Abstract
Purpose
The present study aimed to examine the characteristics, outcomes, and problems related to surgery for acute abdomen in adult patients with severe motor and intellectual disabilities (MID).
Methods
The clinical records of 35 adult patients with severe MID who received emergency surgery for acute abdomen between 2011 and 2020 were reviewed.
Results
The median duration from onset to surgery was 48 hours. There were 2 cases of in-hospital mortality (5.7%), and all the patients underwent surgery more than 72 hours after onset. The in-hospital mortality rate was significantly higher in patients who received surgery later than 72 hours after onset. Bowel obstruction was the most common disease among the acute abdomen cases (71.4%) and most often involved volvulus of the small bowel and cecum. Of the patients with bowel obstruction with severe MID, 72.0% had abdominal distention, 16.0% had abdominal pain, and 4.0% had vomiting. The median duration from onset to surgery was significantly longer in the patients with bowel obstruction with severe MID than in those without severe MID (24 hours vs. 16 hours).
Acute abdomen is a medical emergency characterized by sudden and severe pain in the abdomen of recent onset with accompanying signs and symptoms of abdominal involvement. Clinical history-taking, clinical symptoms, and laboratory and imaging findings are important for its diagnosis and the decision as to whether or not to operate. However, patients with severe motor and intellectual disabilities (MID) are more susceptible to delayed diagnosis and adverse surgical outcomes owing to impaired communication, variable responses to the symptoms and drugs, physiological anomalies, and skeletal deformities than patients without severe MID. However, only several, previous reports have examined the perioperative outcomes of acute abdomen in patients with intellectual disabilities [12]. The present study aimed to examine the characteristics, perioperative outcomes, and surgical issues related to the acute abdomen in adult patients with severe MID.
The present, monocentric, retrospective study included adult patients with severe MID undergoing emergency surgery for acute abdomen between January 1, 2011 and December 31, 2020 at Tokyo Metropolitan Tama Medical Center and was approved by the Institutional Review Board of Tokyo Metropolitan Tama Medical Center (No. 4-34). This study was performed in accordance with the Declaration of Helsinki and written informed consent was obtained from all the patients.
Patients with severe MID aged 18 years or older were selected according to the following criteria: (1) severe or profound intellectual disability with an estimated intelligence quotient <35; (2) profound motor disability (unable to move independently); and (3) sensory function impairment (visual and/or auditory) [34]. To assess the clinical features of these patients, patient records were reviewed for the patient characteristics, including age, sex, body mass index (BMI), background disease, symptoms, vital signs on arrival, duration from onset to surgery (onset was defined as the point at which the caregiver noticed a change in the patient’s physical condition), operative diagnosis, surgery type, and postoperative outcomes, including postoperative complications, length of intensive care unit (ICU) stay, hospital stay, and in-hospital mortality.
In addition, patients with acute abdomen with an intraoperative diagnosis of bowel obstruction were extracted for analysis. As a comparison group, adult patients without severe MID undergoing emergency surgery for bowel obstruction during the same period at our institution were identified, and their characteristics, symptoms, duration from onset to surgery, operative diagnosis, and postoperative outcomes were reviewed. Cases of bowel obstruction caused by a neoplasm were excluded. None of the patients with bowel obstruction with severe MID had bowel obstruction caused by a neoplasm.
Categorical variables were compared using the chi-square or Fisher exact test, and continuous variables were compared using the Student t-test. The P-value of <0.05 was considered to indicate statistical significance. All statistical analyses were performed using IBM SPSS Statistics ver. 26 (IBM Corp.).
