INTRODUCTION
Hirschsprung disease (HD) is a congenital anomaly of the enteric nervous system causing intractable constipation which requires surgical correction. Following the first successful operation for HD [
1], several surgical techniques have been developed. Most patients with HD have favorable outcomes, although some experience long-term postoperative complications, including constipation, fecal incontinence, recurrent Hirschsprung-associated enterocolitis (HAEC), and failure to thrive (FTT) [
234]. Obstructive symptoms after a pull-through (PT) occur around 8%–30%, and the causes can be classified as anatomical, pathologic, and functional [
4]. Although conservative medical treatment or minor surgical intervention can improve these symptoms, some patients may require redo PT [
5]. Indications for redo PT surgery can include pathologic and/or anatomic factors. Anatomical problems can include anastomotic stricture, stenosis, obstructing Duhamel pouch, remnant septum, and obstructing Soave cuff, whereas pathologic problems include retained aganglionosis and transition zone pathology [
25]. Most of the anatomical problems are related to the initial PT procedure, which can be confirmed by rectal examination or contrast enema. In the absence of mechanical obstruction on rectal examination and contrast enema, a rectal biopsy should be performed to determine pathologic reasons [
4].
Several studies on redo PT surgery in HD patients have been previously published. However, the outcomes vary by report and long-term outcomes were scarce. Therefore, we aimed to evaluate the clinical outcomes of redo PT surgery in HD patients at a single center.
Go to :

METHODS
