Abstract
Purpose
The number of elderly patients, especially aged ≥80 years, undergoing emergency surgery is gradually increasing. The aim of this study was to find out the trends and results of emergency general surgery for elderly patients over 9 years in an emergency medical center in South Korea, where the population is aging most rapidly.
Methods
The clinical characteristics, outcomes, and medical expenses of emergency general surgery for the elderly (aged 65–79 years) and highly elderly (aged ≥80 years) patients who visited to a regional emergency medical center from 2012 to 2020 were analyzed.
Results
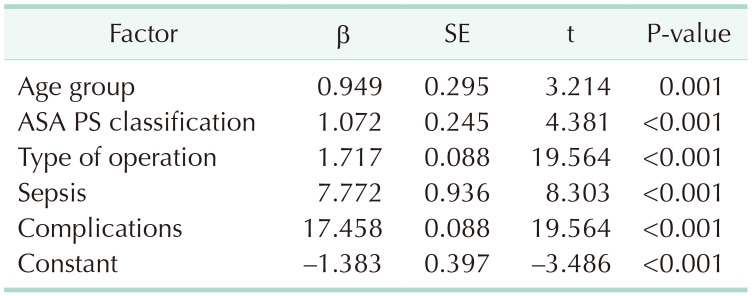
The number of highly elderly patients increased with each 3-year interval, whereas the proportion of patients aged 19–79 years was similar, and that of pediatric patients was decreasing. The higher the age group, the higher the mortality (young adult vs. elderly vs. highly elderly: odds ratio [OR], 1 vs. 3.689 vs. 11.293; P < 0.001) and complication rates (OR, 1 vs. 2.840 vs. 4.633; P < 0.001), and longer length of hospital stay (β = 0.949, P = 0.001) even after adjusting for the type of surgery and the American Society of Anesthesiologists physical status classification. Non-covered medical expenses were significantly related to the age groups (β = 151,608.802, P < 0.001).
South Korea has a rapidly aging population. The pace of entry into an aging society, which is defined as the proportion of the population aged >65 years at >14%, has been faster than that of Japan, and it is expected to enter a super-aged society, with >20% of the population aged >65 years, by 2025 [1]. Since elderly patients exhibit a high rate of emergency surgery [23], the number of elderly patients undergoing emergency general surgery (EGS) in Korea is presumed to be also increasing. EGS is associated with high complication and mortality rates and medical costs in elderly patients [456]. In addition, EGS data in Korea, where the super-aged population is rapidly increasing, will suggest what other aging societies need to prepare for in the field of social health care system. Hence, we attempted to analyze the tendency and outcome of EGS in highly elderly patients compared to young adults and elderly patients using long-term patient data obtained from a hospital designated as a regional emergency medical center.
This study was approved by the Institutional Review Board of the Myongji Hospital, and the requirement for obtaining written informed consent was waived owing to the retrospective study design (No. 2022-09-026).
Data were collected prospectively from the electronic medical records of patients who visited the emergency medical center and underwent general surgery within 24 hours of hospital admission, between January 1, 2012 and December 31, 2020. Patient characteristics, including age, sex, date of visit to the emergency medical center, date of operation, length of hospital stay, pre- and postoperative diagnoses, name of surgery, underlying diseases, the American Society of Anesthesiologists (ASA) physical status classification, postoperative complications, results of treatment (recovery or improvement, no improvement, death within 48 hours, death after 48 hours), and medical expenses, such as total, covered, and non-covered medical expenses, were obtained. Patients with trauma and surgeries under local or regional anesthesia, such as anal and subcutaneous abscesses, were excluded from the analysis.
For the underlying disease, only the ASA PS classification was used because the grade of the patients’ medical status before surgery was needed for analysis rather than each disease, and the results of treatment data were converted into mortality and used. In this study, complication was defined as any deviation from the normal postoperative course, and the presence or absence was used in the analysis. Perioperative sepsis or septic shock was considered to be attributable to the preoperative condition and excluded from complications, and these data were separately used for analysis.
Patients aged 0–18 years were classified as children, 19–64 years as young adults, 65–79 years as elderly, and ≥80 years as highly elderly. These patients were further classified by period: (1) 2012–2014, (2) 2015–2017, and (3) 2018–2020. This period division was based on the years 2012 and 2015 because our institution was designated as the regional emergency medical center in northwestern Gyeonggi province on June 30, 2011, and as a severe trauma center on October 20, 2014. Altogether, 4208 patients visited the emergency medical center and underwent general surgical operations from 2012 to 2020. After excluding pediatric patients, patients whose ASA PS classification was not recorded by an anesthesiologist during surgery, and patients with missing total medical cost data, 2,733 patients were included in the study (Table 1). In the subgroup analysis, total 643 patients were included, excluding appendectomy (OP 1) and cholecystectomy (OP 2) patients (Supplementary Table 1).