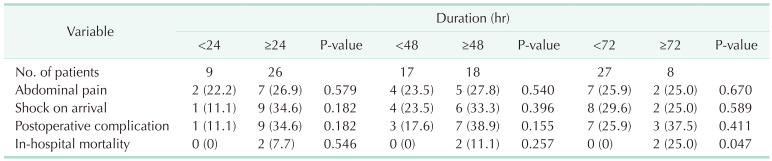
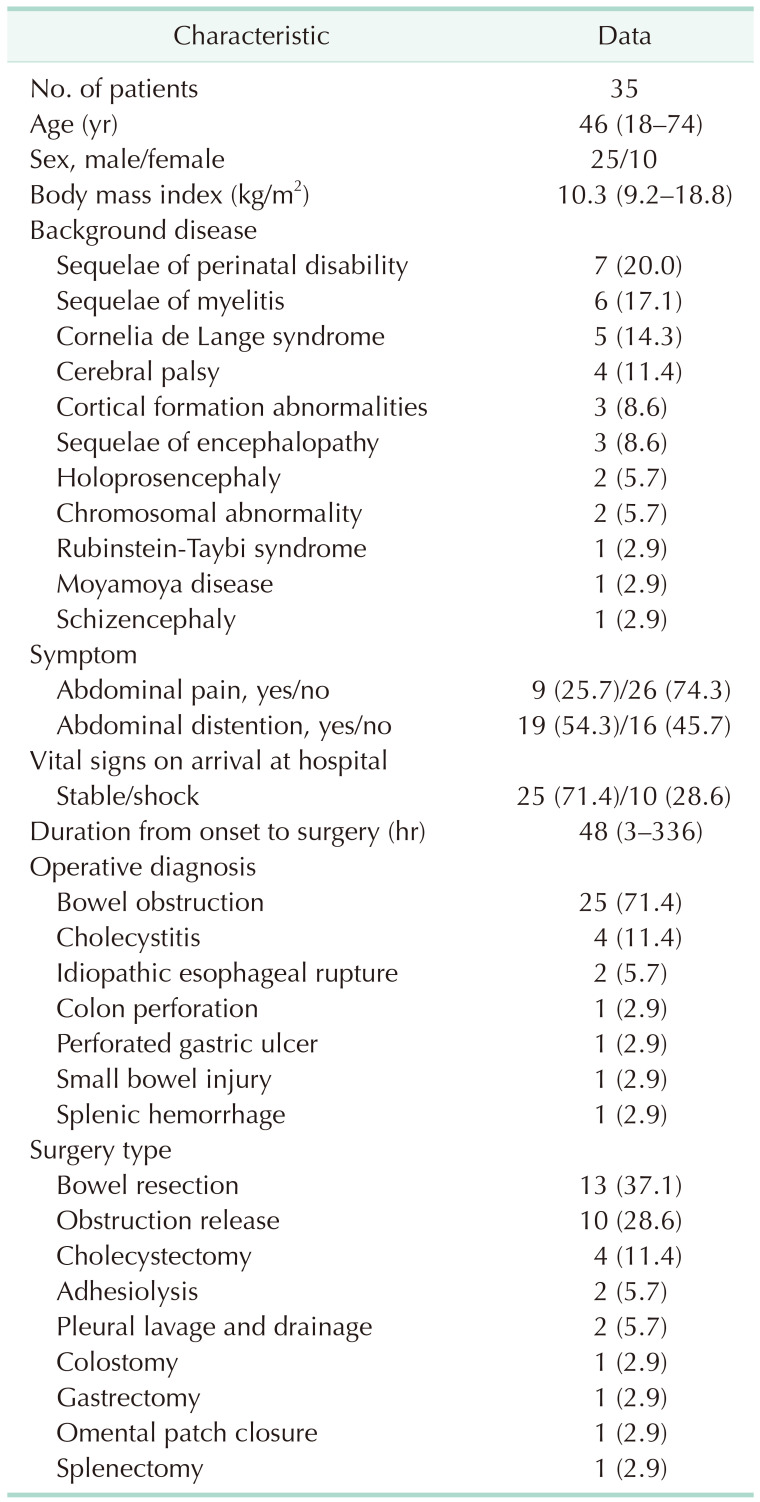
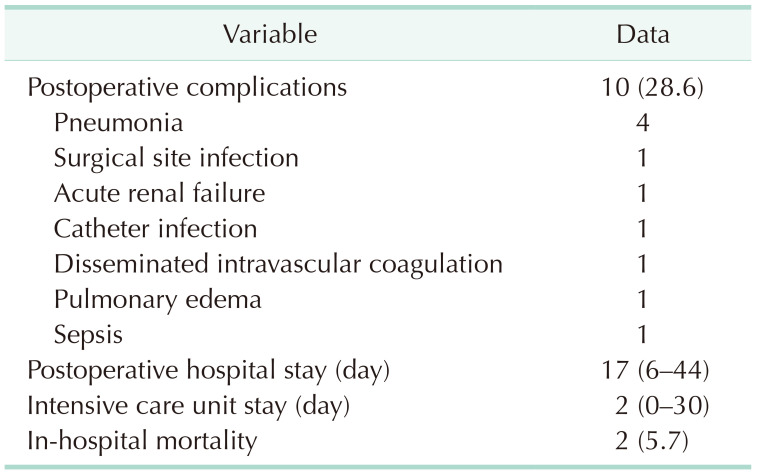
Fig. 1 shows a flow chart of the present study. During the study period, 35 adult patients with severe MID received emergency surgery for the acute abdomen. Table 1 shows the clinical characteristics of the patients; 25 were male, and 10 were female, and the median age was 46 years (range, 18–74 years). The median BMI was 10.3 kg/m2 (range, 9.2–18.8 kg/m2). The patients had the following background diseases: sequelae of perinatal disability (n = 7), sequelae of myelitis (n = 6), Cornelia de Lange syndrome (n = 5), cerebral palsy (n = 4), cortical formation abnormalities (n = 3), sequelae of encephalopathy (n = 3), holoprosencephaly (n = 2), chromosomal abnormality (n = 2), Rubinstein-Taybi syndrome (n = 1), Moyamoya disease (n = 1), and schizencephaly (n = 1). Nine patients (25.7%) had abdominal pain, a typical symptom of acute abdomen, and 26 patients (74.3%) denied abdominal pain. Abdominal distension was the most common symptom (19 cases, 54.3%). On arrival at our hospital, 25 patients (71.4%) had stable vital signs, but 10 patients (28.6%) presented with shock. Abdominal CT corroborated the diagnosis and identified the cause of acute abdomen in all the patients preoperatively. The median duration from onset to surgery was 48 hours (range, 3–336 hours). Bowel obstruction was the most common, intraoperatively diagnosed disease (n = 25, 71.4%), followed by cholecystitis at 11.4% (n = 4), idiopathic esophageal rupture at 5.7% (n = 2), and colon perforation, perforated gastric ulcer, small bowel injury, and splenic