The medical records of patients who underwent redo PT for HD at a single tertiary center, between June 2003 and October 2019 were retrospectively reviewed. Data regarding clinical characteristics, pathologic results, initial surgical techniques, redo PT techniques, symptoms and indications for redo surgery, complications after redo PT, and follow-up clinical outcomes were collected. The study was approved by the Institutional Review Board of Asan Medical Center (No. 2020-0188). It was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
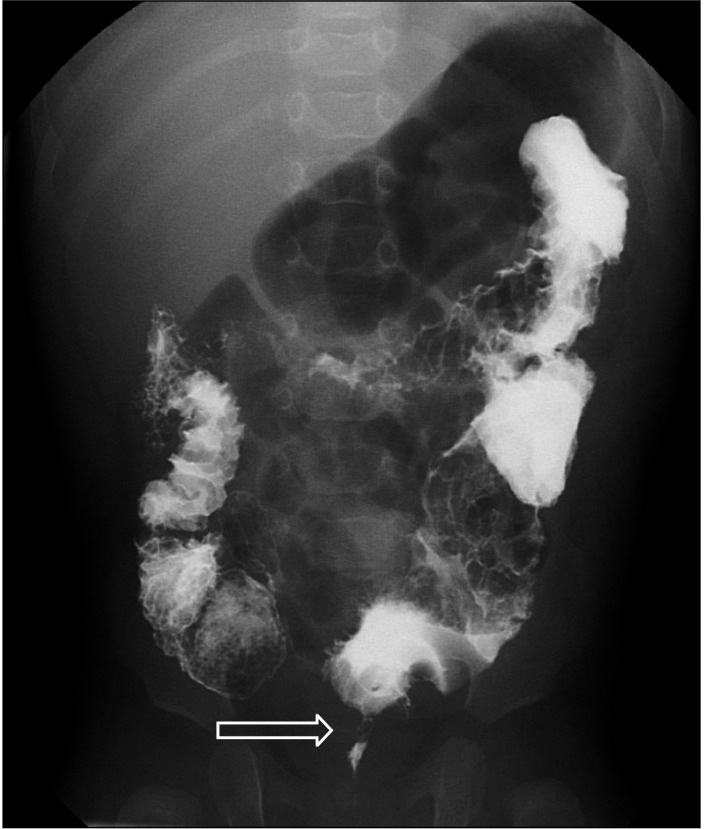
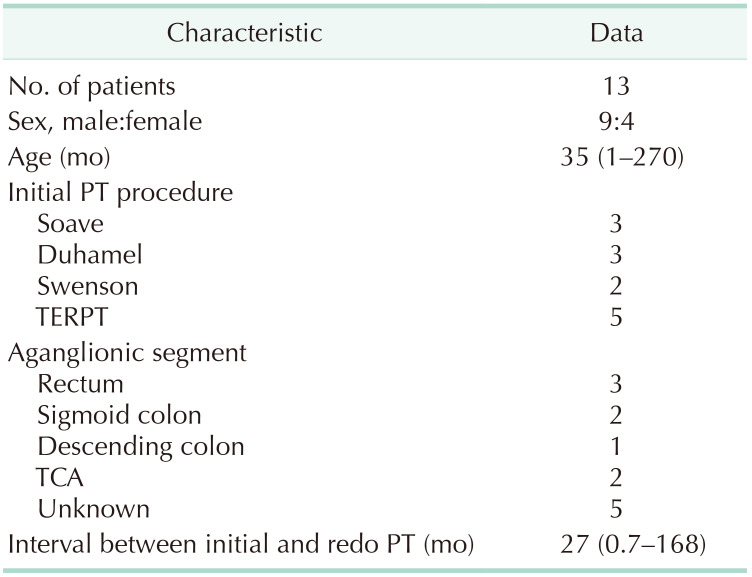
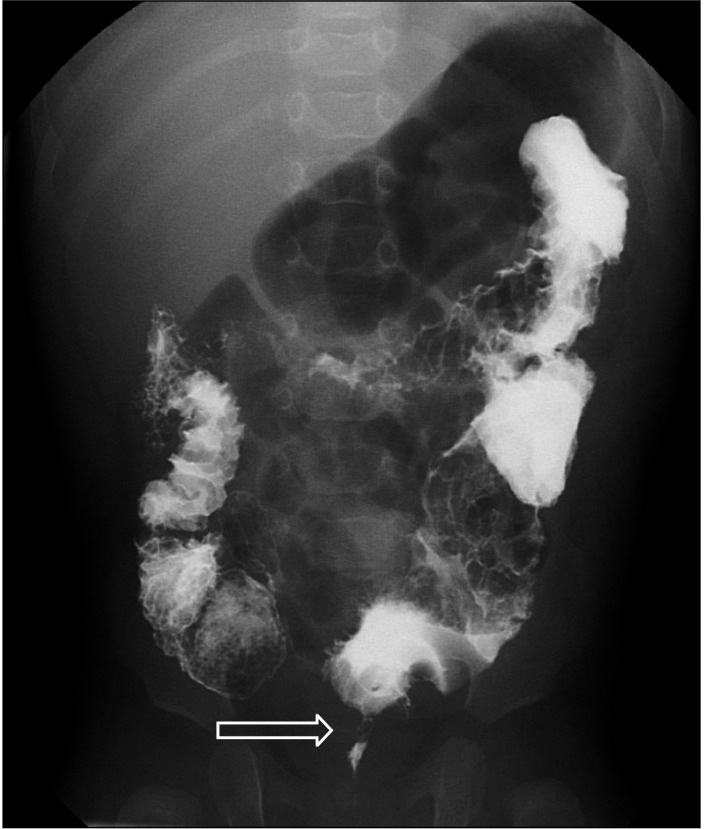
All redo PT procedures were performed by a single surgeon. Patients were included if they had postoperative obstructive symptoms after initial PT, including refractory constipation and episodes of enterocolitis or FTT. For work-up, contrast enema (
Figs. 1,
2) was done in every patient, except for those confirmed to have pathologic problems by biopsy.
 | Fig. 1Contrast enema of a patient who had a Duhamel procedure. The enlarged Duhamel pouch was causing obstructive symptoms.
|
 | Fig. 2Contrast enema of a patient with retained aganglionosis after transanal endorectal pull-through. The arrow shows the transition zone.
|
The surgical technique for redo PT was determined by the surgeon according to the patient’s state. Posterior sagittal approach was performed in 1 patient in 2003 and transanal endorectal PT (TERPT), which has a similar basic procedure to the Soave procedure, was performed thereafter [
6]. TERPT underwent in lithotomy position, and laparoscopy was performed for the mobilization of the colon if necessary.
