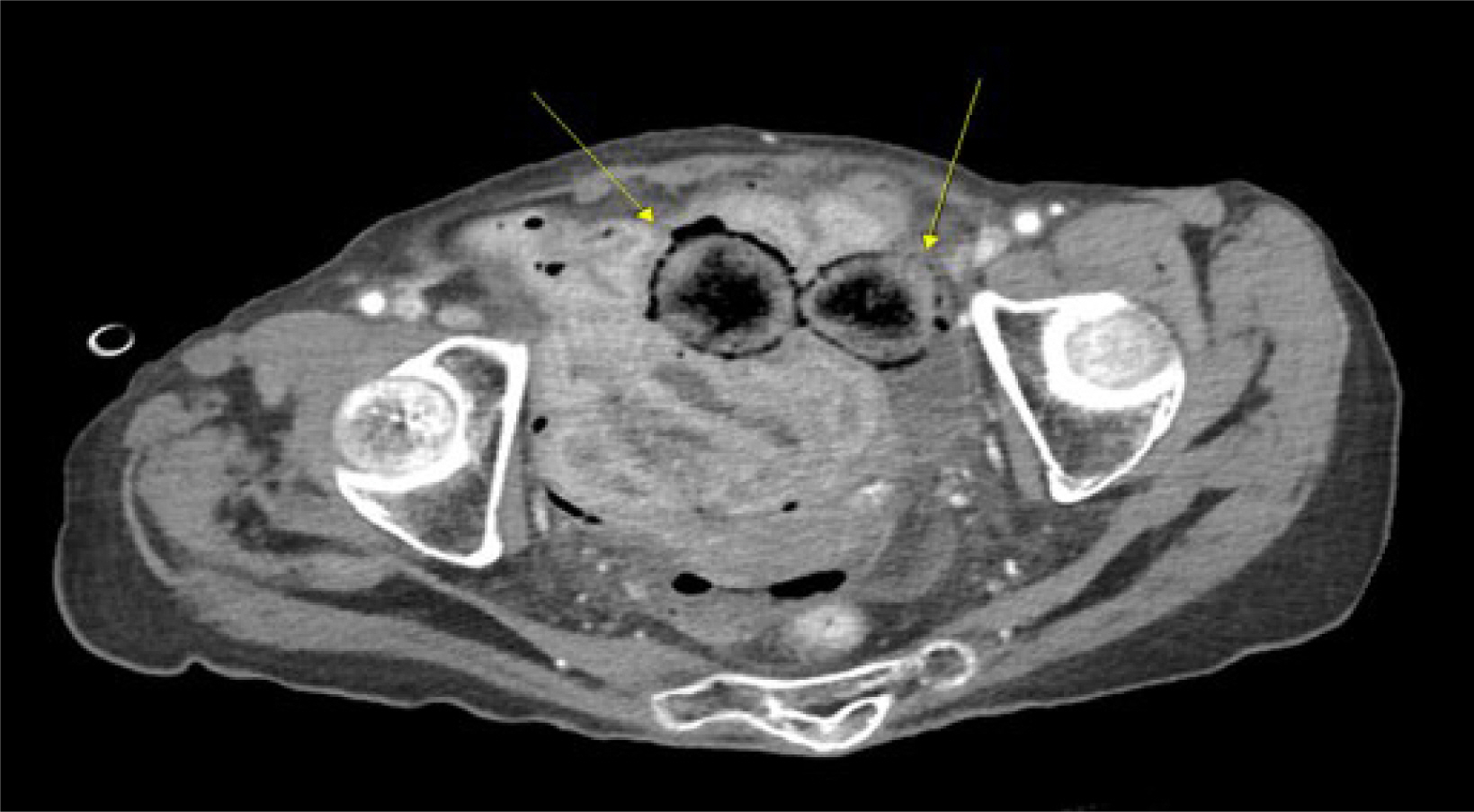
An 89-year-old bedridden woman with Parkinson’s disease was admitted for septic shock with hypotension and hypoxia. The patient had abdominal pain for one day before admission, and physical examination revealed generalized abdominal tenderness, rebound tenderness, and rigidity. On admission, the initial blood pressure was 53/34 mmHg, pulse rate was 77 beats per minute, and body temperature was 34.9℃ which was diagnostic of septic shock. Medical history revealed that the patient had undergone a Hartmann operation for stercoral perforation five years prior. Abdominopelvic computed tomography revealed a suspicious perforation in the sigmoid colon, proximal to the colostomy site (Fig. 1). In the operative field, typical findings of a stercoral perforation on the proximal part of the colostomy, such as a fecaloma and perforation on the antimesenteric side, were observed. We performed a segmental colon resection, including resection of the perforation site, followed by an end transverse colostomy. The patient died due to unrecovered septic shock the day after surgery.
An 87-year-old man with hypertension, osteoarthritis, and dementia was admitted to the authors' hospital with severe lower abdominal pain. The initial vital signs were as follows: blood pressure 160/97 mmHg, pulse rate, 92 beats per minute; and body temperature, 36.8℃. Physical examination revealed diffuse abdominal tenderness and rebound tenderness, particularly in the lower abdomen. Laboratory examination revealed a white blood cell count of 860 cells/mm3 suggesting leukocytopenia, a c-reactive protein of 0.65 mg/dL and a lactate level of 17.7 mg/dL. Two years ago, the patient underwent the Hartmann operation and reversal for a distal sigmoid colon perforation due to ischemic colitis. One year later, he underwent a second Hartmann operation for recurrent sigmoid colon perforation at another hospital. Abdominopelvic computed tomography on the third admission revealed a sigmoid colon perforation proximal to the previously built colostomy (Fig. 2). In the operative field, a 3 cm colon perforation was observed proximal to the colostomy, and colonic ischemia with fecal soiling was observed throughout the abdominal cavity. Segmental colon resection, including the perforation site and end transverse colostomy formation, was performed. The patient was discharged on the 17th postoperative day. During the 1-year follow-up period, the patient showed no recurrence of ischemic colitis.
Go to : 