hemorrhage, each at 2.9% (n = 1). The types of surgery were as follows: bowel resection for bowel obstruction and small bowel injury (n = 13), obstruction release for bowel obstruction (n = 10), cholecystectomy for cholecystitis (n = 4), adhesiolysis for bowel obstruction (n = 2), pleural lavage and drainage for idiopathic esophageal rupture (n = 2), colostomy for colon perforation (n = 1), gastrectomy for gastric volvulus (n = 1), omental patch closure for perforated gastric ulcer (n = 1), and splenectomy for splenic hemorrhage (n = 1). Table 2 shows the postoperative outcomes. The rate of postoperative complications was 28.6%. Pneumonia was the most common complication (40.0%). The median postoperative hospital stay was 17 days (range, 6–44 days), and the median ICU stay was 2 days (range, 0–30 days). The in-hospital mortality rate was 5.7% (2 cases). Both patients who died underwent surgery more than 72 hours after onset and were already in shock on arrival at the hospital. One patient had ileus caused by fecal impaction and died of sepsis from bacterial translocation, and the other patient had an internal hernia and died of pulmonary edema. Table 3 shows the relationship between adverse events in patients who underwent surgery within 24 hours of, or 48 or 72 hours after, onset. When durations up to 24 hours and 48 hours from onset to surgery were compared, no significant difference was found in the rate of abdominal pain, shock on arrival, postoperative complications, or the in-hospital mortality rate. On the other hand, the in-hospital mortality rate was significantly higher in patients who received surgery more than 72 hours after onset.
