Abstract
Purpose
We analyzed the timing of inguinal hernia repair in premature infants in the neonatal intensive care unit (NICU) considering recurrence, incarceration, and other complications.
Methods
In this multicenter retrospective review, premature infants (<37 weeks) in the NICU diagnosed with inguinal hernia between 2017 and 2021 were segregated into 2 groups based on the timing of inguinal hernia repair.
Results
Of 149 patients, 109 (73.2%) underwent inguinal hernia repair in the NICU and 40 (26.8%) after discharge. Preoperative incarceration did not differ, but complications with recurrence and postoperative respiratory insufficiency were higher in the NICU group (11.0% vs. 0%, P = 0.029; 22.0% vs. 5.0%, P = 0.01). Multivariate analysis showed that the significant factors affecting recurrence were preoperative ventilator dependence and body weight of <3,000 g at the time of surgery (odds ratio [OR], 16.89; 95% confidence interval [CI], 3.45–82.69; P < 0.01 and OR, 9.97; 95% CI, 1.03–95.92; P = 0.04).
Conclusion
Our results suggest that when premature infants are diagnosed with inguinal hernia in the NICU, inguinal hernia repair after discharge may decrease the odds of recurrence and postoperative respiratory insufficiency. In patients who have difficulty delaying surgery, it is thought that surgery should be performed carefully in a ventilator preoperatively or weighed <3,000 g at the time of surgery.
Inguinal hernia (IH), the most common disease requiring surgery in children, has an incidence of 3%–5% in term infants [1] which is increased by up to 30% in premature infants [2]. Although IH unequivocally requires surgical treatment, the timing of surgery remains controversial [34]. Some authors recommend surgery immediately following diagnosis to avoid significant complications caused by incarceration and testicular atrophy [56], and thus, IH repair (IHR) is performed before discharge from the neonatal intensive care unit (NICU). However, other authors recommend hernia repair after discharge from the NICU, once greater weight is reached and the tissues of the infant are more developed to reduce the possibility of postoperative respiratory insufficiency and reduce the recurrence rate associated with general anesthesia [789].
Therefore, in this study, we analyzed IHR timing, clinical outcomes, and complications in premature infants in the NICU and investigated the predictive factors that affect the outcomes.
We retrospectively reviewed the medical records of pediatric patients who underwent IHR between January 2017 and December 2021 at 6 institutions in Korea. All were tertiary care hospitals, and all surgeries were performed by pediatric surgeons. Only preterm infants born at a gestational age (GA) of less than 37 weeks and diagnosed with IH during NICU hospitalization were included. Surgery was performed either during hospitalization or delayed until after discharge from the NICU. The timing of surgery was at the surgeon’s discretion based on the patient’s medical condition; in the case of delayed surgery, the ultimate timing was decided by each surgeon.
This study was conducted with the approval of our Institutional Review Board (IRB) of Ulsan University Hospital (No. 2202-07-014). It was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature. All procedures performed in the study were in accordance with the ethical standards of the IRB.
We collected data from patient medical records including demographics such as GA, birth weight, sex, age at operation, body weight at operation, comorbidities, and IH laterality. Surgical techniques (open or laparoscopic surgery), operation time, postoperative hospitalization period, incarceration, surgical complications (wound infection, testicular atrophy, secondary high testes, hydrocele, small bowel resection, and recurrence), and postoperative respiratory insufficiency were also investigated and analyzed. Incarceration was defined if it could not be manually reduced.
Postoperative respiratory insufficiency was defined as when a patient was dependent on a mechanical ventilator for more than 4 hours without self-respiration, or desaturation of SpO2 <90% was observed for 10 seconds without respiratory movements in extubated patients [10]. Comorbidities included congenital anomalies, bronchopulmonary dysplasia, intraventricular hemorrhage, necrotizing enterocolitis, and sepsis.
Premature infants were categorized into 2 groups according to time of operation: (1) The NICU group, comprised of patients who underwent surgery while admitted to the NICU, and (2) the delayed group, comprised of patients who underwent surgery after discharge from the NICU.
Statistical analysis was performed using the IBM SPSS Statistics ver. 21.0 (IBM Corp.). Categorical variables were analyzed using the chi-square test and Mann-Whitney U-test. To assess the independent effects of risk factors on the development of recurrence, multivariate logistic regression models were constructed. A 95% confidence interval (CI) was calculated for the regression analysis results. All tests were 2-tailed, and statistical significance was set at P < 0.05.