The surgical classification was modified as follows, such that with an increase in the severity, the coding number also increased, based on a report by Scott et al. [7], which classified and defined EGS in the United States: (1) appendectomy; (2) cholecystectomy; (3) adhesiolysis, including hernia surgery without bowel resection; (4) small bowel segmental resection, including hernia surgery with bowel resection; (5) simple closure of peptic ulcer perforation; (6) colon resection; and (7) others including Hartmann’s operation, gastrectomy, and any surgery that could not be classified in more detail, such as diagnostic laparotomy. Patients who died postoperatively (n = 42) were excluded when analyzing the following parameters to avoid errors due to fewer complications, fewer hospital stays, and lower medical costs. In addition, patients who did not have medical insurance (n = 20) were also excluded from the analysis when analyzing covered and non-covered medical costs separately.
Continuous variables are expressed as mean ± standard deviation and categorical variables as numbers (%). The analysis of variance (ANOVA) was used for the average comparison among groups, and the chi-square test was used for the ratio comparison. The post hoc analyses for ANOVA results were performed using Dunnett T3 test because the assumption of equal variance among 3 groups was not satisfied by the Welch test. The analysis, in the presence or absence of complications or death, was performed by logistic regression, and the cost and length of hospital stay after surgery were analyzed by multivariable regression. All analyses were performed using IBM SPSS Statistics ver. 24.0 (IBM Corp.). Statistical significance was set at P < 0.05.
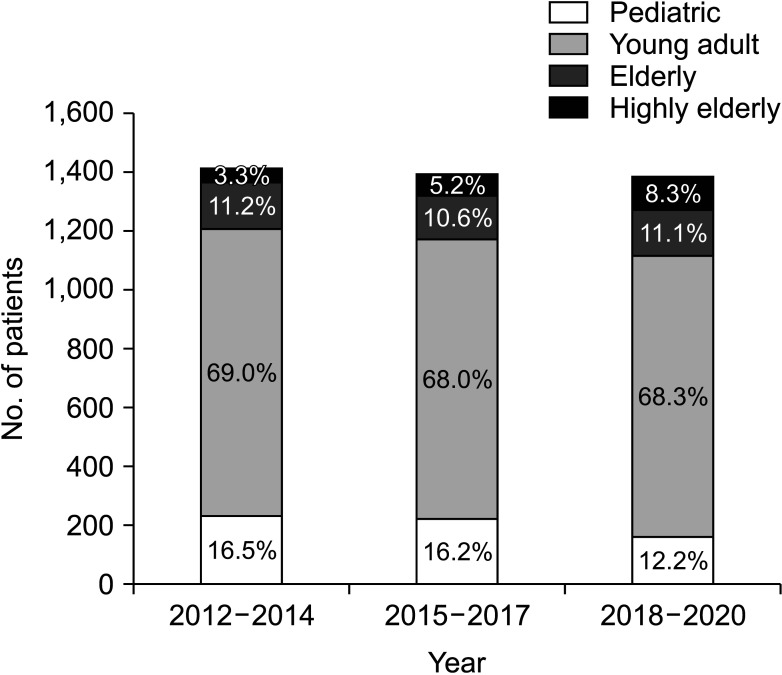
On dividing this period into 3-year intervals, the ratio of hospital admission in adult (19–64 years) to elderly patients (65–79 years) was similar. In the last 3 years, the proportion of hospital admissions in children progressively decreased compared to the past (16.5%, 16.2%, and 12.2%, respectively), whereas this proportion progressively increased in highly elderly patients (≥80 years; 3.3%, 5.2%, and 8.3%, respectively). This difference was statistically significant (P < 0.001) (Fig. 1).
The higher the age group, the lower the percentage of males (58.6%, 48.3%, and 37.6%, respectively; P < 0.001), and the higher proportion of patients with ASA PS classification of ≥III (6.2%, 33.8%, and 48.6%, respectively; P < 0.001). The elderly than younger adults, and the highly elderly than elderly showed a significant increase in the proportion of EGS with high severity, and the intensive care unit (ICU) admission rate, postoperative complication rate, mortality rate, postoperative length of hospital stay, and total medical costs all deteriorated. This trend was also confirmed in the post hoc analysis of the ANOVA results of length of hospital stay (younger adult vs. elderly, P < 0.001; younger adult vs. highly elderly, P < 0.001; and elderly vs. highly elderly, P = 0.025) and total medical cost (younger adult vs. elderly, P < 0.001; younger adult vs. highly elderly, P < 0.001; and elderly vs. highly elderly, P = 0.005).