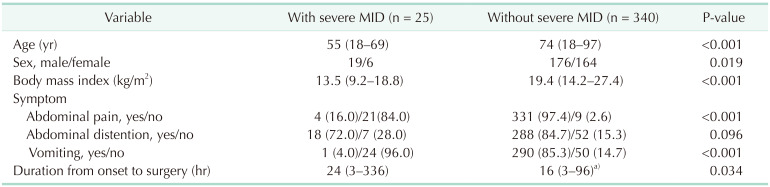
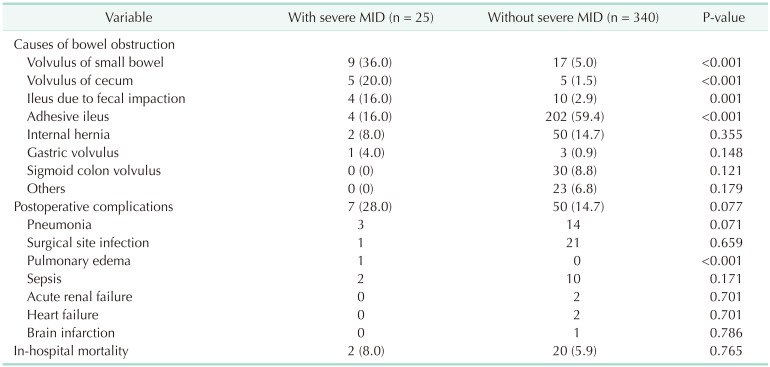
To examine the detailed characteristics of bowel obstruction in patients with severe MID, only the patients with acute abdomen caused by a bowel obstruction (n = 25) were extracted from the entire cohort of patients with severe MID with acute abdomen (n = 35). For comparison, 340 patients without severe MID receiving surgery for bowel obstruction during the same period (January 1, 2011 to December 31, 2020) were analyzed (Fig. 1). Table 4 shows the comparison of the clinical characteristics of patients with and without severe MID who had acute abdomen caused by a bowel obstruction. Compared with the patients without severe MID, the patients with severe MID were younger and had a lower BMI. Of the patients with severe MID, 18 (72.0%) had abdominal distension, 4 (16.0%) had abdominal pain, and 1 (4.0%) had vomiting. Of those without severe MID, 331 (97.4%) had abdominal pain, 288 (84.7%) had abdominal distension, and 290 (85.3%) had vomiting. The precise duration from onset to surgery was recorded in the medical records of 133 of the 340 patients without severe MID. The median duration was significantly longer in the patients with severe MID (24 hours vs. 16 hours). Table 5 shows the causes of bowel obstruction and postoperative outcomes in the 2 groups. Among the patients with severe MID, 9 (36.0%) had volvulus of the small bowel, 5 (20.0%) had volvulus of the cecum, and 4 (16.0%) had ileus caused by fecal impaction. On the other hand, the most common cause of bowel obstruction in the patients without severe MID was adhesive ileus (59.4%) followed by internal hernia (14.7%). Seventeen patients (5.0%) had volvulus of the small bowel, 10 patients (2.9%) had ileus caused by fecal impaction, and 5 patients (1.5%) had volvulus of the cecum. Volvulus of the small bowel and cecum and ileus caused by fecal impaction were more common while adhesive ileus was significantly less common in the patients with severe MID than in those without severe MID. The rate of bowel resection was 52.0% and 59.1% for the respective group. No significant difference was found between the groups. The postoperative complication rate was 28.0% and 14.7% in the patients with and without severe MID, respectively. Pneumonia and surgical site infection was the most common complication in the patients with and without severe MID, respectively. The incidence of total postoperative complications and pneumonia was more common in patients with severe MID, but no significant difference was found between the groups. The in-hospital mortality rate was 8.0% and 5.9% for the respective group, with no significant difference found between the groups.
The present study examined 2 topics: one concerned the clinical characteristics and postoperative outcomes in all the patients with severe MID with acute abdomen; the second concerned the clinical characteristics and postoperative outcomes in patients with severe MID with acute abdomen caused by a bowel obstruction.
Of the entire cohort of patients with severe MID with acute abdomen, 28.6% were already in shock on arrival at the hospital, and the median duration from onset to surgery was as long as 48 hours. Patients with severe MID may have difficulty accurately describing the severity of their subjective symptoms, and medical staff often have difficulty examining the patients because of skeletal deformities and their variable responses to the symptoms. In our study, abdominal pain, a typical symptom of acute abdomen, occurred in only 25.7% of the patients, and abdominal distension was the most common symptom. Many patients with MID experience constant abdominal distension caused by aerophagia, chronic constipation, or medications affecting the gastrointestinal tract. These factors contribute to the difficulties and delays in diagnosing the condition. For early diagnosis and treatment, caregivers should be trained to recognize signs of distress in their charges, seek immediate medical care, and not hesitate to consult a physician when in doubt. It is also important that medical staff watch for symptoms and signs by performing a careful physical examination especially because these signs and symptoms may be more subtle or less recognizable in patients with MID than in other patients [5]. In our study, the postoperative complication rate was 28.6%, and the in-hospital mortality rate was 5.7%. Khalid and Al-Salamah [1] reported a morbidity rate of 33% and a mortality rate of 23% in surgical patients with acute abdomen with intellectual disabilities. Lin et al. [6] reported that surgical patients with intellectual disabilities had a higher risk of postoperative acute renal failure, pneumonia, bleeding, sepsis, and overall complications. The most common complication in our patients was pneumonia (40%), in line with the findings of a previous report [1]. The risk of pneumonia is substantially higher in patients with MID owing to multiple factors, including poor oral hygiene, gastroesophageal reflex, a dysfunctional pharyngoesophageal sphincter, and anticonvulsants and/or tranquilizers causing hypersalivation [6]. To prevent pneumonia, close attention should be paid to the possibility of its postoperative occurrence, along with perioperative antibiotic coverage, postoperative respiratory rehabilitation, and oral and pulmonary hygiene. Acute renal failure is an important complication although it occurred in only 1 patient in the present study [6]. Patients with intellectual disability often have renal dysfunction accompanying polycystic kidney, and some intellectual disabilities related to syndromes, such as Bardet-Biedl syndrome and Williams-Beuren syndrome, are associated with renal dysfunction. Patients with these conditions show progression to renal failure early in life [789] and therefore should be observed carefully for indications of progression of acute renal failure caused by the stress or invasiveness of surgery. In-hospital mortality was significantly higher in the patients who underwent surgery more than 72 hours after onset than in those who underwent surgery within 71 hours of onset although the rate of other adverse events did not differ in terms of the duration from onset to surgery. This result might be explained by delays in diagnosis and treatment, underscoring the importance of early diagnosis and treatment for improved, postoperative outcomes.