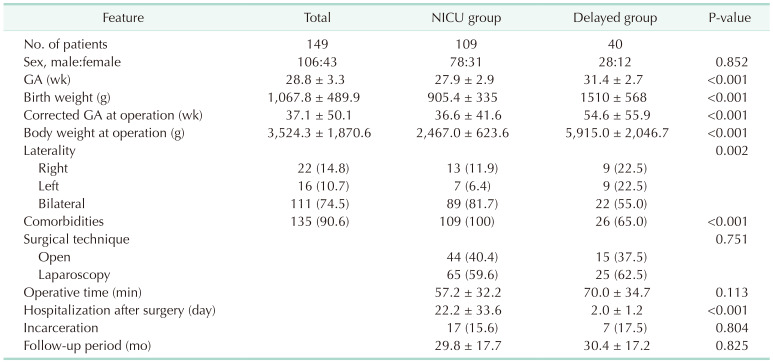
A total of 149 premature infants were included in the study. Table 1 shows patient demographic data and clinical features. The mean GA and birth weight were 28.8 ± 3.3 weeks and 1,067.8 ± 489.9 g, respectively. The corrected age at the time of surgery was 37.1 ± 50.1 weeks, and 90 patients (60.4%) were less than 40 weeks of corrected age.
Of the 149 patients, 109 (73.2%) underwent IHR in the NICU and 40 (26.8%) did so after discharge. The delayed group underwent surgery within an average of 10.7 weeks of discharge from the NICU. Two-group analysis indicated that GA, birth weight, corrected age, and birth weight at operation were lower in the NICU group than in the delayed group (P < 0.001 for each variable); however, the proportion of males did not differ between the 2 groups. The number of patients with bilateral IH was higher in the NICU group (81.7% vs. 55.0%, P = 0.002). All patients who underwent surgery in the NICU had comorbidities, which were significantly higher than those who underwent the surgery after discharge (100% vs. 65.0%, P < 0.001). Incidence of incarceration, surgical techniques such as open or laparoscopy, and time of surgery did not differ between the 2 groups; however, the postoperative hospitalization period was 22.2 ± 33.6 days in the NICU group, significantly longer than the 2 ± 1.2 days in the delayed group (P < 0.001).
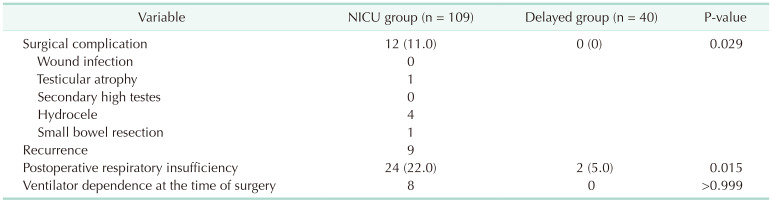
Postoperative complications occurred in the NICU group exclusively (11.0%, P = 0.029), of which recurrence was the highest at 8.3% (Table 2). In addition to recurrence, there was 1 incidence of testicular atrophy (0.9%), 4 hydroceles (3.7%), and 1 small bowl resection (0.9%). No wound infection or secondary high testes occurred. Postoperative respiratory insufficiency occurred more frequently in the NICU group (22.0%, P = 0.015). Among the patients with postoperative respiratory insufficiency in the NICU group, 8 out of 24 patients had ventilator dependence at the time of surgery. There was no statistical significance compared with the delayed group (P > 0.999).
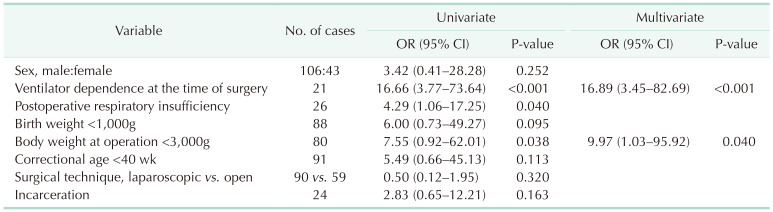
In the logistic regression analysis for risk factors affecting recurrence, we found significant risk factors such as ventilator dependence at the time of surgery, postoperative respiratory insufficiency and body weight of <3,000 g at the of surgery (P < 0.001, P = 0.040, and P = 0.038, respectively) (Table 3). Multivariate analysis confirmed that ventilator dependence and body weight of <3,000 g at the time of surgery were the only significant factors influencing recurrence (P < 0.001 and P = 0.046, respectively).
IH has an incidence of 13% in infants born at <32 weeks GA and up to 30% in infants born weighing less than 1,000 g [211]. Although the procedure is recommended immediately following diagnosis owing to the high possibility of strangulation and incarcerated hernia in infants, this remains controversial. One survey from the American Academy of Pediatrics showed varying results for the time of IHR [4], with 63%–70% of surgeons reporting that they would repair a hernia discovered in an inpatient prior to discharge, while others reporting waiting until the baby’s GA and weight are 50 weeks and 3,000 g or 60 weeks and 3,500 g, respectively. However, the differences in these trends were not significant.