The factors that significantly affected in-hospital mortality after EGS were the type of surgery, sepsis, ASA PS classification, complications and age group according to the multivariable logistic regression analysis. After adjusting for other factors, the odds of death were 3.689 (95% confidence interval [CI], 1.066–12.769) times higher in the elderly and 11.293 (95% CI, 3.506–36.379) times higher in the highly elderly than in young adults (P < 0.001) (Table 2).
Factors associated with occurrence of postoperative complication were also analyzed using logistic regression analysis for 2,691 patients after excluding deceased patients (n = 42). The type of surgery, sepsis, ASA PS classification and age group were significant factors. The odds ratio of postoperative complications were 2.840 (95% CI, 1.646–4.901) and 4.633 (95% CI, 2.623–8.183) times higher in elderly and highly elderly patients, respectively, than in young adults (P < 0.001) after adjusting for the effects of other factors (Table 3).
The type of surgery, sepsis, complications, ASA PS classification, and age group were significant factors according to multivariable regression analysis performed on the postoperative length of hospital stay of patients excluding the deceased patients (Table 4). When other significant factors were at the same level, the higher age group was related to a longer postoperative hospital stay (β = 0.949, standard error [SE] = 0.295, P = 0.001).
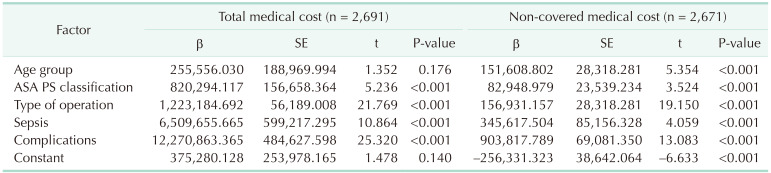
The influence of these factors on medical costs was analyzed via a multivariable regression analysis (Table 5). The type of surgery, sepsis, ASA PS classification, complications, and age group were used as independent variables to analyze the total, covered, and non-covered medical expenses. When the effects of other factors were adjusted, no difference was observed between the age groups for total and covered medical costs; however, it was found that the non-covered medical costs significantly increased as the age group increased (β = 151,608.802, SE = 28,318.281, P < 0.001).
The effect of age group on mortality, complication, postoperative length of hospital stay, and medical cost was analyzed in a subgroup analysis with the same methods as in the entire cohort, excluding appendectomy and cholecystectomy cases which have relatively good surgical outcomes and can be replaced with conservative treatment if possible. The results of subgroup analysis also showed that the elderly than younger adults, and highly elderly than the elderly presented higher mortality and complication after surgery, longer length of hospital stay, and significantly higher non-covered medical costs (Supplementary Tables 2, 3, 4, 5).
In this study, we retrospectively analyzed prospectively collected EGS data for the last 9 years at 1 of the 7 regional emergency medical centers in Gyeonggi province, where approximately 26% of the Korean population resides. The authors found that the number of EGS for the highly elderly population is increasing, and the mortality and complication rates after surgery were the highest among that age group. In addition, it was found that the age group itself was a significant factor that increased postoperative length of hospital stay and the non-covered medical cost, even after the underlying disease status as reflected by the ASA PS classification or the type of surgery was adjusted.
In the last 3 years, the proportion of hospital admissions among children had progressively decreased compared to the past (16.5%, 16.2%, and 12.2%, respectively), whereas this proportion increased in patients aged ≥80 years (3.3%, 5.2%, 8.3%, respectively), which was similar to the change in the overall Korean population structure. According to the demographic data of registered residents from the Ministry of Public Administration and Security, the proportion of children aged ≤19 years gradually decreased from 21.2% to 19.4% to 17.6% of the total population during the first, second, and third 3-year intervals, respectively, and this proportion increased for highly elderly patients from 2.3% to 2.9% to 3.6%, respectively [8]. These details show that although this study was conducted in a single institution, it reflects the changing patterns of the entire Korean population to some extent.