In the present study, in patients with severe MID with acute abdomen, bowel obstruction was the most common cause of acute abdomen (25 of 35 patients, 71.4%). In previous reports, bowel obstruction was the main cause of acute abdomen with MID as well as our study [12]. Jancar and Speller [10] reported a higher incidence and lower mean age at death in patients with an intellectual disability with a fatal bowel obstruction than in the total national population, and chronic constipation, megacolon, and lower intellectual functioning were identified as risk factors of fatal bowel obstruction. In the present study, almost all the patients without severe MID had abdominal pain, distension, and vomiting, which are typical symptoms of bowel obstruction. On the other hand, of the patients with severe MID only 16.0% and 4.0% had abdominal pain and vomiting, respectively, and the median duration from onset to surgery was significantly longer than in the patients without severe MID. Because abdominal pain and vomiting do not commonly occur in severe MID with bowel obstruction, it is important for the caregiver to be vigilant for any signs of abdominal distension to enable early diagnosis of the condition. Previous reports described the predictive factors of bowel obstruction requiring surgery in patients with severe MID which might be useful for diagnosing bowel obstruction at an early stage and determining if surgery is indicated [11]. In general, the causes of bowel obstruction in descending order of frequency are adhesion (60% to 75%), neoplasms (13% to 20%), herniation (2% to 15%), and volvulus (<5%) [12]. In the patients with severe MID in the present study, the major causes of bowel obstruction were volvulus of the small bowel and cecum and ileus caused by fecal impaction. On the other hand, the most common cause of bowel obstruction in patients without severe MID was adhesive ileus. It is notable that volvulus of the cecum, which accounted for 20% of bowel obstruction cases in patients with severe MID, is extremely rare in healthy individuals, accounting for fewer than 1% of all bowel obstruction cases. It is caused by abnormal mobility of the cecum stemming from anomalous developmental fusion of the cecum and ascending colon mesentery with the retroperitoneum and occurs commonly in association with MID, Cornelia de Lange syndrome, or lissencephaly [131415]. In patients with severe MID, ileus due to fecal impaction accounted for 16% of the cases and was rare in patients without severe MID (2.9%). Chronic constipation in patients with severe MID is a risk factor for ileus due to fecal impaction. In our study, the rate of bowel resection, postoperative complications, and in-hospital mortality associated with bowel obstruction did not differ significantly between the groups, possibly owing to the small sample pool. Our study found no case of intestinal obstruction caused by pica, which is a craving for, or ingestion of, non-food items often observed in people with developmental disabilities [1617]. Pica should therefore be suspected if a patient presents with a bowel obstruction of unknown etiology.
Our study had several limitations. It was monocentric, retrospective, and lacked postdischarge follow-up data. Data on the patients’ caregivers and living environment were unavailable although they may be important factors in the duration from onset to surgery. The cases of acute abdomen with severe MID for which surgery was not performed (including cases in which family or caregiver declined treatment) or which were treated with conservative therapy were excluded. While the present study excluded patients receiving only conservative therapy, some patients presumably respond well to conservative therapy alone without surgery. Unfortunately, including these patients in the present study was not possible owing to the lack of a database of patients with severe MID without surgery at the study center. A future study should analyze such patients to shed more light on the relationship between adverse events and duration from onset to surgery exceeding 72 hours. Further, information about the duration from onset to surgery was unavailable for all the cases of bowel obstruction without severe MID. Future studies on this topic should enroll more cases from multiple centers.