For premature infants diagnosed with IH in the NICU, surgeon concerns regarding early surgery may include surgical difficulty and risk of general anesthesia. In our study, the mean weight of the patients in the NICU group was 2,500 g at operation, which was smaller than that of common full-term newborns. Premature infants have underlying pathologies such as fragile hernia sac and spermatic cord, and their delicate tissue demands a high level of technical skill for the surgeon [12]. A 2019 meta-analysis including 6 comparative studies published by Masoudian et al. [13] showed the recurrence rate of hernia as significantly higher in the early surgery group than in the late surgery group (odds ratio [OR], 4.12; 95% CI, 1.17–14.45). In that study, the number of surgical complications with recurrence was significantly higher in the NICU group (P = 0.029), and in multivariate analysis examining factors affecting recurrence, preoperative ventilator dependence and body weight of <3,000 g at the time of IHR were statistically significant (OR, 16.893; 95% CI, 3.451–82.690 and OR, 9.978; 95% CI, 1.038–95.921). Extreme friability of the hernia sac in premature infants along with a higher number of comorbidities leads to more technically demanding repair and increases the risk of postoperative complications with recurrence.
Surgeons are also concerned about complications related to general anesthesia such as postoperative apnea and bradycardia requiring assisted ventilation, which are more problematic in premature infants. In one study, Iqbal et al. [14] suggested that a body weight <2,500 g and GA <34 weeks were risk factors for ventilation in newborns. Further, another study also found an increased risk of postoperative apnea when GA was <45 weeks [7]. Additionally, cardiovascular complications, neonatal respiratory distress syndrome, and sepsis have been more commonly associated with premature infants [1516]. In our study, similar to those previously published, the delayed group had less postoperative respiratory insufficiency than patients in the NICU group. Patients in the NICU group had 100% comorbidities and 16.5% ventilator dependence at the time of surgery, which was expected to increase postoperative respiratory insufficiency. In particular, bronchopulmonary dysplasia accounted for 63 of 109 (57.8%) and 9 of 40 (22.5%) in the NICU and delayed groups, respectively. Considering these points, some surgeons recommend waiting until the appropriate weight, age, and respiratory status have been reached before performing surgery [91718].
Although rates of delayed IHR are gradually increasing, pediatric surgeons still prefer IHR to be performed on premature infants before discharge from the NICU whenever medically feasible. Concern regarding incarceration is the primary motivation for performing IHR as soon as possible after diagnosis. Vaos et al. [6] reported a higher rate of incarceration with delayed IHR in premature neonates (12% vs. 56%), and Zamakhshary et al. [19] reported similar outcomes in patients under 2 years. Furthermore, Uemura et al. [20] suggested that delayed IHR induces adhesion of the thickened hernia sac and spermatic cord, making later dissection difficult. They reported prolonged operative time, increased risk of damage to testicular vessels, and subsequent testicular atrophy in delayed IHR. In our study, the incidence of incarceration was not significantly different between the 2 groups (P = 0.804) and was comparable to the range of 11.5%–35% found in other studies [21222324]. However, the incidence of incarceration was 15.6% and 17.6% in the 2 groups, respectively, and thus this remains a point to always be vigilant of preceding surgery.
This study was a retrospective review and thus has some limitations. The data collected were not explicitly included in the study and were therefore subject to the biases inherent in such methodology. Further, although this was a multicenter study, the sample size may have been smaller than that in several previous investigations of pediatric IHR. The purpose of this was to identify the undated surgical trend over the last 5 years, but with this comes a potential for type-II error. A longer follow-up time into later childhood or even adulthood is required to confirm the occurrence of metachronous IH and recurrence. However, we used an average of 31.8 weeks after surgery, which may have been too short of a period to provide a full picture of recurrence.
This study suggested that when premature infants are diagnosed with IH in the NICU, receiving IHR after discharge may decrease the odds of recurrence and postoperative respiratory insufficiency. When premature NICU infants undergo IHR, it is recommended that those with a presurgical ventilator or weight less than 3,000 g at the time of surgery are operated on with caution regarding complications, including recurrence.
References
1. Pastore V, Bartoli F. Neonatal laparoscopic inguinal hernia repair: a 3-year experience. Hernia. 2015; 19:611–615. PMID: 24889274.
2. González Santacruz M, Mira Navarro J, Encinas Goenechea A, García Ceballos A, Sánchez Zaplana H, Jiménez Cobo B. Low prevalence of complications of delayed herniotomy in the extremely premature infant. Acta Paediatr. 2004; 93:94–98. PMID: 14989447.
3. Pini Prato A, Rossi V, Mosconi M, Disma N, Mameli L, Montobbio G, et al. Inguinal hernia in neonates and ex-preterm: complications, timing and need for routine contralateral exploration. Pediatr Surg Int. 2015; 31:131–136. PMID: 25381589.