According to a systematic review on emergency abdominal surgery for patients aged >65 years from 1994 to 2013, emergency surgery in elderly patients showed higher mortality rates than emergency surgery in young adults and scheduled surgery in elderly patients [9]. Ingraham et al. [10] analyzed 68,003 emergency surgical procedures registered with the National Surgical Quality Improvement Program (NSQIP) in 2005–2008 and reported that patients aged ≥65 years had a 1.17 times (95% CI, 1.10–1.24) higher risk of serious complications and a 2.29 times (95% CI, 2.09–2.51) higher risk of death than young adults. However, our study is meaningful in that there are not many studies that have confirmed the difference between the elderly and the super-aged, not only in mortality but also in other outcomes such as complications, hospital days, and medical costs.
The elderly and highly elderly patients, compared to adults aged ≤64 years, exhibited more unfavorable outcomes, including higher ICU admission, complication, in-hospital mortality rates, postoperative length of hospital stay, and total medical costs in this study. Even after adjusting for the type of surgery and ASA PS classification that can affect postoperative outcomes, the age group had a significant effect on the incidence of complications, mortality, and length of postoperative hospital stay.
These effects of age groups on postoperative outcomes were also found to be the same in subgroup analysis conducted after removing appendectomy and cholecystectomy cases. The reason for performing subgroup analysis was that these surgeries can have relatively good postoperative results compared to other EGSs, and depending on the situation, they can be avoided with conservative treatment in some clinical situations. Therefore, it was intended to confirm whether the results obtained in all cohorts were solid except for these surgeries. Actually, a United States study of 149,855 patients hospitalized for cholecystectomy between 1999 and 2006 found that the higher the age group, the higher the mortality rate, complications, hospital days, and medical costs [4]. On the other hand, in a Korean study of patients who received laparoscopic cholecystectomy between 2011 and 2013, patients aged 80 years or older only presented longer postoperative length of stay, but there was no difference in mortality or complications, which was analyzed because the rate of percutaneous transhepatic gall bladder drainage before surgery was significantly high in that age group [11].
We used the ASA PS classification as data on patients’ basic conditions and used it for adjustment; however, the NSQIP score and physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM) are known to be more accurate for predicting the prognosis of surgical patients [12]. In addition, it has recently been reported that variables such as frailty and sarcopenia are more accurate in predicting the prognosis of these patients as compared to the existing grading and prediction systems. The significance of age also reportedly becomes insignificant in the outcome of EGS patients when multivariable analysis is performed, including these variables [1314]. This study showed that the older age group demonstrated worse complication and mortality rates in EGS, but it was not explained whether the reason was the age group itself or whether these results were caused by other factors such as frailty that the elderly generally have.
There have been reports that medical expenses increase in the elderly or patients with high frailty after EGS during the period of hospitalization or up to 1 year after discharge [1516]. Also in our data, even when the type of the surgery, the condition of the underlying disease, and even the complication occurrence status were the same, the older the age, the higher the medical expenses. In particular, the uniqueness of our study results is that age was not a factor for the covered medical expenses but was a significant factor only for non-covered medical expenses. In South Korea, the medical insurance system has been applied to the entire nation since 1989. Each medical institution submits data on medical expenses to the Health Insurance Review and Assessment (HIRA) service; then, the HIRA charges medical expenses to the national health insurance and pays each institution [17]. More medical resources were consumed by the variables adjusted during the analysis, such as the type of the surgery and underlying disease status reflected by ASA PS classification . However, non-covered medical expenses increased with increasing age group, even after adjustment. One possible explanation is that drugs or treatments might have been prescribed according to physician experience or clinical preference in emergency or critical situations to improve outcomes of elderly patients, even if immediate effectiveness or indication was not evident. Since this is the first report an increase in non-covered medical expenses for the elderly undergoing EGS was observed, further research and analysis of the causes for this result are warranted.
Although our study showed the results of EGS for the elderly and highly elderly in Korea, it has several limitations. First, it is a retrospective study based on single-center data; this interferes with the generalization of our results. However, a study period of 9 years with the data source as the regional emergency center that conducts emergency surgeries in a metropolitan area of Korea makes this study a relevant addition to the existing literature. Second, since the data were retrospectively obtained from the insurance claim data of the institution, complications may have been less accurate than those in the medical record analysis. However, as hospitals must record complications and diagnostic codes to ensure proper compensation by the National Health Insurance Corporation, most complications with significant costs were likely included. Finally, the ASA PS classification was used as a variable to correct the risk of underlying disease. However, if the analysis was performed with consideration of the data on indicators, which more accurately reflect the patient’s preoperative risk, such as NSQIP score and frailty, the results would have improved reliably. However, it is difficult to obtain accurate and consistent data from elderly patients undergoing emergency surgery who require prompt treatment.