Recurrent colonic perforation has rarely been reported, and only a few cases of colonic perforation after colostomy have been reported. Serpell et al. [1] reported two cases of recurrent stercoral colon perforation proximal to the end colostomy in the postoperative period after undergoing Hartmann procedure for stercoral perforation. Kim et al. [2] also reported two cases of stercoral perforation in the colon proximal to a sigmoid colostomy in patients who underwent abdominoperineal excision for rectal cancer. Gekas and Schuster [3] presented a case of stercoral perforation in a patient, following transverse-end colostomy for traumatic colon perforation. The first case in our report is consistent with a previous report based on operative findings showing fecaloma and antimesenteric side perforation. In the second case, perforation due to ischemic colitis was suspected because of the past history of a previous perforation of the sigmoid colon and the operative findings of ischemia of the colon wall. Recurrent colonic perforation resulting from ischemic colitis in patients with colostomy has not yet been reported.
As we performed the transverse colostomy following segmental colon resection, including the perforation site in the second case, there was no recurrence of ischemic colitis, though the follow-up period was short. Surgeons should consider the existence of points vulnerable to ischemic injury, such as Griffith's and Sudek's points, when deciding on the point of resection. Although some surgeons have suggested that the watershed zone is not especially vulnerable [4], we thought that the transverse colon would be more suitable as the stoma site in patients with recurrent colon perforation, especially in recurrent colonic ischemia.
In conclusion, surgeons should consider preventive strategies to reduce the risk of recurrent perforation in geriatric patients who have already undergone colostomy. Appropriate management of constipation, including laxatives, enemas, and a high-fiber diet, is important to prevent recurrent stercoral perforation [2]. In addition, in cases of recurrent perforation due to colonic ischemia, the transverse colon may be considered for the stoma site.
Go to : 
Author Contribution
Conceptualization: Kim HS
Formal Analysis: Kim H
Investigation: Kim H
Methodology: Noh GT
Project Administration: Kim KH
Writing – Original Draft: Kim H, Kim KH, Noh GT, Kim HS
Writing – Review & Editing: Kim H, Kim KH, Noh GT, Kim HS
Go to : 
References
1. Serpell JW, Sen M, Giddins G, Nicholls RJ, Bradfield WJ. Stercoral perforation of the colon proximal to an end colostomy. Postgrad Med J. 1991; 67((785)):299–300. DOI: 10.1136/pgmj.67.785.299. PMID: 2062783. PMCID: PMC2399011.

2. Kim YW, Kwon HJ, Kim IY. Stercoral perforation of the colon in sigmoid colostomy patients: two case reports. Int J Surg Case Rep. 2013; 4((11)):1038–1040. DOI: 10.1016/j.ijscr.2013.09.005. PMID: 24121050. PMCID: PMC3825961.

3. Gekas P, Schuster MM. Stercoral perforation of the colon: case report and review of the literature. Gastroenterology. 1981; 80((5)):1054–1058. DOI: 10.1016/0016-5085(81)90081-0. PMID: 7202964.

4. Carlson RM, Madoff RD. Is "ischemic" colitis ischemic? Dis Colon Rectum. 2011; 54((3)):370–373. DOI: 10.1007/DCR.0b013e31820481a9. PMID: 21304312.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download