Go to :

RESULTS
Demographics
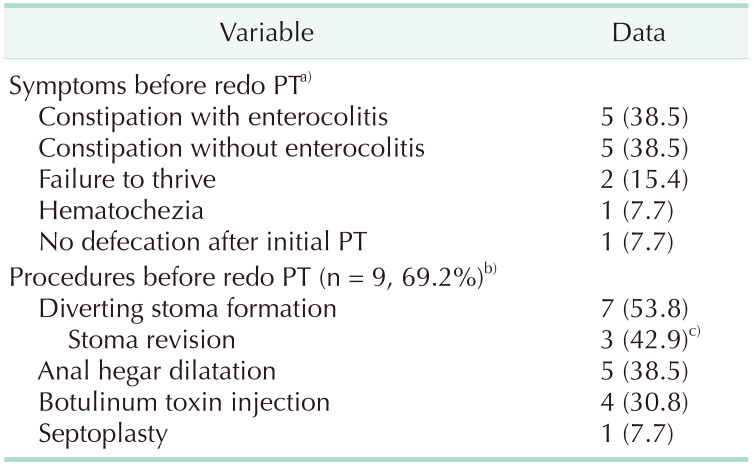
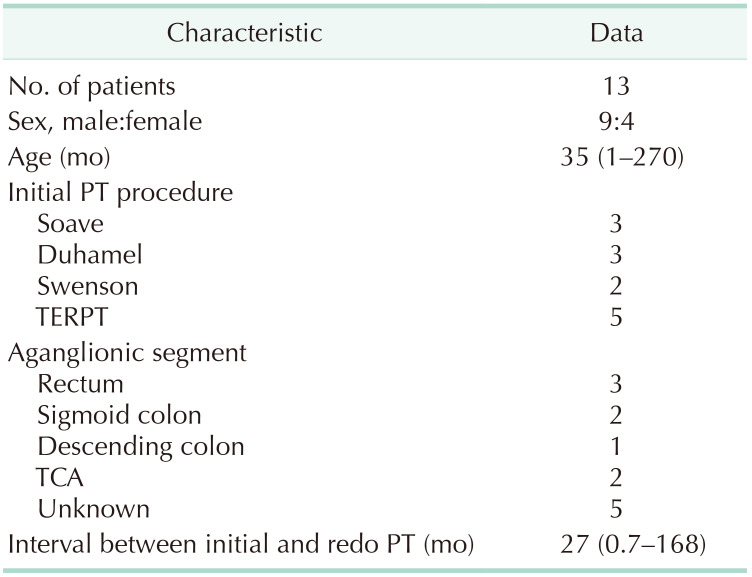
During the study period, 187 patients underwent PT procedure for HD at Asan Medical Center, 13 of which were redo PT. The 13 patients included 9 boys and 4 girls, with median age of 35 months (range, 1–270 months) at the time of redo PT. The median interval between primary and redo PT was 27 months (range, 18 days–168 months). Eight of the patients had primary PT at initial surgery, whereas 5 underwent staged operations. Five patients underwent initial PT at our center and 8 at another center. Initial PT procedures included the Soave procedure in 3 patients, the Duhamel procedure in 3, the Swenson procedure in 2, and TERPT in 5.
At the time of initial PT, aganglionic segments were in the rectum of 3 patients (23.1%), the sigmoid colon in 2 (15.4%), and the descending colon in 1 (7.7%), with 2 patients (15.4%) having total colonic aganglionosis (TCA). The transition zone in 5 patients (38.5%) was not documented (
Table 1).