In conclusion, the number of elderly and highly elderly patients undergoing EGS is increasing in Korea, which has led to high complication and mortality rates accompanied by increased medical expenses. Therefore, continuous research on medical and institutional improvements is required to reduce the social burden while improving prevention and treatment outcomes in emergency surgery for the elderly population.
References
1. Baek JY, Lee E, Jung HW, Jang IY. Geriatrics fact sheet in Korea 2021. Ann Geriatr Med Res. 2021; 25:65–71. PMID: 34187140.
2. Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003; 238:170–177. PMID: 12894008.
3. Ukkonen M, Jämsen E, Zeitlin R, Pauniaho SL. Emergency department visits in older patients: a population-based survey. BMC Emerg Med. 2019; 19:20. PMID: 30813898.
4. Kuy S, Sosa JA, Roman SA, Desai R, Rosenthal RA. Age matters: a study of clinical and economic outcomes following cholecystectomy in elderly Americans. Am J Surg. 2011; 201:789–796. PMID: 21741511.
5. Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, et al. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015; 78:306–311. PMID: 25757115.
6. Hadaya J, Sanaiha Y, Juillard C, Benharash P. Impact of frailty on clinical outcomes and resource use following emergency general surgery in the United States. PLoS One. 2021; 16:e0255122. PMID: 34297772.
7. Scott JW, Olufajo OA, Brat GA, Rose JA, Zogg CK, Haider AH, et al. Use of national burden to define operative emergency general surgery. JAMA Surg. 2016; 151:e160480. PMID: 27120712.
8. Ministry of the Interior and Safety (MOIS), Republic of Korea. Population status by age [Internet]. MOIS;2022. cited 2022 Jun 10. Available from: https://jumin.mois.go.kr/ageStatMonth.do
.
9. Cooper Z, Scott JW, Rosenthal RA, Mitchell SL. Emergency major abdominal surgical procedures in older adults: a systematic review of mortality and functional outcomes. J Am Geriatr Soc. 2015; 63:2563–2571. PMID: 26592523.
10. Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Variation in quality of care after emergency general surgery procedures in the elderly. J Am Coll Surg. 2011; 212:1039–1048. PMID: 21620289.
11. Lee SI, Na BG, Yoo YS, Mun SP, Choi NK. Clinical outcome for laparoscopic cholecystectomy in extremely elderly patients. Ann Surg Treat Res. 2015; 88:145–151. PMID: 25741494.
12. Havens JM, Columbus AB, Seshadri AJ, Brown CV, Tominaga GT, Mowery NT, et al. Risk stratification tools in emergency general surgery. Trauma Surg Acute Care Open. 2018; 3:e000160. PMID: 29766138.
13. Chua MS, Chan DK. Increased morbidity and mortality of emergency laparotomy in elderly patients. World J Surg. 2020; 44:711–720. PMID: 31646368.
14. Joseph B, Zangbar B, Pandit V, Fain M, Mohler MJ, Kulvatunyou N, et al. Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg. 2016; 222:805–813. PMID: 27113515.
15. Eamer GJ, Clement F, Pederson JL, Churchill TA, Khadaroo RG. Analysis of postdischarge costs following emergent general surgery in elderly patients. Can J Surg. 2018; 61:19–27. PMID: 29368673.
16. McIsaac DI, Taljaard M, Bryson GL, Beaulé PE, Gagné S, Hamilton G, et al. Frailty as a predictor of death or new disability after surgery: a prospective cohort study. Ann Surg. 2020; 271:283–289. PMID: 30048320.
17. Song YJ. The South Korean health care system. JMAJ. 2009; 52:206–209.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1–5 can be found via https://doi.org/10.4174/astr.2023.104.6.325.