In conclusion, acute abdomen in patients with severe MID often stemmed from a bowel obstruction caused by volvulus. Because the patients with severe MID had few symptoms, they were susceptible to adverse surgical outcomes associated with a prolonged duration from onset to surgery.
References
1. Khalid K, Al-Salamah SM. Surgery for acute abdominal conditions in intellectually-disabled adults. ANZ J Surg. 2006; 76:145–148. PMID: 16626354.
2. Voitk AJ. Acute abdomen in severely mentally retarded patients. Can J Surg. 1987; 30:195–196. PMID: 3580979.
3. Nakken H, Vlaskamp C. A need for a taxonomy for profound intellectual and multiple disabilities. J Policy Pract Intellect Disabil. 2007; 4:83–87.
4. van Timmeren EA, van der Putten AA, van Schrojenstein Lantman-de Valk HM, van der Schans CP, Waninge A. Prevalence of reported physical health problems in eople with severe or profound intellectual and motor disabilities: a cross-sectional study of medical records and care plans. J Intellect Disabil Res. 2016; 60:1109–1118. PMID: 27197564.
5. Cvetković D, Živković V, Damjanjuk I, Nikolić S. Intestinal obstruction as a cause of death in the mentally disabled. Forensic Sci Med Pathol. 2019; 15:136–139. PMID: 30076536.
6. Lin JA, Liao CC, Chang CC, Chang H, Chen TL. Postoperative adverse outcomes in intellectually disabled surgical patients: a nationwide population-based study. PLoS One. 2011; 6:e26977. PMID: 22046425.
7. Seeman T, Malíková M, Bláhová K, Seemanová E. Polycystic kidney and hepatic disease with mental retardation and hand anomalies in three siblings. Pediatr Nephrol. 2009; 24:1409–1412. PMID: 19011905.
8. Green JS, Parfrey PS, Harnett JD, Farid NR, Cramer BC, Johnson G, et al. The cardinal manifestations of Bardet-Biedl syndrome, a form of Laurence-Moon-Biedl syndrome. N Engl J Med. 1989; 321:1002–1009. PMID: 2779627.
9. Biesecker LG, Laxova R, Friedman A. Renal insufficiency in Williams syndrome. Am J Med Genet. 1987; 28:131–135. PMID: 3314505.
10. Jancar J, Speller CJ. Fatal intestinal obstruction in the mentally handicapped. J Intellect Disabil Res. 1994; 38(Pt 4):413–422. PMID: 7949792.
11. Eren T, Boluk S, Bayraktar B, Ozemir IA, Yildirim Boluk S, Tombalak E, et al. Surgical indicators for the operative treatment of acute mechanical intestinal obstruction due to adhesions. Ann Surg Treat Res. 2015; 88:325–333. PMID: 26029678.
12. Jackson P, Vigiola Cruz M. Intestinal obstruction: evaluation and management. Am Fam Physician. 2018; 98:362–367. PMID: 30215917.
13. Hasbahceci M, Basak F, Alimoglu O. Cecal volvulus. Indian J Surg. 2012; 74:476–479. PMID: 24293902.
14. Masumoto K, Izaki T, Arima T. Cornelia de Lange syndrome associated with cecal volvulus: report of a case. Acta Paediatr. 2001; 90:701–703. PMID: 11440107.
15. Lee EK, Kim JE, Lee YY, Kim S, Choi KH. A case of cecal volvulus presenting with chronic constipation in lissencephaly. Pediatr Gastroenterol Hepatol Nutr. 2013; 16:131–134. PMID: 24010118.
16. Feldman MD. Pica: current perspectives. Psychosomatics. 1986; 27:519–523. PMID: 3526382.
17. Tokue H, Takahashi Y, Hirasawa S, Awata S, Kobayashi S, Shimada T, et al. Intestinal obstruction in a mentally retarded patient due to pica. Ann Gen Psychiatry. 2015; 14:22. PMID: 26236386.
Table 3
Relationship between adverse events and duration from onset to surgery within 24 hours and after 48 and 72 hours




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download