Table 1
Demographics and clinical characteristics of patients included in this study

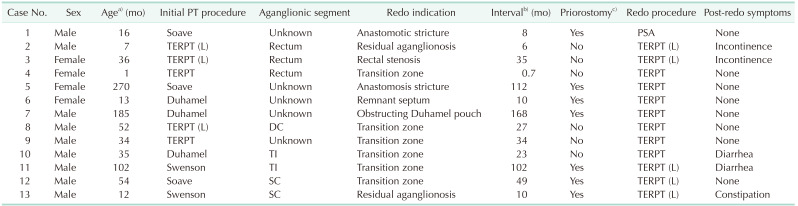
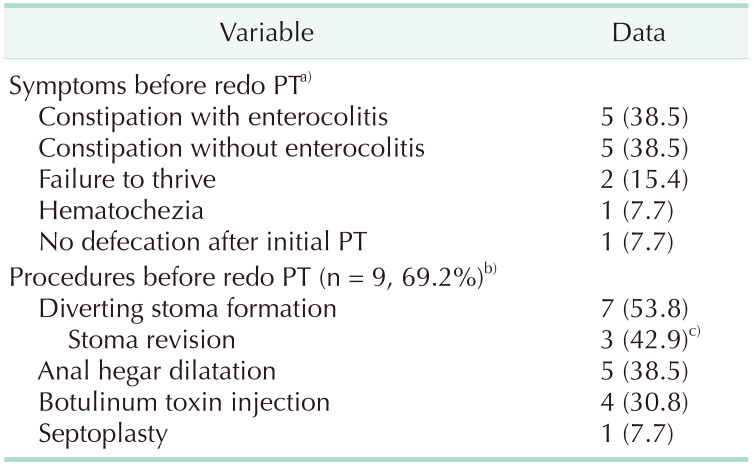
Assessments and procedures prior to redo pull-through
Ten patients (76.9%) presented with constipation, including 5 with (38.5%) and 5 without (38.5%) episodes of enterocolitis. Other presenting symptoms included FTT in 2 patients (15.4%), hematochezia in 1 (7.7%), and absence of defecation after initial PT in 1 (7.7%). One patient who presented constipation with recurrent enterocolitis also showed FTT (
Table 2).
Table 2
Symptoms and procedures prior to redo pull-through (PT)

Seven patients (53.8%) underwent diverting ileostomy formation in our center prior to redo PT to alleviate obstructive symptoms during the preoperative evaluation period. All of them received initial PT at other institutions and were referred to our institution. Three patients who underwent stoma formation had to undergo additional stoma revision due to stoma-related complications, including prolapse in 2 (66.7%) and retraction in 1 (33.3%).
Nine patients (69.2%) underwent other treatment interventions to resolve obstructive symptoms such as constipation, enterocolitis, or FTT before redo PT, including anal dilation, botulinum toxin injection, or septoplasty for remnant septum, but these procedures were not successful (
Table 2). For the 4 patients with suspected spasms of the anal sphincters, 5 mg/kg of botulinum toxin was injected between external anal sphincter and internal anal sphincter in 4 divided doses around the anal opening as in the previously published protocol [
7]. However, 3 of 4 were found to have transition zone pathology, and an additional patient was found to have anastomotic stricture.
A patient who underwent the Duhamel procedure at another institution showed anastomotic stricture on contrast enema, and during examination under anesthesia, the remaining septum of the anastomosis area was confirmed. Septoplasty was performed via laparotomy sequentially. The anterior wall of original rectum was incised and the remaining septum was removed, but it was ineffective.
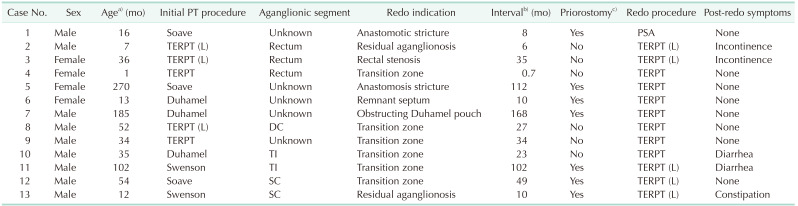
Case 10 in
Table 3 is 1 of the 2 patients diagnosed with TCA who underwent the Duhamel procedure for initial PT in our institution but subsequently experienced constant constipation and recurrent enterocolitis. Case 11 in
Table 3 is the other patient diagnosed with TCA who underwent the Swenson procedure at another institution and was referred to our hospital with uncontrolled diarrhea and intermittent hematochezia. This patient was suspected of sphincter muscle impairment during examination under anesthesia and had severe skin erosion around the anus, thus underwent diverting ileostomy prior to redo PT.
Table 3
Summary of patients in this study who underwent redo pull-through (PT)

Redo pull-through: indications and surgical techniques
Indications for redo PT in the 13 patients included pathologic problems in 8 (61.5%), stricture in 2 (15.4%), and rectal stenosis, obstructing Duhamel pouch, and remnant septum in 1 each (7.7%). Of the 8 patients with pathologic problems, 2 had retained aganglionosis and 6 had transition zone pathology. Of the 13 redo PT operations, 12 (92.3%) were TERPT, including 5 with laparoscopy assisted, and 1 (7.7%) was performed via the posterior sagittal approach (
Table 3).