Supplementary Table 1
Basic clinical characteristics presented according to the age-groups after excluding appendectomy and cholecystectomy cases
Supplementary Table 2
Analysis of possible factors affecting postoperative in-hospital mortality after excluding appendectomy and cholecystectomy cases
Supplementary Table 3
Analysis of possible factors affecting postoperative complication occurrence after excluding appendectomy and cholecystectomy cases
Supplementary Table 4
Effect of possible factors for postoperative length of hospital stay after excluding appendectomy and cholecystectomy cases (n = 603)
Supplementary Table 5
Effect of possible factors for medical costs after excluding appendectomy and cholecystectomy cases
Table 2
Analysis of possible factors affecting postoperative in-hospital mortality
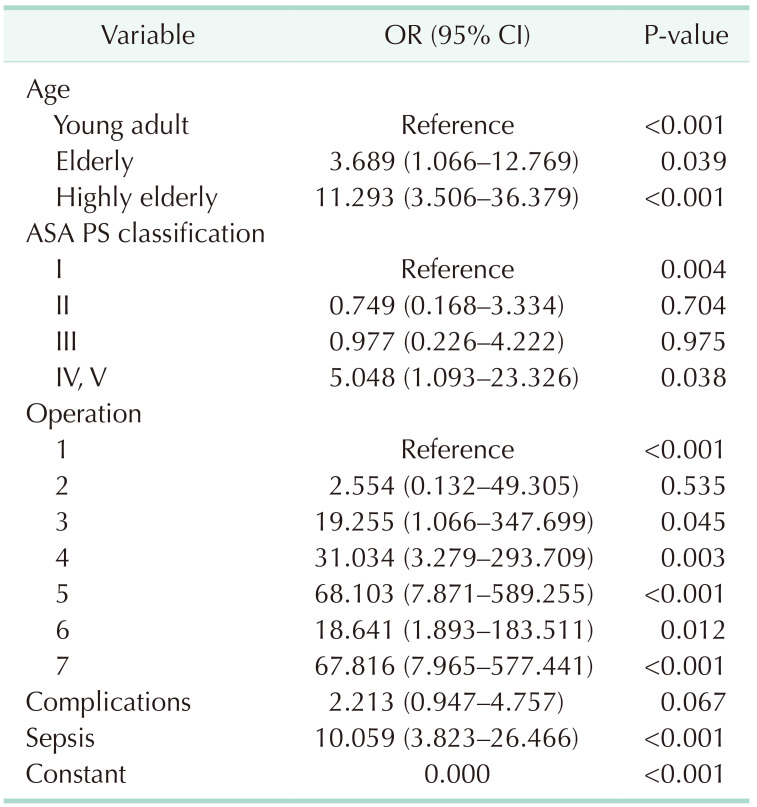
OR, odds ratio; CI, confidence interval; ASA PS, American Society of Anesthesiologists physical status.
Operation 1–7, same as described in Table 1.
Table 3
Analysis of possible factors affecting postoperative complication occurrence
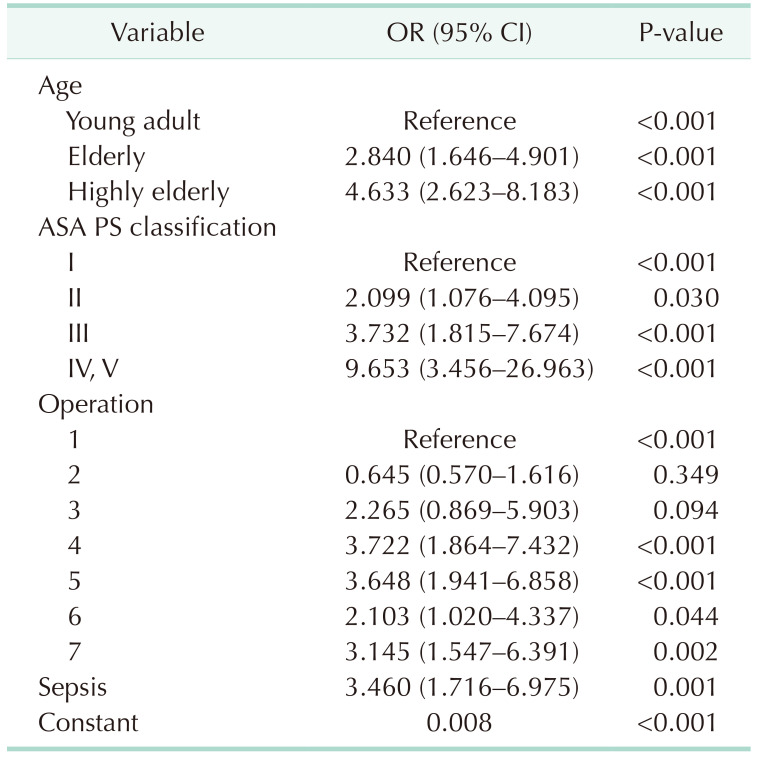
OR, odds ratio; CI, confidence interval; ASA PS, American Society of Anesthesiologists physical status.
Operation 1–7, same as described in Table 1.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download