4. Antonoff MB, Kreykes NS, Saltzman DA, Acton RD. American academy of pediatrics section on surgery hernia survey revisited. J Pediatr Surg. 2005; 40:1009–1014. PMID: 15991187.
5. Fu YW, Pan ML, Hsu YJ, Chin TW. A nationwide survey of incidence rates and risk factors of inguinal hernia in preterm children. Pediatr Surg Int. 2018; 34:91–95. PMID: 29230549.
6. Vaos G, Gardikis S, Kambouri K, Sigalas I, Kourakis G, Petoussis G. Optimal timing for repair of an inguinal hernia in premature infants. Pediatr Surg Int. 2010; 26:379–385. PMID: 20169441.
7. Ozdemir T, Arıkan A. Postoperative apnea after inguinal hernia repair in formerly premature infants: impacts of gestational age, postconceptional age and comorbidities. Pediatr Surg Int. 2013; 29:801–804. PMID: 23780479.
8. Maillet OP, Garnier S, Dadure C, Bringuier S, Podevin G, Arnaud A, et al. Inguinal hernia in premature boys: should we systematically explore the contralateral side? J Pediatr Surg. 2014; 49:1419–1423. PMID: 25148751.
9. Youn JK, Kim HY, Huh YJ, Han JW, Kim SH, Oh C, et al. Inguinal hernia in preterms in neonatal intensive care units: optimal timing of herniorrhaphy and necessity of contralateral exploration in unilateral presentation. J Pediatr Surg. 2018; 53:2155–2159. PMID: 29628207.
10. Silins V, Julien F, Brasher C, Nivoche Y, Mantz J, Dahmani S. Predictive factors of PACU stay after herniorraphy in infant: a classification and regression tree analysis. Paediatr Anaesth. 2012; 22:230–238. PMID: 22098252.
11. Peevy KJ, Speed FA, Hoff CJ. Epidemiology of inguinal hernia in preterm neonates. Pediatrics. 1986; 77:246–247. PMID: 3753760.
12. Baird R, Gholoum S, Laberge JM, Puligandla P. Prematurity, not age at operation or incarceration, impacts complication rates of inguinal hernia repair. J Pediatr Surg. 2011; 46:908–911. PMID: 21616251.
13. Masoudian P, Sullivan KJ, Mohamed H, Nasr A. Optimal timing for inguinal hernia repair in premature infants: a systematic review and meta-analysis. J Pediatr Surg. 2019; 54:1539–1545. PMID: 30541673.
14. Iqbal Q, Younus MM, Ahmed A, Ahmad I, Iqbal J, Charoo BA, et al. Neonatal mechanical ventilation: indications and outcome. Indian J Crit Care Med. 2015; 19:523–527. PMID: 26430338.
15. Steward DJ. Preterm infants are more prone to compl icat ions following minor surgery than are term infants. Anesthesiology. 1982; 56:304–306. PMID: 7065438.
16. Mayhew JF, Bourke DL, Guinee WS. Evaluation of the premature infant at risk for postoperative complications. Can J Anaesth. 1987; 34:627–631. PMID: 3677290.
17. Rescorla FJ, Grosfeld JL. Inguinal hernia repair in the perinatal period and early infancy: clinical considerations. J Pediatr Surg. 1984; 19:832–837. PMID: 6520682.
18. Lee SL, Gleason JM, Sydorak RM. A critical review of premature infants with inguinal hernias: optimal timing of repair, incarceration risk, and postoperative apnea. J Pediatr Surg. 2011; 46:217–220. PMID: 21238671.
19. Zamakhshary M, To T, Guan J, Langer JC. Risk of incarceration of inguinal hernia among infants and young children awaiting elective surgery. CMAJ. 2008; 179:1001–1005. PMID: 18981440.
20. Uemura S, Woodward AA, Amerena R, Drew J. Early repair of inguinal hernia in premature babies. Pediatr Surg Int. 1999; 15:36–39. PMID: 9914352.
21. Lautz TB, Raval MV, Reynolds M. Does timing matter? A national perspective on the risk of incarceration in premature neonates with inguinal hernia. J Pediatr. 2011; 158:573–577. PMID: 21035818.
22. Abdulhai SA, Glenn IC, Ponsky TA. Incarcerated pediatric hernias. Surg Clin North Am. 2017; 97:129–145. PMID: 27894423.
23. Stylianos S, Jacir NN, Harris BH. Incarceration of inguinal hernia in infants prior to elective repair. J Pediatr Surg. 1993; 28:582–583. PMID: 8483072.
24. Hughes K, Horwood JF, Clements C, Leyland D, Corbett HJ. Complications of inguinal herniotomy are comparable in term and premature infants. Hernia. 2016; 20:565–569. PMID: 26749021.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download