Postoperative clinical outcomes
Two patients (15.4%) experienced early complications including postoperative ileus and a ureter injury during redo PT procedure due to severe adhesion. Five of the 7 patients who had a diverting stoma prior to redo PT performed stoma closure 4 to 6 months after redo PT, and the other 2 had stoma closure concurrently. None of the patients experienced anastomotic complications including leakage, abscess, or perforation.
After a median follow-up period of 68 months (range, 3–227 months), 8 patients (61.5%) had voluntary bowel movements, 1 (7.7%) needed laxatives for constipation, and 2 (15.4%) were incontinent. One patient with fecal incontinence showed spontaneous improvement of symptoms at the age of 7 years, which was 69 months after surgery. The patient with TCA who underwent the Duhamel procedure for primary PT and underwent redo TERPT was monitored by a pediatric gastroenterologist in the outpatient clinic due to recurrent ileitis with constant diarrhea. The other TCA patient with suspected sphincter muscle impairment underwent laparoscopic-assisted redo TERPT due to transition zone pathology. However, since the diarrhea was not alleviated, this patient underwent permanent ileostomy formation 20 months after the redo PT procedure (
Table 3).
Go to :

DISCUSSION
Although surgery is usually successful in patients with HD, some patients experience postoperative morbidities, including constipation, fecal incontinence, and enterocolitis [
234]. Improvements are often provided by medical treatment or minor surgical interventions, but some patients may require redo PT [
5]. The present study evaluated long-term clinical outcomes in patients who underwent redo PT for various indications, with all procedures performed by a single surgeon.
Of the 13 cases requiring redo PT during the study period, 8 (61.5%) did so for pathologic issues, as confirmed by examination of the removed tissue specimens. Pathologic problem is usually caused by a pathologist’s incorrect assessment of presence or absence of ganglion cells on frozen section of specimen, or by a surgeon’s technical failure not going far enough above the pathological transition zone [
4]. Three patients underwent redo PT based on biopsy results without contrast enema. Case 4 in
Table 3 had regular ganglion cells in the frozen biopsy specimen during initial PT. However, the patient had no stool passage after the surgery, and the final pathology report indicates that, with a few ganglion cells present, this patient underwent redo PT 18 days after the initial PT. Case 8 in
Table 3, who suffered from refractory constipation, was found to have a decrease in ganglion cell density only upon reassessment of the pathology slides 26 months after initial PT; this patient underwent redo PT without re-biopsy during the work-up period. Two sequential rectal biopsies of case 2 in
Table 3 with recurrent enterocolitis and FTT after initial PT confirmed that the bowel was normally ganglionated. Contrast enema of this patient showed functional obstruction, for which this patient underwent redo PT, and examination of the final specimen showed transition zone pathology. These cases indicate the importance of the evaluation of adequate and sufficient specimens by experienced and reliable pathologists [
8].
Two patients (15.4%) experienced early complications within 30 days after redo PT. One patient experienced postoperative ileus, which improved after conservative management, whereas the other experienced a ureter injury during redo PT due to severe adhesion, with this patient later requiring an additional ureteroureterostomy. None of the patients experienced an anastomotic leak, abscess, or perforation. This incidence was lower than in previous studies [
910], which regarded preoperative stoma formation as advantageous. All 7 patients who underwent diverting ostomy formation prior to redo PT were referred from other institutions after initial PT. Since obstructive symptoms such as refractory constipation or HAEC were severe in patients who were referred from other institutions, diverting ostomy was performed to prevent obstructive symptoms during preoperative evaluation period. Five of the 6 patients who did not undergo stoma formation prior to redo PT had undergone initial PT at our institution, with initial PT in the sixth performed by a pediatric surgeon trained in our center. The absence of detailed medical records made it difficult to perform redo PT shortly after initial PT. Diverting ostomy formation prior to redo PT may be a safe option, enabling preoperative work-up with sufficient time to prevent the recurrence of obstructive symptoms. In addition, early complications after redo PT can be reduced by delayed stoma closure [
11]. However, 42.9% of the patients with diverting ostomy in this study and 28% of pediatric patients with colostomy in a previous study had stoma-related complications [
12], suggesting the need for careful patient selection.
Three patients (23.1%) experienced incontinence after redo surgery, with 1 showing symptom improvement during follow-up, an incidence lower than in previous studies [
210]. It is important to preserve the anal canal during PT procedures [
413], as the low incidence of incontinence in this study appears to be due to careful preservation of the dentate line throughout the procedure.
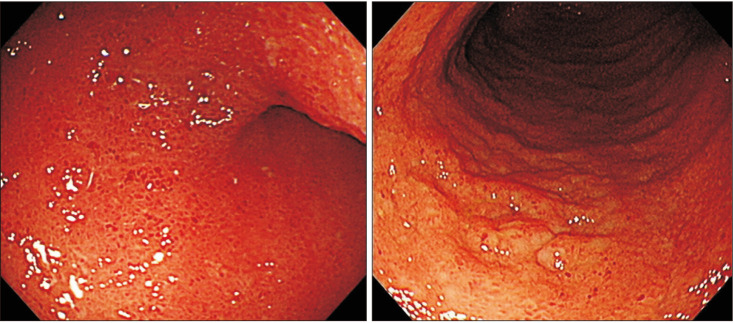
Two patients (15.4%) diagnosed with TCA reported recurrent diarrhea after redo PT. One of these patients (case 10 in
Table 3), who underwent redo PT for transition zone pathology, was diagnosed by a pediatric gastroenterologist with chronic active ileitis and possibility of Crohn disease (
Fig. 3). This patient is currently on medication for Crohn disease and has been showing improvement in symptoms since. A meta-analysis reported that, of HD patients who developed inflammatory bowel disease (IBD) after PT operation, 41% had TCA and 45% showed aganglionic involvement of the long segment [
14]. The possibility of IBD should be considered in patients with extensive colonic aganglionosis if uncontrolled diarrhea persists after successful PT operation. The other TCA patient (case 11 in
Table 3) with suspected sphincter muscle impairment eventually required a permanent ileostomy due to repeated diarrhea after redo PT. This patient was also diagnosed with chronic ileitis by the same gastroenterologist and received medical treatment, but symptoms did not improve. Findings in this patient once again indicate the importance of preserving the anal canal during initial PT [
413].
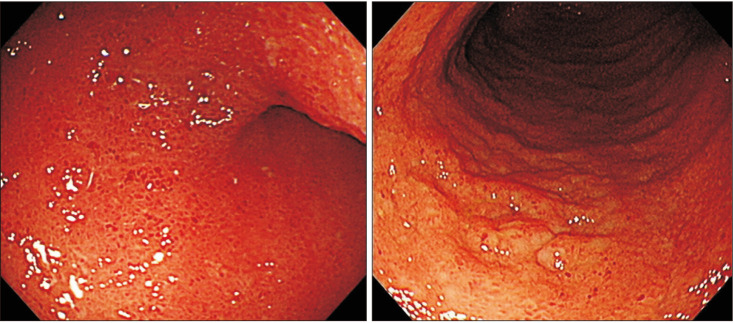 | Fig. 3Endoscopic findings of a patient with total colonic aganglionosis after redo pull-through showing hyperemic mucosa with aphthous ulcers. Endoscopic biopsy reported chronic active ileitis with dense lymphoplasmacytic infiltration in lamina propria and cryptitis.
|
The strengths of this study were its relatively long-term follow-up period after redo PT and that all operations were performed by a single expert surgeon, which makes all surgeries comparable by similar surgical skill. However, the present study had several limitations. Firstly, its retrospective design can lead to selection bias and 5 patients referred from other centers might not include sufficient data. Secondly, it has wide variability and heterogeneity of the patient population including initial length of aganglionosis, type of primary PT, highly variable patient age, highly variable interval between initial and redo surgery, and the presenting symptoms leading to redo PT. Thirdly, included number of patients is too small to reach any conclusions, though we attempted to show long-term follow-up results of redo PT.
In conclusion, redo PT procedures could be effective approach for improving obstructive symptoms in HD patients with anatomic or pathologic reasons following primary PT. Careful selection of patients and discreet indications for redo PT are crucial.
Go to :





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download